Abstract
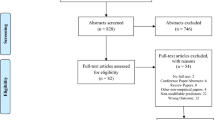
The long-term consequences of exposure to firearm injury—including suicide, assault, and mass shootings—on children’s mental and physical health is unknown. Using PRISMA-ScR guidelines, we conducted a scoping review of four databases (PubMed, Scopus, PsychINFO, and CJ abstract) between January 1, 1985 and April 2, 2018 for articles describing long-term outcomes of child or adolescent firearm injury exposure (n = 3582). Among included studies (n = 31), most used retrospective cohorts or cross-sectional studies to describe the correlation between firearm injury and post-traumatic stress. A disproportionate number of studies examined the effect of mass shootings, although few of these studies were conducted in the United States and none described the impact of social media. Despite methodologic limitations, youth firearm injury exposure is clearly linked to high rates of post-traumatic stress symptoms and high rates of future injury. Evidence is lacking on best practices for prevention of mental health and behavioral sequelae among youth exposed to firearm injury. Future research should use rigorous methods to identify prevalence, correlates, and intervention strategies for these at-risk youth.

Similar content being viewed by others
References
Affinati, S., Patton, D., Hansen, L., Ranney, M., Christmas, A. B., Violano, P., et al. (2016). Hospital-based violence intervention programs targeting adult populations: An Eastern Association for the Surgery of Trauma evidence-based review. Trauma Surgery & Acute Care Open, 1, e000024.
Alcorn, T. (2017). Trends in research publications about gun violence in the United States, 1960 to 2014. JAMA Internal Medicine, 177, 124–126.
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8, 19–32.
Bair-Merritt, M. H., Blackstone, M., & Feudtner, C. (2006). Physical health outcomes of childhood exposure to intimate partner violence: A systematic review. Pediatrics, 117, e278–e290.
Barthel, M., Shearer, E., Gottfried, J., & Mitchell, A. (2015). The evolving role of news on Twitter and Facebook. Pew Research Center, 14, 1–18.
Benson, J. E., & Elder, G. H., Jr. (2011). Young adult identities and their pathways: A developmental and life course model. Developmental Psychology, 47, 1646.
Bergman, B., Ponzer, S., & Brismar, B. (1996). Criminality and morbidity in young victims of firearm injuries: A follow-up study. Annals of the New York Academy of Sciences, 794, 334–335.
Bergström, A., & Jervelycke Belfrage, M. (2018). News in social media: Incidental consumption and the role of opinion leaders. Digital Journalism, 6, 583–598.
Betz, M. E., Ranney, M. L., & Wintemute, G. J. (2016). Frozen funding on firearm research:“Doing nothing is no longer an acceptable solution”. Western Journal of Emergency Medicine, 17, 91.
Boynton-Jarrett, R., Ryan, L. M., Berkman, L. F., & Wright, R. J. (2008). Cumulative violence exposure and self-rated health: Longitudinal study of adolescents in the United States. Pediatrics, 122, 961–970. https://doi.org/10.1542/peds.2007-3063
Brent, D. A., Perper, J. A., Moritz, G., Allman, C., Schweers, J., Roth, C., et al. (1993a). Psychiatric sequelae to the loss of an adolescent peer to suicide. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 509–517.
Brent, D. A., Perper, J., Moritz, G., Friend, A., Schweers, J., Allman, C., et al. (1993b). Adolescent witnesses to a peer suicide. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 1184–1188.
Bugge, I., Dyb, G., Stensland, S. Ø., Ekeberg, Ø., Wentzel-Larsen, T., & Diseth, T. H. (2015). Physical injury and posttraumatic stress reactions. A study of the survivors of the 2011 shooting massacre on Utøya Island, Norway. Journal of Psychosomatic Research, 79, 384–390.
Carter, P. M., Cook, L. J., Macy, M. L., Zonfrillo, M. R., Stanley, R. M., Chamberlain, J. M., et al. (2017). Individual and neighborhood characteristics of children seeking emergency department care for firearm injuries within the PECARN Network. Academic Emergency Medicine, 24, 803–813.
Carter, P. M., Walton, M. A., Roehler, D. R., Goldstick, J., Zimmerman, M. A., Blow, F. C., et al. (2015). Firearm violence among high-risk emergency department youth after an assault injury. Pediatrics, 135, 805–815. https://doi.org/10.1542/peds.2014-3572
Center for Disease Control and Prevention, C. (2014). Web-based injury statistics query and reporting systems: Fatal Injury Data (WISQARS). Retrieved from https://www.cdc.gov/injury/wisqars/fatal.html
Cheng, T. L., Wright, J. L., Markakis, D., Copeland-Linder, N., & Menvielle, E. (2008). Randomized trial of a case management program for assault-injured youth: Impact on service utilization and risk for reinjury. Pediatric Emergency Care, 24, 130–136.
Chong, V. E., Lee, W. S., & Victorino, G. P. (2015). Neighborhood socioeconomic status is associated with violent reinjury. Journal of Surgical Research, 199, 177–182.
Chong, V. E., Smith, R., Garcia, A., Lee, W. S., Ashley, L., Marks, A., et al. (2015). Hospital-centered violence intervention programs: A cost-effectiveness analysis. The American Journal of Surgery, 209, 597–603.
Council, N. R. (2013). Priorities for research to reduce the threat of firearm-related violence. Washington: National Academies Press.
Cunningham, R. M., Carter, P. M., Ranney, M., Zimmerman, M. A., Blow, F. C., Booth, B. M., et al. (2015). Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: A 2-year prospective cohort study. JAMA Pediatrics, 169, 63–70. https://doi.org/10.1001/jamapediatrics.2014.1900
Cunningham, R. M., Walton, M. A., & Carter, P. M. (2018). The major causes of death in children and adolescents in the United States. New England Journal of Medicine, 379, 2468–2475.
David-Ferdon, C., Vivolo-Kantor, A. M., Dahlberg, L. L., Marshall, K. J., Rainford, N., & Hall, J. E. (2016). A comprehensive technical package for the prevention of youth violence and associated risk behaviors (pp. 1–61). Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention.
Davis, J. S., Pandya, R. K., Sola, J. E., Perez, E. A., Neville, H. L., & Schulman, C. I. (2013). Pediatric trauma recidivism in an urban cohort. Journal of Surgical Research, 182, 326–330.
DeWolfe, D. J. (2004). Mental health response to mass violence and terrorism: A training manual. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, US Department of Health and Human Services.
Dyb, G., Jensen, T., Glad, K. A., Nygaard, E., & Thoresen, S. (2014). Early outreach to survivors of the shootings in Norway on the 22nd of July 2011. European Journal of Psychotraumatology, 5, 23523.
Finkelhor, D., Turner, H. A., Shattuck, A., & Hamby, S. L. (2015). Prevalence of childhood exposure to violence, crime, and abuse: Results from the national survey of children’s exposure to violence. JAMA Pediatrics, 169, 746–754.
Follman, M., Aronsen, G., & Pan, D. (2018). US mass shootings, 1982–2018: Data from Mother Jones’ investigation. Mother Jones.
Fowler, K. A., Dahlberg, L. L., Haileyesus, T., Gutierrez, C., & Bacon, S. (2017). Childhood firearm injuries in the United States. Pediatrics, 140, e20163486.
Fowler, P. J., Tompsett, C. J., Braciszewski, J. M., Jacques-Tiura, A. J., & Baltes, B. B. (2009). Community violence: A meta-analysis on the effect of exposure and mental health outcomes of children and adolescents. Development and Psychopathology, 21, 227–259.
Gibson, P. D., Ippolito, J. A., Shaath, M. K., Campbell, C. L., Fox, A. D., & Ahmed, I. (2016). Pediatric gunshot wound recidivism: Identification of at-risk youth. Journal of Trauma and Acute Care Surgery, 80, 877–883.
Gill, A. C. (2002). Risk factors for pediatric posttraumatic stress disorder after traumatic injury. Archives of Psychiatric Nursing, 16, 168–175.
Hafstad, G. S., Dyb, G., Jensen, T. K., Steinberg, A. M., & Pynoos, R. S. (2014). PTSD prevalence and symptom structure of DSM-5 criteria in adolescents and young adults surviving the 2011 shooting in Norway. Journal of Affective Disorders, 169, 40–46.
Hamrin, V. (1998). Psychiatric interviews with pediatric gunshot patients. Journal of Child and Adolescent Psychiatric Nursing, 11, 61–68.
Hamrin, V., Jonker, B., & Scahill, L. (2004). Acute stress disorder symptoms in gunshot-injured youth. Journal of Child and Adolescent Psychiatric Nursing, 17, 161–172.
Haravuori, H., Kiviruusu, O., Suomalainen, L., & Marttunen, M. (2016). An evaluation of ICD-11 posttraumatic stress disorder criteria in two samples of adolescents and young adults exposed to mass shootings: Factor analysis and comparisons to ICD-10 and DSM-IV. BMC Psychiatry, 16, 140.
Haravuori, H., Suomalainen, L., Berg, N., Kiviruusu, O., & Marttunen, M. (2011). Effects of media exposure on adolescents traumatized in a school shooting. Journal of Traumatic Stress, 24, 70–77.
Hawkins, N. A., McIntosh, D. N., Silver, R. C., & Holman, E. A. (2007). Early responses to school violence: A qualitative analysis of students’ and parents’ immediate reactions to the shootings at Columbine High School. Journal of Emotional Abuse, 4, 197–223.
Health, U. D. o., & Services, H. (2005). Terrorism and other public health emergencies: A reference guide for media. Washington, DC: Department of Health and Human Services.
Heinze, J. E., Reischl, T. M., Bai, M., Roche, J. S., Morrel-Samuels, S., Cunningham, R. M., et al. (2016). A comprehensive prevention approach to reducing assault offenses and assault injuries among youth. Prevention Science, 17, 167–176. https://doi.org/10.1007/s11121-015-0616-1
Higgins, J., Sterne, J., Savović, J., Page, M., Hróbjartsson, A., Boutron, I., et al. (2016). A revised tool for assessing risk of bias in randomized trials. Cochrane Database Systematic Review, 10, 29–31.
Jovanovic, T., Vance, L. A., Cross, D., Knight, A. K., Kilaru, V., Michopoulos, V., et al. (2017). Exposure to violence accelerates epigenetic aging in children. Scientific Reports, 7, 8962.
Karp, A. (2018). Estimating global civilian-held firearms numbers. Small Arms Survey.
Kümpel, A. S., Karnowski, V., & Keyling, T. (2015). News sharing in social media: A review of current research on news sharing users, content, and networks. Social Media Society, 1, 2056305115610141.
Levine, P. B., & McKnight, R. (2017). Firearms and accidental deaths: Evidence from the aftermath of the Sandy Hook school shooting. Science, 358, 1324–1328.
McGill, T., Self-Brown, S. R., Lai, B. S., Cowart, M., Tiwari, A., LeBlanc, M., et al. (2014). Effects of exposure to community violence and family violence on school functioning problems among urban youth: The potential mediating role of posttraumatic stress symptoms. Frontiers in Public Health, 2, 8.
Mercer, K. B., Orcutt, H. K., Quinn, J. F., Fitzgerald, C. A., Conneely, K. N., Barfield, R. T., et al. (2012). Acute and posttraumatic stress symptoms in a prospective gene × environment study of a university campus shooting. Archives of General Psychiatry, 69, 89–97.
Nader, K., Pynoos, R., Fairbanks, L., & Frederick, C. (1990). Children’s PTSD reactions one year after a sniper attack at their school. The American Journal of Psychiatry, 147, 1526.
Naghavi, M., Marczak, L. B., Kutz, M., Shackelford, K. A., Arora, M., Miller-Petrie, M., et al. (2018). Global mortality from firearms, 1990–2016. JAMA, 320, 792–814.
Netburn, D. (2018, November 10). The role of PTSD in mass shootings: Let’s separate myth from reality. Los Angeles Times. Retrieved from http://www.latimes.com/science/sciencenow/la-sci-sn-ptsd-mass-shootings-20181110-story.html
Olfson, M., Wall, M., Wang, S., Crystal, S., Bridge, J. A., Liu, S.-M., & Blanco, C. (2018). Suicide after deliberate self-harm in adolescents and young adults. Pediatrics, 141, e20173517.
Omar, H. A. (1999). Adolescent violence as viewed by high school students. International Journal of Adolescent Medicine and Health, 11, 153–158.
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan—A web and mobile app for systematic reviews. Systematic Reviews, 5, 210.
Ponzer, S., Bergman, B., Brismar, B., & Johansson, S. (1997). Accidental firearm injury in childhood—A predictor of social and medical outcome? European Journal of Emergency Medicine, 4, 125–129.
Pynoos, R. S., Frederick, C., Nader, K., Arroyo, W., Steinberg, A., Eth, S., et al. (1987a). Life threat and posttraumatic stress in school-age children. Archives of General Psychiatry, 44, 1057–1063.
Pynoos, R. S., Nader, K., Frederick, C., Gonda, L., & Stuber, M. (1987b). Grief reactions in school age children following a sniper attack at school. Israel Journal of Psychiatry and Related Sciences, 24, 53–63.
Rand Corporation. (2018). Mass shootings: Definitions and trends. Retrieved from https://www.rand.org/research/gun-policy/analysis/supplementary/mass-shootings.html
Ranney, M. L., Fletcher, J., Alter, H., Barsotti, C., Bebarta, V. S., Betz, M. E., et al. (2017). A consensus-driven agenda for emergency medicine firearm injury prevention research. Annals of Emergency Medicine, 69, 227–240. https://doi.org/10.1016/j.annemergmed.2016.08.454
Roche, J. S., Clery, M. J., Carter, P. M., Dora-Laskey, A., Walton, M. A., Ngo, Q. M., et al. (2018). Tracking assault-injured, drug-using youth in longitudinal research: Follow-up methods. Academic Emergency Medicine, 25, 1204–1215.
Rowhani-Rahbar, A., Zatzick, D., Wang, J., Mills, B. M., Simonetti, J. A., Fan, M. D., et al. (2015). Firearm-related hospitalization and risk for subsequent violent injury, death, or crime perpetration: A cohort study. Annals of Internal Medicine, 162, 492–500.
Samuelson, K. W., Wilson, C. K., Padrón, E., Lee, S., & Gavron, L. (2017). Maternal PTSD and children’s adjustment: Parenting stress and emotional availability as proposed mediators. Journal of Clinical Psychology, 73, 693–706.
Santiago, P. N., Ursano, R. J., Gray, C. L., Pynoos, R. S., Spiegel, D., Lewis-Fernandez, R., et al. (2013). A systematic review of PTSD prevalence and trajectories in DSM-5 defined trauma exposed populations: Intentional and non-intentional traumatic events. PLoS ONE, 8, e59236.
Schneider, S. J., Grilli, S. F., & Schneider, J. R. (2013). Evidence-based treatments for traumatized children and adolescents. Current Psychiatry Reports, 15, 332.
Schwarz, E. D., & Kowalski, J. M. (1991). Malignant memories: PTSD in children and adults after a school shooting. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 936–944.
Shih, R. A., Schell, T. L., Hambarsoomian, K., Marshall, G. N., & Belzberg, H. (2010). Prevalence of PTSD and major depression following trauma-center hospitalization. The Journal of Trauma, 69, 1560.
Shultz, J. M., Muschert, G. W., Dingwall, A., & Cohen, A. M. (2013). The Sandy Hook Elementary School shooting as tipping point: “This Time Is Different”. Disaster Health, 1, 65–73.
Slovak, K., & Singer, M. (2001). Gun violence exposure and trauma among rural youth. Violence and Victims, 16, 389.
Song, J. W., & Chung, K. C. (2010). Observational studies: Cohort and case-control studies. Plastic and Reconstructive Surgery, 126, 2234.
Spicer, R. S., & Miller, T. R. (2000). Suicide acts in 8 states: Incidence and case fatality rates by demographics and method. American Journal of Public Health, 90, 1885.
Srinivasan, S., Mannix, R., & Lee, L. K. (2014). Epidemiology of paediatric firearm injuries in the USA, 2001–2010. Archives of Disease in Childhood, 99, 331–335.
Stark, D. E., & Shah, N. H. (2017). Funding and publication of research on gun violence and other leading causes of death. JAMA, 317, 84–85.
Stene, L. E., & Dyb, G. (2015). Health service utilization after terrorism: A longitudinal study of survivors of the 2011 Utøya attack in Norway. BMC Health Services Research, 15, 158.
Stensland, S. Ø., Zwart, J.-A., Wentzel-Larsen, T., & Dyb, G. (2018). The headache of terror: A matched cohort study of adolescents from the Utøya and the HUNT Study. Neurology, 90, e111–e118.
Sterne, J. A., Hernán, M. A., Reeves, B. C., Savović, J., Berkman, N. D., Viswanathan, M., et al. (2016). ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ, 355, i4919.
Suomalainen, L., Haravuori, H., Berg, N., Kiviruusu, O., & Marttunen, M. (2011). A controlled follow-up study of adolescents exposed to a school shooting—Psychological consequences after four months. European Psychiatry, 26, 490–497.
Talley, C. L., Campbell, B. T., Jenkins, D. H., Barnes, S. L., Sidwell, R. A., Timmerman, G., et al. (2018). Recommendations from the American College of Surgeons Committee on Trauma’s Firearm Strategy Team (FAST) Workgroup: Chicago Consensus I. Journal of the American College of Surgeons, 228, 198–206.
Tellez, M. G., Mackersie, R. C., Morabito, D., Shagoury, C., & Heye, C. (1995). Risks, costs, and the expected complication of re-injury. The American Journal of Surgery, 170, 660–664.
The National Institute of Mental Health. (2017). Strategic Research Priorities Overview. Transforming the understanding and treatment of mental illnesses. Retrieved from https://www.nimh.nih.gov/about/strategic-planning-reports/strategic-research-priorities/index.shtml
Thoresen, S., Jensen, T. K., Wentzel-Larsen, T., & Dyb, G. (2016). Parents of terror victims. A longitudinal study of parental mental health following the 2011 terrorist attack on Utøya Island. Journal of Anxiety Disorders, 38, 47–54.
Walton, M. A., Chermack, S. T., Shope, J. T., Bingham, C. R., Zimmerman, M. A., Blow, F. C., et al. (2010). Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. JAMA, 304, 527–535. https://doi.org/10.1001/jama.2010.1066
Wanner, J. P. (2015). Development of a trauma-specific quality of life measurement. The Journal of Trauma and Acute Care Surgery, 79, 275.
Wise, A. E., & Delahanty, D. L. (2017). Parental factors associated with child post-traumatic stress following injury: A consideration of intervention targets. Frontiers in Psychology, 8, 1412.
Zatzick, D., Jurkovich, G., Rivara, F. P., Russo, J., Wagner, A., Wang, J., et al. (2013). A randomized stepped care intervention trial targeting posttraumatic stress disorder for surgically hospitalized injury survivors. Annals of Surgery, 257, 390.
Acknowledgements
The authors wish to acknowledge Lynn Massey for assistance with the literature search, organizing data abstraction, and manuscript preparation. We would also like to acknowledge Gurpreet Kaur Rana, Informationist at the Taubman Health Sciences Library, University of Michigan, for creating the search strategies for the scoping review; and Zahra Asghar for her assistance with initial literature reviews.
Funding
This review was funded by NIH/NICHD 1R24HD087149-01A1. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the funding agencies.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Megan Ranney, Rebecca Karb, Peter Ehrlich, Kira Bromwich, Rebecca Cunningham, Rinad S. Beidas, for the FACTS Consortium declares that they have no conflict of interest.
Human and animal rights and Informed Consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix: PubMed search strategy
Appendix: PubMed search strategy
Date Searched: April 2, 2018
Final number of results: 590
(((((gun[tiab] OR guns[tiab] OR handgun*[tiab] OR firearm*[tiab] OR firearms[MeSH Terms] OR gunshot*[tiab] OR shooting*[tiab] OR “gun violence”[tiab] OR “gun safety”[tiab]))) AND ((“wounds, gunshot”[MeSH Terms] OR “Wounds and Injuries”[Mesh] OR injury[tiab] OR injuries[tiab] OR mortality[tiab] OR intentional[tiab] OR unintentional[tiab] OR accidental[tiab] OR accident*[tiab]))) AND ((adolescent[MeSH Terms] OR youth[MeSH Terms] OR child[MeSH Terms] OR teenager[Title/Abstract] OR teen[Title/Abstract] OR adolescen*[Title/Abstract] OR child[Title/Abstract] OR youth[title/abstract] OR children[Title/Abstract] OR minor[Title/Abstract] OR minors[title/abstract] OR delinquent[Title/Abstract] OR delinquency[Title/Abstract] OR pediatric*[Title/Abstract] OR parent*[tiab]))) AND (“Recurrence”[Mesh] OR recurren*[tiab] OR “Recidivism”[Mesh] OR recidivism[tiab] OR “Follow-Up Studies”[Mesh] OR “follow-up”[tiab] OR “follow up”[tiab] OR “Exposure to Violence”[Mesh] OR “Life Change Events”[Mesh] OR “Patient Readmission”[Mesh] OR readmission[tiab] OR rehospitalization[tiab] OR “Secondary Prevention”[Mesh] OR “Tertiary Prevention”[Mesh] OR psychosocial[tiab] OR “Mental Health Services”[Mesh] OR “criminal justice” OR “Prisons”[Mesh] OR incarceration[tiab] OR imprisonment[tiab] OR detention[tiab] OR custody[tiab] OR subsequent[tiab])Filters: Publication date from 1985/01/01 to 2018/12/31.
Filters: Publication date from 1985/01/01 to 2018/04/01
Rights and permissions
About this article
Cite this article
Ranney, M., Karb, R., Ehrlich, P. et al. What are the long-term consequences of youth exposure to firearm injury, and how do we prevent them? A scoping review. J Behav Med 42, 724–740 (2019). https://doi.org/10.1007/s10865-019-00035-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-019-00035-2