Abstract
Objective
To investigate the incidence, type and etiology of perioperative metabolic disturbances associated with major abdominal surgery. We hypothesized that metabolic alkalemia is more frequent than metabolic acidemia.
Methods
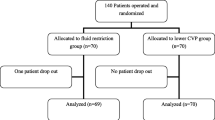
This was a prospective, observational study, performed in a university-affiliated hospital. 98 consecutive patients undergoing major abdominal surgery were included in the study. Patients were observed by serial vital signs and laboratory measurements during the preoperative, intraoperative, PACU and the first three postoperative day periods. Central venous pressure, systolic pressure variation, fluid input, urine output, temper- ature, electrolytes, and acid–base variables were recorded. The primary endpoint of the study was the incidence of metabolic alkalemia or acidemia. Metabolic alkalemia was defined as pH >7.45 and BE >+3. Metabolic acidemia was defined as pH <7.35 and BE <−3. Continuous variables were described as mean ± standard deviation. Distributions of continuous variables was assessed for normalty using the Kolmogorov–Smirnov test (cut off at P = 0.01). The frequency of metabolic acidemia or alkalemia was compared across time points using Cochran’s Q test and between time points using the binomial distribution.
Results
Metabolic acidemia occurred only intraoperatively and in the PACU. Subjects with metabolic acidemia were older, (74 ± 9 yr. vs. 66 ± 12, P = 0.01). Intraoperative body temperature was inversely associated with PACU lactate (P = 0.035). Blood loss >500 mL was more frequent in acidemic patients (42% vs. 19%, P = 0.033). More patients with hyperphosphatemia had acidemia than subjects without hyperphosphatemia (39% vs. 17%, P = 0.019). Metabolic alkalemia occurred more frequently than metabolic acidemia (49% vs. 23%, P < 0.0001) and was correlated with hypochloremia. The incidence of metabolic alkalemia decreased from baseline to intraoperative and PACU periods (13% vs. 3%, P = 0.003) and increased from the PACU to the three postoperative days (3% vs. 45%, P = 0.007).
Conclusions
Metabolic alkalemia occurred more frequently than metabolic acidemia and occurred mainly preoperatively and postoperatively, while acidemia occurred mainly during surgery and in the PACU.
Similar content being viewed by others
References
Tan HL, Liew QY, Loo S, Hawkins R. Severe hyperphosphataemia and associated electrolyte and metabolic derangement following the administration of sodium phosphate for bowel preparation. Anaesthesia. 2002;57:478–83.
Waters JH, Miller LR, Clack S, Kim JV. Cause of metabolic acidemia in prolonged surgery. Crit Care Med. 1999;27:2142–6.
Okusawa S, Aikawa N, Abe O. Postoperative metabolic alkalemia following general surgery: its incidence and possible etiology. Jpn J Surg. 1989;19:312–8.
Marko P, Gabrielli A, Caruso LJ. Too much lactate or too little liver? J Clin Anesth. 2004;16:389–95.
Bastian PJ, Albers P, Haferkamp A, Schumacher S, Muller SC. Modified ureterosigmoidostomy (Mainz Pouch II) in different age groups and with different techniques of ureteric implantation. BJU Int. 2004;94:345–9.
Aker J, O’Sullivan C. The selection and administration of perioperative intravenous fluids for the pediatric patient. J Perianesth Nurs. 1998;13:172–81.
Jones D, Baldwin I, Bellomo R. A technique for the determination of systolic pressure variation in the systemic and pulmonary arterial circulations. Crit Care Resusc. 2004;6:204–8.
Marino PL. Acid-base interpretations. In: Marino PL, editor. The ICU book 3rd ed. Philadelphia: Lippincott !illiams & Wilkins; 2007. p. 540, 568.
Durbin CG. Arterial blood gas analysis and monitoring. In: Lake LC, Hines RL, Blitt CD, editors. Clinical monitoring. Philadelphia: W.B.Saunders Comp; 2001. p. 347.
Klein S, Sakurai Y, Romijn JA, Carroll RM. Progressive alterations in lipid and glucose metabolism during short-term fasting in young adult men. Am J Physiol. 1998;265:E801–6.
Maekawa N, Mikawa K, Yaku H, Nishina K, Obara H. Effects of 2-, 4- and 12-hour fasting intervals on preoperative gastric fluid pH and volume, and plasma glucose and lipid homeostasis in children. Acta Anaesthesiol Scand. 1993;37:783–7.
Chambrier C, Aouifi A, Bon C, Saudin F, Paturel B, Bouletreau P. Effects of intraoperative glucose administration on circulating metabolites and nitrogen balance during prolonged surgery. J Clin Anesth. 1999;11:646–51.
Schricker T, Carli F, Lattermann R, Wachter U, Georgieff M. Glucose infusion does not suppress increased lipolysis after abdominal surgery. Nutrition. 2001;17:85–90.
Freeman BD. Fluid and electrolyte abnormalities. In: Mulholland MW, Doherty GM, editors. Complications in surgery. Philadelphia: Lippincott Williams & Wilkins; 2006. p. 148.
Morgan TJ. The meaning of acid-base abnormalities in the intensive care unit: part III–effects of fluid administration. Crit Care. 2005;9:204–11.
Chappell D, Jacob M, Hofmann-Kiefer K, Conzen P, Rehm M. A rational approach to perioperative fluid management. Anesthesiology. 2008;109:723–40.
Beloosesky Y, Grinblat J, Weiss A, Grosman B, Gafter U, Chagnac A. Electrolyte disorders following oral sodium phosphate administration for bowel cleansing in elderly patients. Arch Intern Med. 2003;163:803–8.
Amlal H, Wang Z, Soleimani M. Potassium depletion downregulates chloride-absorbing transporters in rat kidney. J Clin Invest. 1998;101:1045–54.
McAuliffe JJ, Lind L, Leith DE, Fencl V. Hypoproteinemic alkalemia. Am J Med. 1986;81:86–90.
Author information
Authors and Affiliations
Corresponding author
Additional information
Boaz M, Iskhakov A, Tsivian A, Shimonov M, Berkenstadt H, Izakson A, Szmuk P, Evron S, Muggia M, Ezri T. Perioperative metabolic alkalemia is more frequent than metabolic acidemia in major elective abdominal surgery.
Rights and permissions
About this article
Cite this article
Boaz, M., Iskhakov, A., Tsivian, A. et al. Perioperative metabolic alkalemia is more frequent than metabolic acidemia in major elective abdominal surgery. J Clin Monit Comput 25, 223–230 (2011). https://doi.org/10.1007/s10877-011-9299-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-011-9299-8