Abstract
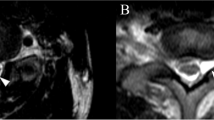
Interscalene brachial plexus block (IBPB) has been widely used in shoulder surgical procedures. The incidence of postoperative neural injury has been estimated to be as high as 3 %. We report a long-term neurologic deficit after a nerve stimulator assisted brachial plexus block. A 55 year-old male, with right shoulder impingement syndrome was scheduled for elective surgery. The patient was given an oral dose of 10 mg of diazepam prior to the nerve stimulator assisted brachial plexus block. The patient immediately complained, as soon as the needle was placed in the interscalene area, of a sharp pain in his right arm and he was sedated further. Twenty-four hours later, the patient complained of severe shoulder and arm pain that required an increased dose of analgesics. Severe peri-scapular atrophy developed over the following days. Electromyography studies revealed an upper trunk plexus injury with severe denervation of the supraspinatus, infraspinatus and deltoid muscles together with a moderate denervation of the biceps brachii muscle. Chest X-rays showed a diaphragmatic palsy which was not present post operatively. Pulmonary function tests were also affected. Phrenic nerve paralysis was still present 18 months after the block as was dysfunction of the brachial plexus resulting in an inability to perform flexion, abduction and external rotation of the right shoulder. Severe brachial plexopathy was probably due to a local anesthetic having been administrated through the perineurium and into the nerve fascicles. Severe brachial plexopathy is an uncommon but catastrophic complication of IBPB. We propose a clinical algorithm using ultrasound guidance during nerve blocks as a safer technique of regional anesthesia.


Similar content being viewed by others
References
Lin E, Choi J, Hadzic A. Peripheral nerve blocks for outpatient surgery: evidence-based indications. Curr Opin Anaesthesiol. 2013;26(4):467–74.
Moore DD, Maerz T, Anderson K. Shoulder surgeons’ perceptions of interscalene nerve blocks and a review of complications rates in the literature. Phys Sports Med. 2013;41(3):77–84.
Bilbao Ares A, Sabaté A, Porteiro L, Ibáñez B, Koo M, Pi A. Neurological complications associated with ultrasound-guided interscalene and supraclavicular block in elective surgery of the shoulder and arm. Prospective observational study in a university hospital. Rev Esp Anestesiol Reanim. 2013;60(7):384–91.
Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104(4):965–74.
Robaux S, Bouaziz H, Boisseau N, Raucoules-Aimé M, Laxenaire MC. Persistent phrenic nerve paralysis following interscalene brachial plexus block. Anesthesiology. 2001;95(6):1519–21.
Ediale KR, Myung CR, Neuman GG. Prolonged hemidiaphragmatic paralysis following interscalene brachial plexus block. J Clin Anesth. 2004;16(8):573–5.
Borgeat A, Ekatodramis G, Kalberer F, Benz C. Acute and nonacute complications associated with interscalene block and shoulder surgery: a prospective study. Anesthesiology. 2001;95(4):875–80.
Benumof JL. Permanent loss of cervical spinal cord function associated with interscalene block performed under general anesthesia. Anesthesiology. 2000;93(6):1541–4.
Orebaugh SL, Mukalel JJ, Krediet AC, Weimer J, Filip P, McFadden K, Bigeleisen PE. Brachial plexus root injection in a human cadaver model: injectate distribution and effects on the neuraxis. Reg Anesth Pain Med. 2012;37(5):525–9.
Sala-Blanch X, Vandepitte C, Laur JJ, Horan P, Xu D, Reina MA, Karmakar MK, Clark TB, Hadzic A. A practical review of perineural versus intraneural injections: a call for standard nomenclature. Int Anesthesiol Clin. 2011;49(4):1–12.
Jeng CL, Rosenblatt MA. Intraneural injections and regional anesthesia: the known and the unknown. Minerva Anestesiol. 2011;77(1):54–8.
Barrington MJ, Watts SA, Gledhill SR, Thomas RD, Said SA, Snyder GL, Tay VS, Jamrozik K. Preliminary results of the Australasian Regional Anaesthesia Collaboration: a prospective audit of more than 7000 peripheral nerve and plexus blocks for neurologic and other complications. Reg Anesth Pain Med. 2009;34(6):534–41.
Sviggum HP, Jacob AK, Mantilla CB, Schroeder DR, Sperling JW, Hebl JR. Perioperative nerve injury after total shoulder arthroplasty: assessment of risk after regional anesthesia. Reg Anesth Pain Med. 2012;37(5):490–4.
Sala-Blanch X, López AM, Vandepitte C. Safety algorithms for ultrasound guided blocks: the next challenge. Rev Esp Anestesiol Reanim. 2015;62(2):116–7.
Bollini CA, Urmey WF, Vascello L, Cacheiro F. Relationship between evoked motor response and sensory paresthesia in interscalene brachial plexus block. Reg Anesth Pain Med. 2003;28(5):384–8.
Gadsden JC, Choi JJ, Lin E, Robinson A. Opening injection pressure consistently detects needle-nerve contact during ultrasound-guided interscalene brachial plexus block. Anesthesiology. 2014;120(5):1246–53.
Jeng CL, Torrillo TM, Rosenblatt MA. Complications of peripheral nerve blocks. Br J Anesth. 2010;105(S1):97–107.
Conflict of interest
If no conflict exists, authors should state: The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Avellanet, M., Sala-Blanch, X., Rodrigo, L. et al. Permanent upper trunk plexopathy after interscalene brachial plexus block. J Clin Monit Comput 30, 51–54 (2016). https://doi.org/10.1007/s10877-015-9681-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9681-z