Abstract
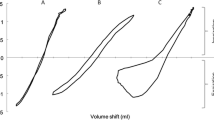
Objectives. Develop a sensitive algorithm and index for detection of asthma patients using forced expiratory flow curves. Methods. A lumped-parameter model of forced expiration was developed. The model can predict the flow-volume curve during forced expiratory maneuver. The flow-volume curves generated by the model depend on values of resistance parameters (FER). Use of flow-volume curves recorded from normal subjects and from patients with asthma before and after ventolin inhalation as inputs for the inverse model, yielded the resistance parameters for each case. These parameters are based on the entire information presented in the flow-volume curve and on the reduction in flow at all lung volumes. Results. Forced Expiratory Resistance (FER N ) indices were estimated at different percent of lung volumes using the inverse model. The index was significantly affected by inhalation of ventolin in asthmatic patients and was insensitive to ventolin inhalation in normal patients. In asthmatic patients, the FER index at five lung volumes (out of eight), was two–five times greater than in normal subjects with p ≪ 0.05 (three of them with p ≪ 0.01). Conclusions. The estimated parameters were sensitive indicators of the degree of lung function impairment and were able to accurately distinguish between healthy and asthmatic patients.
Similar content being viewed by others
References
Abboud S, Barnea O, Guber A, Narkis N, Bruderman I, Maximum expiratory flow-volume curve: mathematical model and experimental results. Med Eng Phys 1995; 17(5): 332–336.
Barnea O, Abboud S, Guber A, Bruderman I, New model-based indices for maximum expiratory flow-volume curve in patients with chronic obstructive pulmonary disease. Comput Biol Med 1996; 26(2): 123–131.
Clement J, Pardeans J, van de Woestijne KP, Expiratory flow rates, driving pressures and time-dependent factors. Simulation by means of a model. Resp Physiol 1974; 20: 353–369.
Fry DL, Theoretical considerations of the bronchial pressure-flow-volume relationships with particular reference to the maximum expiratory flow volume curve. Phys Med Biol 1958; 3: 174–194.
Fry DL, A preliminary lung model for simulating the aerodynamics of the bronchial tree. Comp Biomed Res 1968; 2: 11–134.
Lambert RK, Wilson TA, Hyatt RE, Rodarte JR, A computational model for expiratory flow. J Appl Physiol 1982; 52(1): 44–56.
Pardaens J, van de Woestijne KP, Clement J, A physical model of expiration. J Appl Physiol 1972; 33(4): 479–490.
Reynolds DB, Lee JS, Steady pressure-flow relationship of a model of the canine bronchial tree. J Appl Physiol 1981; 51: 1072–1079.
Author information
Authors and Affiliations
Corresponding author
Additional information
Barnea O, Abboud S, Guber A. Model-based prediction of expiratory resistance index in patients with asthma
Rights and permissions
About this article
Cite this article
Barnea, O., Abboud, S., Guber, A. et al. Model-Based Prediction of Expiratory Resistance Index in Patients with Asthma. J Clin Monit Comput 18, 241–245 (2004). https://doi.org/10.1007/s10877-005-9612-5
Received:
Revised:
Issue Date:
DOI: https://doi.org/10.1007/s10877-005-9612-5