Abstract
Background
All current methods of core temperature monitoring have limitations. There is at least one skin temperature probe that can be modified to a nasal temperature probe (NP). This study was conducted to validate this modified skin temperature probe as an accurate surrogate measure of core temperature by comparing the temperature measurements obtained from NP to those from the esophageal stethoscope (ES).
Methods
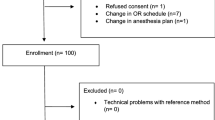
In 45 adult patients undergoing general anesthesia, one pair of simultaneous temperature measurements were obtained from the ES (E temp) and the NP (N temp).
Results
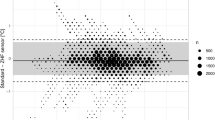
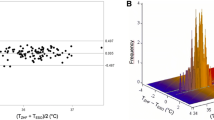
The NP was easily inserted in all patients. No patient developed epistaxis. The magnitudes of the differences between N temp and E temp measurements were 0.2°C or less in 43 out of 45 patients (95.6%); 0.1°C or less in 33 patients (73.3%). On average, the E temp was 0.05°C higher than the N temp. The 95% prediction interval for the E temp−N temp difference was −0.2°C to +0.3°C. Thus we expect the magnitude of the temperature difference to be less than 1/3°C in the next future individual patient.
Conclusion
In adults, the NP readings closely match the core temperature readings obtained by ES and thus can be used as a reliable surrogate measure of core temperature. This technique may be useful and advantageous in various situations, particularly when other methods of core temperature monitoring are not available or reliable.
Similar content being viewed by others
References
Cereda M, Maccioli G. Intraoperative temperature monitoring. Int Anesthesiol Clin 2004; 42(2):41–54
Tabor MW, Blaho DM, Schriver WR. Tympanic membrane perforation: complications of tympanic thermometry during general anesthesia. Oral Surg Oral Med Oral Pathol 1981; 51:581–583
Wallace CT, Marks WE Jr, Adkins WY, Mahaffey JE. Perforation of the tympanic membrane, a complication of tympanic membrane thermometry during anesthesia. Anesthesiology 1974; 41:290–291
Webb GE. Comparison of esophageal and tympanic membrane temperature monitoring during cardiopulmonary bypass. Anesth Analg 1973;52:729–733
Doezema D, Lunt M, Tandberg D. Cerumen occlusion lowers infrared tympanic membrane temperature measurement. Acad Emerg Med 1995; 2:17–19
Muravchick S. Deep body thermometry during general anesthesia. Anesthesiology 1983; 58(3):271–275
Whitby JD, Dunkin IJ. Temperature differences in the oesophagus preliminary study. Br J Anaesth 1968; 40:991–995
Kaufman RD. The relationship between esophageal temperature gradient and heart and lung sounds heard by esophageal stethoscope. Anesth Analg 1987; 66:1046–1048
Nelson EJ. Grissom: continuous gastric suctioning decreases measured esophageal temperature during general anesthesia. J Clin Monit Comput 1996; 12(6):429–432
Hahn GJ, Meeker WQ. Statistical intervals: a guide for practitioners. New York: Wiley, 1991
Armitage P, Berry G. Statistical methods in medical research, 2nd edn. Oxford: Blackwell Scientific Publications, 1987, p. 157
Braitman LE. Confidence intervals assess both clinical significance and statistical significance. Ann Intern Med 1991; 114(6):515–517
Sessler DI. A proposal for new temperature monitoring and thermal management guidelines. Anesthesiology 1998; 89(5):1298–1300
Clinical Guidelines for the Prevention of Unplanned Perioperative Hypothermia, Surgical Care Improvement Project, Centers for Medicare and Medicaid Services, 2007
Winkler M, Akca O, Birkenberg B, Hetz H, et al. Aggressive warming reduces blood loss during hip arthroplasty. Anesth Analg 2000; 91:978–984
Stone DJ, Bogdonoff DL. Airway considerations in the management of patients requring long-term endotracheal intubation. Anesth Analg 1992; 74:276–287
Vaughan MS, Cork RC, Vaughan R. Inaccuracy of liquid crystal thermometry to identify core temperature trends in postoperative adults. Anesth Analg 1982:61:284–287
Burgess GE III, Cooper JR, Marino RJ, Peuler MJ. Continuous monitoring of skin temperature using a liquid-crystal thermometer during anesthesia. South Med J 1978; 71:516–518
Kumar P, Arora H. Potential aspiration hazard when using a nasopharyngeal temperature probe with disposable cover. J Clin Anesth 2006; 18(7):556–557
Frank SM, Nguyen JM, Garcia CM, Barnes RA. Temperature monitoring during regional anesthesia. Anesth Analg 1999; 88(2):373–377
Author information
Authors and Affiliations
Corresponding author
Additional information
Roth JV, Braitman LE. Nasal temperature can be used as a reliable surrogate measure of core temperature.
Rights and permissions
About this article
Cite this article
Roth, J.V., Braitman, L.E. Nasal Temperature can be used as a Reliable Surrogate Measure of Core Temperature. J Clin Monit Comput 22, 309–314 (2008). https://doi.org/10.1007/s10877-008-9134-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-008-9134-z