Abstract
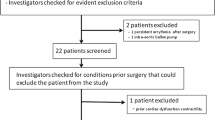
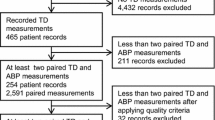
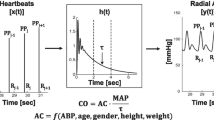
Phenylephrine is often used to treat intra-operative hypotension. Previous studies have shown that the FloTrac cardiac monitor may overestimate cardiac output (CO) changes following phenylephrine administration. A new algorithm (4th generation) has been developed to improve performance in this setting. We performed a prospective observational study to assess the effects of phenylephrine administration on CO values measured by the 3rd and 4th generation FloTrac algorithms. 54 patients were enrolled in this study. We used the Nexfin, a pulse contour method shown to be insensitive to vasopressor administration, as the reference method. Radial arterial pressures were recorded continuously in patients undergoing surgery. Phenylephrine administration times were documented. Arterial pressure recordings were subsequently analyzed offline using three different pulse contour analysis algorithms: FloTrac 3rd generation (G3), FloTrac 4th generation (G4), and Nexfin (nf). One minute of hemodynamic measurements was analyzed immediately before phenylephrine administration and then repeated when the mean arterial pressure peaked. A total of 157 (4.6 ± 3.2 per patient, range 1–15) paired sets of hemodynamic recordings were analyzed. Phenylephrine induced a significant increase in stroke volume (SV) and CO with the FloTrac G3, but not with FloTrac G4 or Nexfin algorithms. Agreement between FloTrac G3 and Nexfin was: 0.23 ± 1.19 l/min and concordance was 51.1 %. In contrast, agreement between FloTrac G4 and Nexfin was: 0.19 ± 0.86 l/min and concordance was 87.2 %. In conclusion, the pulse contour method of measuring CO, as implemented in FloTrac 4th generation algorithm, has significantly improved its ability to track the changes in CO induced by phenylephrine.





Similar content being viewed by others
References
Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg. 2011;112:1392–402.
Rhodes A, Cecconi M, Hamilton M, Poloniecki J, Woods J, Boyd O, Bennett D, Grounds RM. Goal-directed therapy in high-risk surgical patients: a 15-year follow-up study. Intensive Care Med. 2010;36:1327–32.
Dalfino L, Giglio MT, Puntillo F, Marucci M, Brienza N. Haemodynamic goal-directed therapy and postoperative infections: earlier is better. A systematic review and meta-analysis. Crit Care. 2011;15(3):R154.
Benes J, Chytra I, Altmann P, Hluchy M, Kasal E, Svitak R, Pradl R, Stepan M. Intraoperative fluid optimization using stroke volume variation in high risk surgical patients: results of prospective randomized study. Crit Care. 2010;14:R118.
Ramsingh DS, Sanghvi C, Gamboa J, Cannesson M, Applegate RL 2nd. Outcome impact of goal directed fluid therapy during high risk abdominal surgery in low to moderate risk patients: a randomized controlled trial. J Clin Monit Comput. 2013;27(3):249–57.
Cecconi M, Fasano N, Langiano N, Divella M, Costa MG, Rhodes A. Della Rocca G. Goal-directed haemodynamic therapy during elective total hip arthroplasty under regional anaesthesia. Crit Care. 2011;15(3):R132.
Mayer J, Boldt J, Mengistu AM, Röhm KD, Suttner S. Goal-directed intraoperative therapy based on autocalibrated arterial pressure waveform analysis reduces hospital stay in high-risk surgical patients: a randomized, controlled trial. Crit Care. 2010;14:R18.
Gutierrez MC, Moore PG, Liu H. Goal directed therapy in intraoperative fluid and hemodynamic management. J Biomed Res. 2013;27(5):357–65.
Eleftheriadis S, Galatoudis Z, Didilis V, Bougioukas I, Schön J, Heinze H, Berger KU, Heringlake M. Variations in arterial blood pressure are associated with parallel changes in FloTrac/Vigileo-derived cardiac output measurements: a prospective comparison study. Crit Care. 2009;13:R179.
Lorsomradee S, Cromheecke S, De Hert SG. Uncalibrated arterial pulse contour analysis versus continuous thermodilution technique: effects of alterations in arterial waveform. J Cardiothorac Vasc Anesth. 2007;21:636–43.
Monnet X, Anguel N, Naudin B, Jabot J, Richard C, Teboul JL. Arterial pressure-based cardiac output in septic patients: different accuracy of pulse contour and uncalibrated pressure waveform devices. Crit Care. 2010;14:R109.
Meng L, Tran NP, Alexander BS, Laning K, Chen G, Kain ZN, Cannesson M. The impact of phenylephrine, ephedrine, and increased preload on third-generation Vigileo-FloTrac and esophageal doppler cardiac output measurements. Anesth Analg. 2011;113:751–7.
Pratt B, Roteliuk L, Hatib F, Frazier J, Wallen RD. Calculating arterial pressurebased cardiac output using a novel measurement and analysis method. Biomed Instrum Technol. 2007;41:403–11.
Bogert LW, Wesseling KH, Schraa O, Van Lieshout EJ, de Mol BA, van Goudoever J, Westerhof BE, van Lieshout JJ. Pulse contour cardiac output derived from non-invasive arterial pressure in cardiovascular disease. Anaesthesia. 2010;65:1119–25.
Broch O, Renner J, Gruenewald M, Meybohm P, Schöttler J, Caliebe A, Steinfath M, Malbrain M, Bein B. A comparison of the Nexfin® and transcardiopulmonary thermodilution to estimate cardiac output during coronary artery surgery. Anaesthesia. 2012;67(4):377–83.
Chen G, Meng L, Alexander B, Tran NP, Kain ZN, Cannesson M. Comparison of noninvasive cardiac output measurements using the Nexfin monitoring device and the esophageal Doppler. J Clin Anesth. 2012;24:275–83.
Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–92.
Cannesson M, Jian Z, Chen G, Vu TQ, Hatib F. Effects of phenylephrine on cardiac output and venous return depend on the position of the heart on the Frank-Starling relationship. J Appl Physiol. 2012;113:281–9.
Yin J, Tian L. Joint confidence region estimation for area under ROC curve and Youden index. Stat Med. 2014;33:985–1000.
Peyton PJ, Chong SW. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. Anesthesiology. 2010;113:1220–35.
Wesseling KH, Smith NT, Nichols WW, Weber H, De Wit B, Beneken JE. Beat-to-beat cardiac output from the arterial pressure pulse contour. In: Feldman SA, Leigh JM, Spierdijk J, editors. Measurement in Anaesthesia. Leiden: Leiden University Press; 1974. p. 148–64.
Westerhof N, Lankhaar JW, Westerhof BE. The arterial Windkessel. Med Biol Eng Comput. 2009;47:131–41.
Bubenek-Turconi SI, Craciun M, Miclea I, Perel A. Noninvasive continuous cardiac output by the Nexfin before and after preload-modifying maneuvers: a comparison with intermittent thermodilution cardiac output. Anesth Analg. 2013;117(2):366–72.
Maas JJ, Pinsky MR, de Wilde RB, de Jonge E, Jansen JR. Cardiac output response to norepinephrine in postoperative cardiac surgery patients: interpretation with venous return and cardiac function curves. Crit Care Med. 2013;41(1):143–50.
Bubenek-Turconi SI, Craciun M, Miclea I, Perel A. Noninvasive continuous cardiac output by the Nexfin before and after preload-modifying maneuvers: a comparison with intermittent thermodilution cardiac output. Anesth Analg. 2013;117(2):366–72.
Acknowledgments
The authors thank Zhongping Jian, PhD of Edwards Lifesciences for assisting with the data analysis and members of the Department of Anesthesiology and Perioperative Care, University of California, Irvine for assisting with part of the data collection. This work was supported by the University of California Davis Health System Department of Anesthesiology and Pain Medicine, and NIH grant UL1 TR000002. This study was supported by a grant from Edwards Lifesciences, a grant from Jiangsu Province’s by Key Provincial Talents Program, China (Fuhai Ji), by Jiangsu province’s six major peak talents program, China (Fuhai Ji) and by Suzhou science and No. SYS201111 (Fuhai Ji) from Technology Bureau’s program, China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Fuhai Ji and Jian Li have contributed equally to this paper.
Rights and permissions
About this article
Cite this article
Ji, F., Li, J., Fleming, N. et al. Reliability of a new 4th generation FloTrac algorithm to track cardiac output changes in patients receiving phenylephrine. J Clin Monit Comput 29, 467–473 (2015). https://doi.org/10.1007/s10877-014-9624-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9624-0