Abstract
Objective
To evaluate the clinical outcomes of reconstruction of maxillary class III defect using 3D-printed titanium mesh.
Methods
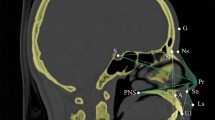
Twelve patients with maxillary class III defect from April 2015 to December 2016 were retrospectively studied. A 3D individualized maxillary stereo model based on mirror images of the unaffected maxilla was obtained to fabricate an anatomically adapted titanium mesh using computer-assisted design and manufacture. The individual titanium mesh was inserted into the maxillary class III defect after total maxillectomy. The incidence of postoperative complications was evaluated. The postoperative orbital volume and protrusion degree of eye were measured.
Results
All patients were satisfied with their postoperative facial symmetry, without developing diplopia or endophthalmos. The postoperative orbital volumes were 26.41 ± 0.52 mL on the affected side and 26.55 ± 0.45 mL on the unaffected side. The postoperative protrusion degrees of affected and unaffected eyes were 16.21 ± 0.48 and 16.82 ± 0.79 mm, respectively. Titanium mesh exposure was observed in 2 patients and mild limitation of mouth opening was observed in 4 patients who underwent postoperative radiotherapy.
Conclusion
Reconstruction of maxillary class III defect with 3D-printed titanium mesh can achieve successful clinical outcomes, which recovered orbital volume and protrusion degree of eye.

Twelve patients with maxillary class III defect were satisfied with their postoperative facial symmetry, without developing diplopia or endophthalmos. We investigated that reconstruction of maxillary class III defect with 3D-printed titanium mesh can achieve successful clinical outcomes.




Similar content being viewed by others
References
Brown JS, Rogers SN, McNally DN, Boyle M. A modified classification for the maxillectomy defect. Head Neck. 2000;22:17–26.
Brown JS, Shaw RJ. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol. 2010;11:1001–8.
Lenox ND, Kim DD. Maxillary reconstruction. Oral Maxillofac Surg Clin North Am. 2013;25:215–22.
Witjes MJH, Schepers RH, Kraeima J. Impact of 3D virtual planning on reconstruction of mandibular and maxillary surgical defects in head and neck oncology. Curr Opin Otolaryngol Head Neck Surg. 2018;26:108–14.
Roy AA, Efanov JI, Mercier-Couture G, Chollet A, Borsuk DE. Zygomatico-maxillary reconstruction with computer-aided manufacturing of a free DCIA osseous flap and intraoral anastomoses. Plast Reconstr Surg Glob Open. 2017;5:e1226.
Sharaf MY, Ibrahim SI, Eskander AE, Shaker AF. Prosthetic versus surgical rehabilitation in patients with maxillary defect regarding the quality of life: systematic review. Oral Maxillofac Surg. 2018;22:1–11.
Sotsuka Y, Fujiwara T, Kawai K, Nishimoto S, Kakibuchi M. Bilateral maxillary reconstruction using fibular flap in bisphosphonate-related osteonecrosis. Plast Reconstr Surg Glob Open. 2016;4:e1045.
Trinh BB, French B, Khechoyan DY, Deleyiannis FW. Designing a fibular flow-through flap with a proximal peroneal perforator-free flap for maxillary reconstruction. Plast Reconstr Surg Glob Open. 2017;5:e1543.
Chen C, Ren W, Gao L, Cheng Z, Zhang L, Li S, Zhi PK. Function of obturator prosthesis after maxillectomy and prosthetic obturator rehabilitation. Braz J Otorhinolaryngol. 2016;82:177–83.
Kreeft AM, Krap M, Wismeijer D, Speksnijder CM, Smeele LE, Bosch SD, Muijen MS, Balm AJ. Oral function after maxillectomy and reconstruction with an obturator. Int J Oral Maxillofac Surg. 2012;41:1387–92.
Shan XF, Chen HM, Liang J, Huang JW, Cai ZG. Surgical reconstruction of maxillary and mandibular defects using a printed titanium mesh. J Oral Maxillofac Surg. 2015;73:1437 e1431–9.
Diaconu SC, Dreizin D, Uluer M, Mossop C, Grant MP, Nam AJ. The validity and reliability of computed tomography orbital volume measurements. J Craniomaxillofac Surg. 2017;45:1552–7.
Denion E, Hitier M, Guyader V, Dugue AE, Mouriaux F. Unique human orbital morphology compared with that of apes. Sci Rep. 2015;5:11528.
Karti O, Selver OB, Karahan E, Zengin MO, Uyar M. The effect of age, gender, refractive status and axial length on the measurements of hertel exophthalmometry. Open Ophthalmol J. 2015;9:113–5.
Iyer S, Thankappan K. Maxillary reconstruction: current concepts and controversies. Indian J Plast Surg. 2014;47:8–19.
Motiee-Langroudi M, Harirchi I, Amali A, Jafari M. Reconstruction of midface and orbital wall defects after maxillectomy and orbital content preservation with titanium mesh and fascia lata: 3-year follow-up. J Oral Maxillofac Surg. 2015;73:2447 e2441–5.
Janecka IP. New reconstructive technologies in skull base surgery: role of titanium mesh and porous polyethylene. JAMA Otolaryngol–Head Neck Surg. 2000;126:396–401.
Tarsitano A, Battaglia S, Ciocca L, Scotti R, Cipriani R, Marchetti C. Surgical reconstruction of maxillary defects using a computer-assisted design/computer-assisted manufacturing-produced titanium mesh supporting a free flap. J Cranio-Maxillofac Surg. 2016;44:1320–6.
Shengwei H, Zhiyong W, Qingang H, Wei H. Combined use of an anterolateral thigh flap and rapid prototype modeling to reconstruct maxillary oncologic resections and midface defects. J Craniofac Surg. 2014;25:1147–9.
Funding
This study was supported by the National Natural Science Foundation of China (81500872), Natural Science Foundation of Jiangsu Province (BK20161389), Young Medical Talent Foundation of Jiangsu Province (QNRC2016906), and Six talent peaks project in Jiangsu Province (2016-WSW-093), National Postdoctoral Foundation (2016M593040).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, By., Cao, G., Dong, Z. et al. The application of 3D-printed titanium mesh in maxillary tumor patients undergoing total maxillectomy. J Mater Sci: Mater Med 30, 125 (2019). https://doi.org/10.1007/s10856-019-6326-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-019-6326-7