Abstract
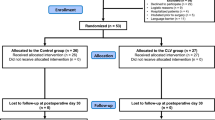
Closed-loop feedback computer-controlled vasopressor infusion has been previously described for maintaining blood pressure during spinal anaesthesia for caesarean section but there are limited data available comparing the relative performance of different vasopressors. The aim of this study was to compare the performance of norepinephrine versus phenylephrine in this system. Data from a randomized, two-arm parallel group, double-blinded controlled trial were reanalyzed. 104 patients scheduled for elective caesarean section under spinal anaesthesia were randomized to receive computer-controlled closed-loop infusion of either norepinephrine 5 µg ml−1 or phenylephrine 100 µg ml−1. This was started immediately after induction of spinal anaesthesia and used an algorithm designed to maintain systolic blood pressure near baseline until fetal delivery. Performance error calculations were used to compare the performance of the two vasopressors. The primary outcome was defined as the median absolute performance error. Median performance error, wobble and divergence were also compared. Median absolute performance error was smaller in the norepinephrine group (median 3.79 [interquartile range 2.82–5.17] %) versus the phenylephrine group (4.70 [3.23–6.57] %, P = 0.028). In addition, median performance error was smaller (0.75 [−1.56–2.52] %) versus 2.61 [0.83–4.57] %, P = 0.002) and wobble was smaller (2.85 [2.07–5.17] %) versus 3.39 [2.62–4.90] %, P = 0.028) in the norepinephrine group versus the phenylephrine group. Divergence was similar between groups. The precision of the control of blood pressure was greater with norepinephrine compared with phenylephrine at the drug concentrations used.


Similar content being viewed by others
References
Ngan Kee WD, Tam YH, Khaw KS, Ng FF, Critchley LA, Karmakar MK. Closed-loop feedback computer-controlled infusion of phenylephrine for maintaining blood pressure during spinal anaesthesia for caesarean section: a preliminary descriptive study. Anaesthesia. 2007;62:1251–6.
Ngan Kee WD, Khaw KS, Ng FF, Tam YH. Randomized comparison of closed-loop feedback computer-controlled with manual-controlled infusion of phenylephrine for maintaining arterial pressure during spinal anaesthesia for Caesarean delivery. Br J Anaesth. 2012;110:59–65.
Varvel JR, Donoho DL, Shafer SL. Measuring the predictive performance of computer-controlled infusion pumps. J Pharmacokinet Biopharm. 1992;20:63–94.
Ngan Kee WD, Khaw KS. Vasopressors in obstetrics: what should we be using? Curr Opin Anaesthesiol. 2006;19:238–43.
Ngan Kee WD, Lee SW, Ng FF, Tan PE, Khaw KS. Randomized double-blinded comparison of norepinephrine and phenylephrine for maintenance of blood pressure during spinal anesthesia for cesarean delivery. Anesthesiology. 2015;122:736–45.
Spilker B. Comparison of the inotropic response to glucagon, ouabain and noradrenaline. Br J Pharmacol. 1970;40:382–95.
Benedict CR, Fillenz M, Stanford C. Changes in plasma noradrenaline concentration as a measure of release rate. Br J Pharmacol. 1978;64:305–9.
Hoyme M, Scheungraber C, Reinhart K, Schummer W. Comparison of norepinephrine and cafedrine/theodrenaline regimens for maintaining maternal blood pressure during spinal anaesthesia for caesarean section a two years analysis. Obstet Gynecol: Int J. 2015. doi:10.5171/2015.714966.
Siriussawakul A, Triyasunant N, Nimmannit A, Ngerncham S, Hirunkanokpan P, Luang-Aram S, Pechpaisit N, Wangdee A, Ruangvutilert P. Effects of supplemental oxygen on maternal and neonatal oxygenation in elective cesarean section under spinal anesthesia: a randomized controlled trial. Biomed Res Int. 2014. doi:10.1155/2014/627028.
Carvalho B, Dyer RA. Norepinephrine for spinal hypotension during cesarean delivery: another paradigm shift? Anesthesiology. 2015;122:728–30.
Ngan Kee WD, Khaw KS, Ng FF, Lee BB. Prophylactic phenylephrine infusion for the prevention of hypotension during spinal anesthesia for cesarean delivery. Anesth Analg. 2004;98:815–21.
Ngan Kee WD. Phenylephrine infusions for maintaining blood pressure during spinal anesthesia for cesarean delivery: finding the shoe that fits. Anesth Analg. 2014;118:496–8.
Stewart A, Fernando R, McDonald S, Hignett R, Jones T, Columb M. The dose-dependent effects of phenylephrine for elective cesarean delivery under spinal anesthesia. Anesth Analg. 2010;111:1230–7.
Ngan Kee WD, Khaw KS, Ng FF. Comparison of phenylephrine infusion regimens for maintaining maternal blood pressure during spinal anaesthesia for Caesarean section. Br J Anaesth. 2004;92:469–74.
Burns SM, Cowan CM, Wilkes RG. Prevention and management of hypotension during spinal anaesthesia for elective caesarean section: a survey of practice. Anaesthesia. 2001;56:794–8.
http://www.drugs.com/pro/levophed.html. Accessed 6 January 2016.
Loubani OM, Green RS. A systematic review of extravasation and local tissue injury from administration of vasopressors through peripheral intravenous catheters and central venous catheters. J Crit Care. 2015;30:653.e9–17.
Acknowledgments
The work described in this paper was substantially supported by a grant from the Research Grants Council of the Hong Kong Special Administrative Region, China, Project No. 472112. Previously presented in part as an oral free paper at Obstetric Anaesthesia 2014, Dublin, Ireland, 23 May 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Appendix: Derivation of performance error calculations
Appendix: Derivation of performance error calculations
1.1 Performance error (PE)
PE was defined as the difference between each measured value of systolic blood pressure (SBP) and the baseline value, expressed as a percentage of the baseline value. For each patient until the time of uterine incision, it was calculated as follows:
where PEij is the percentage performance error for the ith patient at the jth minute, meaSBPij is the measured SBP for the ith patient at the jth minute and tarSBPi is the target SBP (set-point for the closed-loop system) for the ith patient.
1.2 Median performance error (MDPE)
MDPE is a measure of bias and describes whether the measured values for SBP are systematically either above or below the baseline value. For each patient, it was defined as the median of all values of PE and was calculated as follows:
where MDPEi is the median performance error for the ith patient and Ni is the number of values for PE obtained for the ith patient.
1.3 Median absolute performance error (MDAPE)
MDAPE is a measure of inaccuracy and represents an average of the magnitudes of the differences of measured values for SBP above or below the baseline value. For each patient, it was defined as the median of the absolute values of PE (|PE|) and was calculated as follows:
where MDPEi is the median absolute performance error for the ith patient.
1.4 Wobble
Wobble is a measure of the intrasubject variability of PE about MDPE. It was calculated as follows:
where WOBBLEi is the wobble for the ith patient.
1.5 Divergence
Divergence describes the trend of changes in |PE| with time and is a measure of whether the magnitudes of the differences between measured and target values for SBP increase (positive value for divergence) or decrease (negative value for divergence) with time. It was defined for each patient as the slope of the linear regression equation of the values of |PEij| for that patient against time. It was calculated as follows:
where DIVERGENCEi is the divergence for the ith patient and T is time in minutes.
Rights and permissions
About this article
Cite this article
Ngan Kee, W.D., Khaw, K.S., Tam, YH. et al. Performance of a closed-loop feedback computer-controlled infusion system for maintaining blood pressure during spinal anaesthesia for caesarean section: a randomized controlled comparison of norepinephrine versus phenylephrine. J Clin Monit Comput 31, 617–623 (2017). https://doi.org/10.1007/s10877-016-9883-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-016-9883-z