Abstract
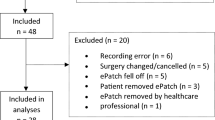
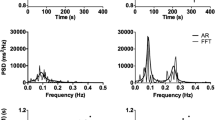
Heart rate volatility (HRVO) is hypothesized to be a physiological measure of sympathetic activity and is defined by the standard deviation (SD) of the heart rate (HR) in beats per minutes (BPM) over fixed time intervals. To investigate the relationship between low HRVO (SD < 0.5 BPM) during surgical procedures and mortality within 48 h post-procedure. We retrospectively reviewed all adult general surgical procedures performed at our center from January 1, 2003 through July 1, 2013 to identify patients who died within 48 h post-procedure. Demographic, heart rate, and mortality data were extracted from the electronic anesthesia record. Propensity score analysis was used to find matching controls based on age, gender, ASA score, anesthesia type, Charlson index, procedure type, emergency status, year, use of preoperative beta blocker, hypertension, diabetes, atrial fibrillation and heart failure. HRVO was calculated for each 5 min interval as the SD of all HR’s within that interval. Negative binomial regression was then used to model the count of intervals with HRVO < 0.5 BPM for the duration of the surgery. During the 10 year study period, 283 patients died within 48 h of procedure finish. These patients were matched to 566 patients who did not die within 48 h after procedure. Patients who died had a 39 % increase in frequency of low HRVO episodes compared to patients who survived (RR 1.39, 95 % CI 1.13–1.72; p = 0.003). Low HRVO during surgical procedure is associated with increased mortality risk within 48 h after procedure. Strategies to identify HRVO early and modify it may lead to improvement in outcomes.



Similar content being viewed by others
Abbreviations
- ANS:
-
Autonomic nervous system
- ASA:
-
American Society of Anesthesiologists
- ECG:
-
Electrocardiogram
- HRV:
-
Heart rate variability
- HRVO:
-
Heart rate volatility
- ICD-9:
-
International Statistical Classification of Diseases
- ICU:
-
Intensive care unit
- PRBC:
-
Packed red blood cells
- RR:
-
Relative risk
References
Grogan EL, Morris JA, Norris PR, France DJ, Ozdas A, Stiles REEA, et al. Reduced heart rate volatility. Ann Surg. 2004;240:547–56.
Electrophysiology TFOTESOCTNAS. Heart rate variability. Standards of measurement, physiological interpretation, and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Eur Heart J. 1996;93:1043–65.
Kleiger RE, Stein PK, Bigger JT. Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol. 2005;10:88–101. doi:10.1111/j.1542-474X.2005.10101.x.
Omerbegovic M. Analysis of heart rate variability and clinical implications. Med Arh. 2009;63:102–5.
Grogan EL, Norris PR, Speroff T, Ozdas A, France DJ, Harris PA, et al. Volatility: a new vital sign identified using a novel bedside monitoring strategy. J Trauma. 2005;58:7–12 (discussion 12–4).
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Dehejia RH, Wahba S. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 2002;84:151–61. doi:10.1162/003465302317331982.
Austin PC. Statistical criteria for selecting the optimal number of untreated subjects matched to each treated subject when using many-to-one matching on the propensity score. Am J Epidemiol. 2010;172(9):1092–7.
Rosenbaum PR, Rubin DB. The bias due to incomplete matching. Biometrics. 1985;41:103–16.
Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61.
Dexter F, Ledolter J, Davis E, Witkowski TA, Herman JH, Epstein RH. Systematic criteria for type and screen based on procedure’s probability of erythrocyte transfusion. Anesthesiology. 2012;116:768–78.
Tsuji H, Venditti FJ, Manders ES, Evans JC, Larson MG, Feldman CL, et al. Reduced heart rate variability and mortality risk in an elderly cohort The Framingham Heart Study. Circulation. 1994;90:878–83.
Huikuri HV, Raatikainen MJP, Moerch-Joergensen R, Hartikainen J, Virtanen V, Boland J, et al. Prediction of fatal or near-fatal cardiac arrhythmia events in patients with depressed left ventricular function after an acute myocardial infarction. Eur Heart J. 2009;30:689–98.
Norris PR, Morris JA, Ozdas A, Grogan EL, Williams AE. Heart rate variability predicts trauma patient outcome as early as 12 h: implications for military and civilian triage. J Surg Res. 2005;129:122–8.
Morris JA, Norris PR. Role of reduced heart rate volatility in predicting death in trauma patients. Adv Surg. 2005;39:77–96.
Laitio T, Jalonen J, Kuusela T, Scheinin H. The role of heart rate variability in risk stratification for adverse postoperative cardiac events. Anesth Analg. 2007;105:1548–60.
Scheffler P, Scheffler P, Muccio S, Muccio S, Egiziano G, Egiziano G, et al. Heart rate variability exhibits complication-dependent changes postsurgery. Angiology. 2013;64:597–603.
Marsch SC, Skarvan K, Schaefer HG, Naegeli B, Paganoni R, Castelli I, et al. Prolonged decrease in heart rate variability after elective hip arthroplasty. Br J Anaesth. 1994;72:643–9.
Amar D, Amar D, Fleisher M, Fleisher M, Pantuck CB, Pantuck CB, et al. Persistent alterations of the autonomic nervous system after noncardiac surgery. Anesthesiology. 1998;89:30–42.
Haase O, Haase O, Langelotz C, Langelotz C, Scharfenberg M, Scharfenberg M, et al. Reduction of heart rate variability after colorectal resections. Langenbecks Arch Surg. 2012;397:793–9.
Smith A-L, Owen H, Reynolds KJ. Can short-term heart rate variability be used to monitor fentanyl-midazolam induced changes in ANS preceding respiratory depression? J Clin Monit Comput. 2015;29:393–405. doi:10.1007/s10877-014-9617-z.
Paisansathan C, Lee M, Hoffman WE, Wheeler P. Sevoflurane anesthesia decreases cardiac vagal activity and heart rate variability. Clin Auton Res. 2007;17:370–4.
Hanss R, Hanss R, Renner J, Renner J, Ilies C, Ilies C, et al. Does heart rate variability predict hypotension and bradycardia after induction of general anaesthesia in high risk cardiovascular patients?*. Anaesthesia. 2008;63:129–35.
Jeanne M, Logier R, De Jonckheere J, Tavernier B. Heart rate variability during total intravenous anesthesia: effects of nociception and analgesia. Auton Neurosci. 2009;147:91–6.
Chen Z, Chen Z, Citi L, Citi L, Purdon PL, Purdon PL, et al. Instantaneous assessment of autonomic cardiovascular control during general anesthesia. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:8444–7.
Matchett G, Wood P. General anesthesia suppresses normal heart rate variability in humans. Chaos. 2014;24:023129.
El Beheiry H, Mak P. Effects of aging and propofol on the cardiovascular component of the autonomic nervous system. J Clin Anesth. 2013;25:637–43.
Hanss R, Block D, Bauer M, Ilies C, Magheli A, Schildberg-Schroth H, et al. Use of heart rate variability analysis to determine the risk of cardiac ischaemia in high-risk patients undergoing general anaesthesia. Anaesthesia. 2008;63:1167–73.
Jared M, Huston KJT. The pulse of inflammation: heart rate variability, the cholinergic anti-inflammatory pathway, and implications for therapy. J Intern Med. 2011;269:45.
Liu NT, Holcomb JB, Wade CE, Salinas J. Improving the prediction of mortality and the need for life-saving interventions in trauma patients using standard vital signs with heart-rate variability and complexity. Shock. 2015;43:549–55.
Ryan ML, Thorson CM, Otero CA, Vu T, Proctor KG. Clinical applications of heart rate variability in the triage and assessment of traumatically injured patients. Anesthesiol Res Pract. 2011;2011:1–8.
Riordan WP, Norris PR, Jenkins JM, Morris JA. Early loss of heart rate complexity predicts mortality regardless of mechanism, anatomic location, or severity of injury in 2178 trauma patients. J Surg Res. 2009;156:283–9.
Acknowledgments
Y. Mandel-Portnoy is funded by The National Heart Lung and Blood Institute through the Mount Sinai Emergency Medicine Research Career Development Program, 5K12HL109005.
Author information
Authors and Affiliations
Corresponding author
Additional information
Yael Mandel-Portnoy and Matthew A. Levin have contributed equally to this article.
Rights and permissions
About this article
Cite this article
Mandel-Portnoy, Y., Levin, M.A., Bansilal, S. et al. Low intraoperative heart rate volatility is associated with early postoperative mortality in general surgical patients: a retrospective case–control study. J Clin Monit Comput 30, 911–918 (2016). https://doi.org/10.1007/s10877-015-9792-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9792-6