Abstract
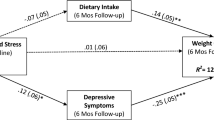
Lower income is associated with greater stress, and stress has been shown to undermine treatment engagement and weight loss outcomes in face-to-face interventions. The present study examined whether lower income predicts treatment engagement and weight loss outcomes during an online behavioral weight loss (BWL) intervention. A total of N = 260 participants (79.2% female; 50.7 ± 11.9 years of age; 60.3% non-Hispanic White) were enrolled into an online BWL program and had their income, stress, program engagement, and weight measured. Results showed that stress fully mediated the effect of income on engagement in the online program. Further, lower income predicted poorer weight loss outcomes, and this effect was partially mediated by perceived stress. This is the first study to demonstrate that lower income is associated with poorer engagement and weight loss outcomes in an online weight loss program, underscoring the need for systems-level stress reduction programs and individual level stress management tools, particularly for individuals with lower income.

Similar content being viewed by others
References
American Diabetes Association. (2011). Diabetes statistics. http://www.diabetes.org/diabetes-basics/diabetes-statistics/.
American Diabetes Association. (2013). Stress. www.diabetes.org/living-with-diabetes/complications/mental-health/stress.html.
American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (DSM-5) 5th ed. American Psychiatric Publishing.
American Psychological Association (2017). Stress and Health Disparities. www.apa.org/pi/health-disparities/resources/stress-report.pdf.
Health and Human Services Department (2017). Annual Update of the HHS Poverty Guidelines. www.federalregister.gov/documents/2017/01/31/2017-02076/annual-update-of-the-hhs-poverty-guidelines
Bandura, A (1986). Social foundations of thought and action: A social cognitive theory. Prentice-Hall.
Beckles, G. L., & Chou, C. F. (2016). Disparities in the prevalence of diagnosed diabetes - United States, 1999–2002 and 2011–2014. Morbidity and Mortality Weekly Report, 65, 1265–1269.
Bennett, G. G., Warner, E. T., Glasgow, R. E., Askew, S., Goldman, J., Ritzwoller, D. P., Emmons, K. M., Rosner, B. A., & Colditz, G. A. (2012). Obesity treatment for socioeconomically disadvantaged patients in primary care practice. Archives of Internal Medicine, 172, 565–574.
Brantley, P., J., Stewart, D. W., Myers, V. H., Matthews-Ewald, M. R., Ard, J. D., , et al. (2014). Psychosocial predictors of weight regain in the weight loss maintenance trial. Journal of Behavioral Medicine, 37, 1155–1168.
Brinkworth, G. D., Buckley, J. D., Noakes, M., Clifton, P. M., & Wilson, C. J. (2009). Long-term effects of a very low-carbohydrate diet and a low-fat diet on mood and cognitive function. Archives of Internal Medicine, 169, 1873–1880.
Centers of Disease Control (2018). Adult obesity facts: Overweight & obesity 2018. https://www.cdc.gov/obesity/data/adult.html.
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24, 385–396.
Cohen, S. & Williamson, G. (1988). Perceived stress in a probability sample of the United States. In: Spacapan, S, Oskamp, S (Eds.). The social psychology of health (pp.31–68). Sage.
Cozier, Y. C., Yu, J., Coogan, P. F., Bethea, T. N., Rosenberg, L., & Palmer, J. R. (2014). Racism, segregation, and risk of obesity in the Black Women’s Health Study. American Journal of Epidemiology, 179, 875–883.
Crain, A. L., Sherwood, N. E., Martenson, B. C., & Jeffery, R. W. (2018). Mediators of weight loss maintenance in the keep it off trial. Annals of Behavioral Medicine, 52, 9–18.
Daubenmier, J., Chao, M. T., Hartogensis, W., Liu, R., Moran, P. J., Acree, M. C., et al. (2020). Exploratory analysis of racial/ethnic and educational differences in a randomized controlled trial of a mindfulness-based weight loss intervention. Psychosomatic Medicine.
Davis, M. P., Rhode, P. C., Dutton, G. R., Redmann, S. M., Ryan, D. H., & Brantley, P. J. (2006). A primary care weight management intervention for low-income African American women. Obesity, 14, 1412–1420.
Diabetes Prevention Program Research Group. (2002a). The Diabetes Prevention Program: Description of the lifestyle intervention. Diabetes Care, 25, 2165–2171.
Diabetes Prevention Program Research Group. (2002b). Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine, 346, 393–403.
Drewnowski, A., Rehm, C. D., & Solet, D. (2007). Disparities in obesity rates: Analysis by ZIP code area. Social Science and Medicine, 65, 2458–2463.
Epel, E. S., et al. (2018). More than a feeling: A unified view of stress measurement for population science. Frontiers in Neuroendocrinology, 49, 146–169.
Fitzpatrick, S. L., Brooks, N., Bray, B., & Stevens, V. J. (2019). Adherence to behavioral recommendations for weight loss and associated psychosocial factors among African American adults. Journal of Behavioral Medicine, 43, 859–864.
Föhr, T., et al. (2015). Subjective stress, objective heart rate variability-based stress, and recovery on workdays among overweight and psychologically distressed individuals: A cross-sectional study”. Journal of Occupational Medicine and Toxicology, 10, 39.
Gaalema, D., et al. (2017). Effect of socioeconomic status on propensity to change risk behaviors following myocardial infarction: Implications for healthy lifestyle. Progress in Cardiovascular Disease, 60, 159–161.
Graffagnino, C. L., Falki, J. M., & La Londe, M. (2006). Effect of a community-based weight management program on weight loss and cardiovascular disease risk factors. Obesity, 14, 280–288.
Green, M. W., Elliman, N. A., & Kretsch, M. J. (2005). Weight loss strategies, stress, and cognitive function: Supervised versus unsupervised dieting. Psychoneuroendocrinology, 30, 908–918.
Harrer, M. (2018). Effectiveness of an internet- and app-based intervention for college students with elevated stress: Randomized controlled trial. Journal of Medical Internet Research, 20, e136.
Hayes, A. F. (2019). The PROCESS Macro for SPSS and SAS. processmacro.org/faq.html.
Imayama, I., Alfano, C. M., Kong, A., Foster-Schubert, K. E., Bain, C. E., Xiao, L., Duggan, C., Wang, C. Y., Campbell, K. L., Blackburn, G. L., et al. (2011). Dietary weight loss and exercise interventions effects on quality of life in overweight/obese postmenopausal women: A randomized controlled trial. International Journal of Behavior Nutrition and Physical Activity, 8, 118–129.
Jilcott Pitts, S. B., Wu, Q., Demarest, C. L., Dixon, C. E., Dortche, C., et al. (2015). Farmers’ market shopping and dietary behaviours among Supplemental Nutrition Assistance Program participants. Public Health Nutrition, 18, 2407–2414.
Kalarchian, M. A., Levine, M. D., Klem, M. L., Burke, L. E., Soulakova, J. N., & Marcus, M. D. (2011). Impact of addressing reasons for weight loss on behavioral weight-control outcome. American Journal of Preventive Medicine, 40, 18–24.
Kim, K. H., Bursac, Z., DiLillo, V., White, D. B., & West, D. S. (2009). Stress, race, and body weight. Health Psychology, 28, 131–135.
Kumanyika, S. (2006). Nutrition and chronic disease prevention: Priorities for U.S. minority groups. Nutrition Review, 64, S9-14.
Leahey, T. M., LaRose, J. G., Mitchell, M. S., Gilder, C. M., & Wing, R. R. (2018). Small Incentives Improve Weight Loss in Women From Disadvantaged Backgrounds. American Journal of Preventive Medicine, 54, e41–e47.
Leahey, T. M., Thomas, G., Fava, J. L., Subak, L. L., Schembri, M., Krupel, K., Kumar, R., Weinberg, B., & Wing, R. R. (2014). Adding evidence-based behavioral weight loss strategies to a statewide wellness campaign: A randomized clinical trial. American Journal of Public Health, 104, 1300–1306.
Mason, A., Epel, E. S., Aschbacher, K., Lustig, R. H., Acree, M., Kristeller, J., et al. (2016). Reduced reward-drive eating accounts for the impact of a mindfulness-based diet and exercise intervention on weight loss: Data from the SHINE randomized controlled trial. Appetite, 100, 86–93.
Morin, I., Bégin, C., Maltais-Giguère, J., Bédard, A., Tchernof, A., & Lemieux, S. (2018). Impact of experimentally induced cognitive dietary restraint on eating behavior traits, appetite sensations, and markers of stress during energy restriction in overweight/obese women. Journal of Obesity, 2018, 4259389.
Ogden, C. L., Fakhouri, T. H., Carroll, M. D., Hales, C. M., Fryar, C. D., Li, X., & Freedman, D. S. (2017). Prevalence of obesity among adults, by household income and education - United States, 2011–2014. Morbidity and Mortality Weekly Report, 66, 1369–1373.
Payne, M. E., Porter Starr, K. N., Orenduff, M., Mulder, H. S., McDonald, S. R., Spira, A. P., Pieper, C. F., & Bales, C. W. (2018). Quality of life and mental health in older adults with obesity and frailty: Associations with a weight loss intervention. The Journal of Nutrition, Health & Aging, 22, 1259–1265.
Pew Research Center. (2015). Americans’ Internet access: 2000–2015. https://www.pewresearch.org/internet/2015/06/26/americans-internet-access-2000-2015/.
Rod, N. H., Gronbaek, M., Schnohr, P., Prescott, E., & Kristensen, T. S. (2009). Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: A longitudinal study. Journal of Internal Medicine, 266, 467–475.
Ryan K. K. (2014). Stress and metabolic disease. In: Committee on Population; Division of Behavioral and Social Sciences and Education, National Academies Press.
Short, M. E., Goetzel, R. Z., Pei, X., Tabrizi, M. J., Ozminkowski, R. J., Gibson, T. B., Dejoy, D. M., & Wilson, M. G. (2009). How accurate are self-reports? Analysis of self-reported health care utilization and absence when compared with administrative data. Journal of Occupational and Environmental Medicine, 51, 786–796.
Institute of Medicine (US) Committee on Health and Behavior: Research, Practice, & Policy ( 2001). Social Risk Factors. https://www.ncbi.nlm.nih.gov/books/NBK43750/
Svetkey, L. P., Stevens, V. J., Brantley, P. J., et al. (2008). Comparison of strategies for sustaining weight loss: The weight loss maintenance randomized controlled trial. Journal of the American Medical Association, 299, 1139–1148.
The George Washington University (2018). Poverty vs. Federal Poverty Level. publichealthonline.gwu.edu/blog/poverty-vs-federal-poverty-level/.
Tomiyama, A. J., Mann, T., Vinas, D., Hunger, J. M., Dejager, J., & Taylor, S. E. (2010). Low calorie dieting increases cortisol. Psychosomatic Medicine, 72, 357–364.
Torres, S. J., & Nowson, C. A. (2007). Relationship between stress, eating behavior, and obesity. Nutrition, 23, 887–894.
Trief, P. M., Cibula, D., Delahanty, L. M., & Weinstock, R. S. (2014). Depression, stress, and weight loss in individuals with metabolic syndrome in SHINE, a DPP translation study. Obesity, 22, 2532–2538.
United States Department of Agriculture (2019). WIC Policy Memorandum. fns-prod.azureedge.net/sites/default/files/resource-files/WICPolicyMemo-2019–4-WICIEGs_508.pdf.
Walvekar, S. S., Ambekar, J. G., & Devaranavadagi, B. B. (2015). Study on serum cortisol and perceived stress scale in the police constables. Journal of Clinical and Diagnostic Research, 9, BC10–BC14.
Warner, E. T., Glasgow, R. E., Emmons, K. M., Bennett, G. G., Askew, S., Rosner, B., & Colditz, G. A. (2013). Recruitment and retention of participants in a pragmatic randomized intervention trial at three community health clinics: Results and lessons learned. BMC Public Health, 13, 192–201.
Warttig, S. L., Forshaw, M. J., South, J., & White, A. K. (2013). New, normative, English-sample data for the Short Form Perceived Stress Scale (PSS-4). Journal of Health Psychology, 18, 1617–1628.
Wing, R. R., Marcus, M. D., Blair, E. H., & Burton, L. R. (1991). Psychological responses of obese type II diabetic subjects to very-low-calorie diet. Diabetes Care, 14, 596–599.
World Health Organization (2018). Obesity and Overweight. www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.
Wynd, C. A. (2006). Relaxation imagery used for stress reduction in the prevention of smoking relapse. Journal of Advanced Nursing, 17, 294–302.
Xenaki, N., Bacopoulou, F., Kokkinos, A., Nicolaides, N. C., Chrousos, G. P., & Darviri, C. (2018). Impact of a stress management program on weight loss, mental health and lifestyle in adults with obesity: a randomized controlled trial. Journal of Molecular Biochemistry, 7, 78–84.
Funding
This research was supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health (NIH) under award number R01DK111232. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no conflicts of interest to disclose.
Ethics approval and consent to participate and publish
This research involved human subjects; IRB approval and informed consent for participation and publication was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Volz, K., Wyckoff, E., Medina, T.H. et al. Impact of income and perceived stress on engagement and weight loss outcomes in an online behavioral weight loss program. J Behav Med 44, 853–859 (2021). https://doi.org/10.1007/s10865-021-00238-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-021-00238-6