Abstract
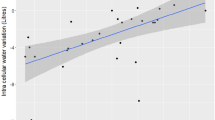
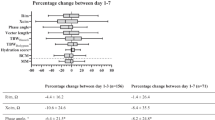
Fluid management is a crucial issue in intensive-care medicine. This study evaluated the feasibility and reproducibility of bioimpedance spectroscopy to measure body-water composition in critically ill patients, and compared fluid balance and daily changes in total body water (TBW) measured by bioimpedance. This observational study included 25 patients under mechanical ventilation. Fluid balance and bioimpedance measurements were recorded on 3 consecutive days. Whole-body bioimpedance spectroscopy was performed with exact or ideal body weights entered into the device, and with or without ICU monitoring. Reproducibility of bioimpedance spectroscopy was very good in all conditions despite ICU monitoring and mechanical ventilation. Bioimpedance measurements using an ideal body weight varied significantly, making the weighing procedure necessary. Comparison of fluid balance and daily changes in body weight provided the best correlation (ρ = 0.74; P < 0.0001). Daily changes in TBW were correlated with fluid balance (Spearman coefficient ρ = 0.31; P = 0.003) and this correlation was improved after exclusion of patients with a SOFA score >10 (ρ = 0.36; P = 0.05) and with extracorporeal circulation (ρ = 0.50; P = 0.005). Regardless of the technique used to estimate volume status, important limits of agreement were observed. Non-invasive determination of body-water composition using bioimpedance spectroscopy is feasible in critically ill patients but requires knowledge of the patient’s weight. The best method to assess volume status after fluid resuscitation and the value gained from information about body composition provided by bioimpedance techniques needs further evaluation.


Similar content being viewed by others
References
Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative G. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345(19):1368–77. doi:10.1056/NEJMoa010307.
Boyd JH, Forbes J, Nakada TA, Walley KR, Russell JA. Fluid resuscitation in septic shock: a positive fluid balance and elevated central venous pressure are associated with increased mortality. Crit Care Med. 2011;39(2):259–65. doi:10.1097/CCM.0b013e3181feeb15.
National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564–75. doi:10.1056/NEJMoa062200.
Koobi T, Kahonen M, Koskinen M, Kaukinen S, Turjanmaa VM. Comparison of bioimpedance and radioisotope methods in the estimation of extracellular water volume before and after coronary artery bypass grafting operation. Clin Physiol. 2000;20(4):283–91.
Network VNARFT, Palevsky PM, Zhang JH, O’Connor TZ, Chertow GM, Crowley ST, Choudhury D, Finkel K, Kellum JA, Paganini E, Schein RM, Smith MW, Swanson KM, Thompson BT, Vijayan A, Watnick S, Star RA, Peduzzi P. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359(1):7–20. doi:10.1056/NEJMoa0802639.
Schneider AG, Baldwin I, Freitag E, Glassford N, Bellomo R. Estimation of fluid status changes in critically ill patients: fluid balance chart or electronic bed weight? J Crit Care. 2012;27(6):745 e747–712. doi:10.1016/j.jcrc.2011.12.017.
Perren A, Markmann M, Merlani G, Marone C, Merlani P. Fluid balance in critically ill patients. Should we really rely on it? Minerva Anestesiol. 2011;77(8):802–11.
Roos AN, Westendorp RG, Frolich M, Meinders AE. Weight changes in critically ill patients evaluated by fluid balances and impedance measurements. Crit Care Med. 1993;21(6):871–7.
Wabel P, Chamney P, Moissl U, Jirka T. Importance of whole-body bioimpedance spectroscopy for the management of fluid balance. Blood Purif. 2009;27(1):75–80. doi:10.1159/000167013.
Earthman C, Traughber D, Dobratz J, Howell W. Bioimpedance spectroscopy for clinical assessment of fluid distribution and body cell mass. Nutr Clin Pract. 2007;22(4):389–405.
Buchholz AC, Bartok C, Schoeller DA. The validity of bioelectrical impedance models in clinical populations. Nutr Clin Pract. 2004;19(5):433–46.
Moissl UM, Wabel P, Chamney PW, Bosaeus I, Levin NW, Bosy-Westphal A, Korth O, Muller MJ, Ellegard L, Malmros V, Kaitwatcharachai C, Kuhlmann MK, Zhu F, Fuller NJ. Body fluid volume determination via body composition spectroscopy in health and disease. Physiol Meas. 2006;27(9):921–33. doi:10.1088/0967-3334/27/9/012.
Kraemer M, Rode C, Wizemann V. Detection limit of methods to assess fluid status changes in dialysis patients. Kidney Int. 2006;69(9):1609–20. doi:10.1038/sj.ki.5000286.
Chamney PW, Wabel P, Moissl UM, Muller MJ, Bosy-Westphal A, Korth O, Fuller NJ. A whole-body model to distinguish excess fluid from the hydration of major body tissues. Am J Clin Nutr. 2007;85(1):80–9.
Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–8.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10.
Valentinuzzi ME, Morucci JP, Felice CJ. Bioelectrical impedance techniques in medicine. Part II: monitoring of physiological events by impedance. Crit Rev Biomed Eng. 1996;24(4–6):353–466.
Foley K, Keegan M, Campbell I, Murby B, Hancox D, Pollard B. Use of single-frequency bioimpedance at 50 kHz to estimate total body water in patients with multiple organ failure and fluid overload. Crit Care Med. 1999;27(8):1472–7.
Thomasset A. Bio-electric properties of tissues. Estimation by measurement of impedance of extracellular ionic strength and intracellular ionic strength in the clinic. Lyon Med. 1963;209:1325–50.
Patel RV, Peterson EL, Silverman N, Zarowitz BJ. Estimation of total body and extracellular water in post-coronary artery bypass graft surgical patients using single and multiple frequency bioimpedance. Crit Care Med. 1996;24(11):1824–8.
Plank LD, Monk DN, Woollard GA, Hill GL. Evaluation of multifrequency bioimpedance spectroscopy for measurement of the extracellular water space in critically ill patients. Appl Radiat Isot. 1998;49(5–6):481–3.
Faisy C, Rabbat A, Kouchakji B, Laaban JP. Bioelectrical impedance analysis in estimating nutritional status and outcome of patients with chronic obstructive pulmonary disease and acute respiratory failure. Intensive Care Med. 2000;26(5):518–25.
Earthman CP, Matthie JR, Reid PM, Harper IT, Ravussin E, Howell WH. A comparison of bioimpedance methods for detection of body cell mass change in HIV infection. J Appl Physiol. 2000;88(3):944–56.
Cox-Reijven PL, van Kreel B, Soeters PB. Accuracy of bioelectrical impedance spectroscopy in measuring changes in body composition during severe weight loss. J Parenter Enter Nutr. 2002;26(2):120–7.
Mager JR, Sibley SD, Beckman TR, Kellogg TA, Earthman CP. Multifrequency bioelectrical impedance analysis and bioimpedance spectroscopy for monitoring fluid and body cell mass changes after gastric bypass surgery. Clin Nutr. 2008;27(6):832–41. doi:10.1016/j.clnu.2008.06.007.
Balik M, Sedivy J, Waldauf P, Kolar M, Smejkalova V, Pachl J. Can bioimpedance determine the volume of distribution of antibiotics in sepsis? Anaesth Intensive Care. 2005;33(3):345–50.
Piccoli A, Pittoni G, Facco E, Favaro E, Pillon L. Relationship between central venous pressure and bioimpedance vector analysis in critically ill patients. Crit Care Med. 2000;28(1):132–7.
Acknowledgments
The authors would like to thank Dr. Erwan Floch, PharmD (Newmed Publishing Services) for reviewing this manuscript. This study was supported solely by the Department of Anesthesiology and Critical care.
Conflict of interest
The authors declare no conflicts of interest. The Body Composition Monitor® was bought by our institution and the electrodes were kindly provided by Fresenius Medical Care (Bad Homburg, Germany), who did not participate in this paper’s redaction.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary online Fig. 1
Bland and Altman plot concordance correlation between daily changes in fluid balance (FB) in liters and body weight (BW) in kilograms (A), and between daily changes in fluid balance in liters and total body water (TBW) in liters measured by bioimpedance spectroscopy (B) after exclusion of patients with a SOFA score of > 10. The middle line symbolizes the mean bias; the upper and lower lines symbolize the upper and lower limits of agreement. (TIFF 518 kb)
Supplementary online Fig. 2
Bland and Altman concordance correlation between daily changes in fluid balance (FB) in liters and body weight (BW) in kilograms (A), and between daily changes in fluid balance in liters and total body water (TBW) in liters measured by bioimpedance spectroscopy (B) after exclusion of patients with extracorporeal circulation. The middle line symbolizes the mean bias; the upper and lower lines symbolize the upper and lower limits of agreement. (TIFF 142 kb)
Rights and permissions
About this article
Cite this article
Dewitte, A., Carles, P., Joannès-Boyau, O. et al. Bioelectrical impedance spectroscopy to estimate fluid balance in critically ill patients. J Clin Monit Comput 30, 227–233 (2016). https://doi.org/10.1007/s10877-015-9706-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9706-7