Abstract
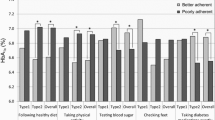
This study examined how Dutch type 1 and type 2 diabetes patients’ perceived autonomy support, as well as their perceived competence and treatment self-regulation, are associated with their diabetes self-care activities (healthy diet, physical activity, monitoring blood glucose, medication use) and general diabetes control. A cross-sectional questionnaire study was conducted among 143 type 1 diabetics and 384 type 2 diabetics. Overall, participants felt competent, supported in their autonomy, and perceived to autonomously self-regulate their diabetes. Our results underline the importance of perceived competence in type 1 and 2 diabetics, as this was strongly associated with adhering to a healthy diet and general diabetes control. Our findings also emphasize the need for autonomy supportive health care professionals in diabetes care. Interestingly, perceived competence partially mediated the influence of autonomy support on general diabetes control.
Similar content being viewed by others
References
American Diabetes Association. (2013). Standards of medical care in diabetes-2013. Diabetes Care, 136, S11–S66.
Baan, C. A., & Poos, M. J. J. C. (2013). Hoe vaak komt diabetes mellitus voor en hoeveel mensen sterven eraan? [How often does diabetes occur and how many people die from it?] In: VTV public health forecast, National Public Health Compass. Bilthoven: National Institute for Public Health and the Environment.
Barlow, J., Wright, C., Sheasby, J., Turner, A., & Hainsworth, J. (2002). Self-management approaches for people with chronic conditions: A review. Patient Education and Counseling, 48, 177–187. doi:10.1016/s0738-3991(02)00032-0
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182.
Central Committee on Research inv. Human subjects. http://www.ccmo-online.nl/main.asp?pid=1
Chen, S. M., Creedy, D., Lin, H. S., & Wollin, J. (2012). Effects of motivational interviewing intervention on self-management, psychological and glycemic outcomes in type 2 diabetes: A randomized controlled trial. International Journal of Nursing Studies, 49, 637–644.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. New York: Academic Press.
Deci, E. L., & Ryan, R. M. (2012). Self-determination theory in health care and its relations to motivational interviewing: A few comments. The international Journal of Behavioral Nutrition and Physical Activity, 9, 24.
EADV, & NAD. (2012). From indication to execution. A multidisciplinary guideline for selfcontrol of blood glucose by diabetes patients. [Van indicatiestelling naar uitvoering. Een multidisciplinaire richtlijn over zelfcontrole van bloedglucosewaarden door mensen met diabetes.] Utrecht: EADV & NAD.
International Diabetes Federation. (2012). Diabetes atlas update 2012: International Diabetes Federation. http://www.idf.org/sites/default/files/5E_IDFAtlasPoster_2012_EN.pdf
Janevic, M. R., McLaughlin, S. J., & Connell, C. M. (2012). Overestimation of physical activity among a nationally representative sample of underactive individuals with diabetes. Medical Care, 50, 441–445.
Lundahl, B., Moleni, T., Burke, B. L., Butters, R., Tollefson, D., Butler, C., & Rollnick, S. (2013). Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Education and Counseling, 93, 157–168.
Malanda, U. L., Welschen, L. M., Riphagen, II, Dekker, J. M., Nijpels, G., & Bot, S. D. (2012). Self-monitoring of blood glucose in patients with type 2 diabetes mellitus who are not using insulin. Cochrane Database of Systematic Reviews, 1, CD005060.
Markland, D., Ryan, R. M., Tobin, V. J., & Rollnick, S. (2005). Motivational interviewing and self-determination theory. Journal of Social and Clinical Psychology, 24, 811–831.
Meis, J. J., Kremers, S. P., & Bouman, M. P. (2012). Television viewing does not have to be sedentary: Motivation to participate in a TV exercise program. Journal of Obesity, 2012, 752820.
National Institute for Public Health and the Environment. (2011). ‘Nederland de maat genomen 2009–2012’. Monitoring van risicofactoren in de algemene bevolking. [‘Nederland de maat genomen 2009–2010’. Monitoring of risk factors in the general population.] Bilthoven: National Institute for Public Health and the Environment.
Netherlands Diabetes Federation. (2007). NDF Zorgstandaard. Transparantie en kwaliteit van diabeteszorg voor mensen met diabetes type 2. [NDF Care Standard. Transparacny and quality of diabetescare for people with diabetes type 2.] Amersfoort: Netherlands Diabetes Federation.
Ng, J. Y. Y., Ntoumanis, N., Thøgersen-Ntoumani, C., Deci, E. L., Ryan, R. M., Duda, J. L., & Williams, G. C. (2012). Self-determination theory applied to health contexts: A meta-analysis. Perspectives on Psychological Science, 7, 325.
Norris, S. L., Engelgau, M. M., & Narayan, K. M. (2001). Effectiveness of self-management training in type 2 diabetes: A systematic review of randomized controlled trials. Diabetes Care, 24, 561–587.
Pollak, K. I., Alexander, S. C., Tulsky, J. A., Lyna, P., Coffman, C. J., Dolor, R. J., & Ostbye, T. (2011). Physician empathy and listening: Associations with patient satisfaction and autonomy. The Journal of the American Board of Family Medicine, 24, 666–674.
Reed, J. A., Ashton, H., Hollinghurst, S., & Higgs, E. R. (2003). Diabetes self management: How are we doing? Practical Diabetes International, 20, 318–322.
Resnicow, K., & McMaster, F. (2012). Motivational Interviewing: Moving from why to how with autonomy support. The international Journal of Behavioral Nutrition and Physical Activity, 9, 19.
Ryan, R. M., & Deci, E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychology, 55, 68–78.
Senecal, C., Nouwen, A., & White, D. (2000). Motivation and dietary self-care in adults with diabetes: Are self-efficacy and autonomous self-regulation complementary or competing constructs? Health Psychology, 19, 452–457.
Shigaki, C., Kruse, R. L., Mehr, D., Sheldon, K. M., Bin, G., Moore, C., & Lemaster, J. (2010). Motivation and diabetes self-management. Chronic Illness, 6, 202–214.
Sobel, M. E. (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology, 13, 290–312.
Toobert, D. J., Hampson, S. E., & Glasgow, R. E. (2000). The sunmmary of diabetes self-care activities measure. Diabetes Care, 23, 943–950.
Vansteenkiste, M., Williams, G. C., & Resnicow, K. (2012). Toward systematic integration between self-determination theory and motivational interviewing as examples of top-down and bottom-up intervention development: Autonomy or volition as a fundamental theoretical principle. International Journal of Behavioral Nutrition and Physical Activity, 9(23), 1–11.
Verweij, A. (2008). Scholing en opleiding: Indeling opleidingsniveau. [Education and training: categorization of educational levels]. Bilthoven: National Institute for Public Health and the Environment.
Williams, G. C., Freedman, Z. R., & Deci, E. L. (1998a). Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care, 21, 1644–1651.
Williams, G. C., Gagné, M., Mushlin, A. I., & Deci, E. L. (2002a). Motivation for behavior change in patients with chest pain. Health Education Research, 105, 304–321.
Williams, G. C., Gagne, M., Ryan, R. M., & Deci, E. L. (2002b). Facilitating autonomous motivation for smoking cessation. Health Psychology, 21, 40–50.
Williams, G. C., Grow, V. M., Freedman, Z., Ryan, R. M., & Deci, E. L. (1996). Motivational predictors of weight loss and weight-loss maintenance. Journal of Personality and Social Psychology, 70, 115–126.
Williams, G. C., McGregor, H. A., King, D., Nelson, C. C., & Glasgow, R. E. (2005). Variation in perceived competence, glycemic control, and patient satisfaction: Relationship to autonomy support from physicians. Patient Education and Counseling, 57, 39–45.
Williams, G. C., McGregor, H. A., Zeldman, A., Freedman, Z. R., & Deci, E. L. (2004). Testing a self-determination theory process model for promoting glycemic control through diabetes self-management. Health Psychology, 23, 58–66.
Williams, G. C., Patrick, H., Niemiec, C. P., Williams, L. K., Divine, G., Lafata, J. E., & Pladevall, M. (2009). Reducing the health risks of diabetes: How self-determination theory may help improve medication adherence and quality of life. Diabetes Education, 35, 484–492.
Williams, G. C., Rodin, G. C., Ryan, R. M., Grolnick, W. S., & Deci, E. L. (1998b). Autonomous regulation: the motivational basis of adherence to medical regimens. Health Psychology, 17, 269–276.
World Health Organization. (2011). BMI classification. from http://apps.who.int/bmi/index.jsp?introPage=intro_3.html
World Health Organization. (2013). Factsheet diabetes. http://www.who.int/mediacentre/factsheets/fs312/en/index.html
Windows, I. S. S. F. (Version 20.0). In I. Corporation (Ed.). Armonk, New York.
Acknowledgments
This study was conducted as part of the Dutch National Diabetes Action Program with a Grant from the Diabetes Federation (Project Number 2010.105.1356).
Conflict of interest
L. Raaijmakers, M. Martens, L. Bagchus, I. de Weerdt, S. Kremers & N. de Vries declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raaijmakers, L.G.M., Martens, M.K., Bagchus, C. et al. Correlates of perceived self-care activities and diabetes control among Dutch type 1 and type 2 diabetics. J Behav Med 38, 450–459 (2015). https://doi.org/10.1007/s10865-014-9609-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10865-014-9609-y