Abstract
Purpose
The demand for titanium dental implants has risen sharply. However, the clinical success rate of implant surgery needs to be improved. In this paper, we report a novel surface modification strategy, large-grit sandblasting combined with micro-arc oxidation (SL-MAO), aiming to promote peri-implant bone formation and osseointegration of titanium implants.
Materials and methods
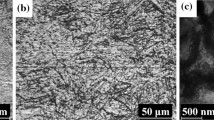
Modified titanium samples were prepared by large-grit sandblasting and acid etching (SLA), micro-arc oxidation (MAO), and SL-MAO. The resulting topographical changes and chemical composition of the samples were examined by scanning electron microscopy (SEM) and energy-dispersive X-ray spectroscopy (EDS), respectively, and the biocompatibility and bioactivity were analyzed by bone-marrow mesenchymal stem cells (BMMSC) adhesion tests. Modified titanium implants were also inserted into the femurs of beagle dogs, and their competence of osseointegration was appraised by quantitative histomorphometry and micro-computed-tomography (micro-CT) analyses.
Results
Compared to SLA and MAO techniques, SL-MAO surface modification further enhanced titanium surfaces by creating a topographic morphology characterized by both micron-sized craters and sub-micron-scale pits, and resulted in superior chemical composition, which promoted cell adhesion, proliferation, and osteogenic differentiation. SL-MAO-modified titanium implants osseointegrated more efficiently than SLA or MAO controls, with significantly higher bone-area (BA) ratio and bone-implant contact (BIC) in the peri-implant region.
Conclusions
The SL-MAO surface modification technique optimized the surface properties of titanium implants and enhanced peri-implant bone formation and osseointegration.





Similar content being viewed by others
References
Byrne G. There is not an optimum number of implants for an overdenture. J Am Dent Assoc. 2015;146:773–4.
Albrektsson T, Canullo L, Cochran D, De Bruyn H. “Peri-Implantitis”: a complication of a foreign body or a man-made “disease”. Facts and fiction. Clin Implant Dent Relat Res. 2016;18:840–9.
Piccinini M, Cugnoni J, Botsis J, Ammann P, Wiskott A. Peri-implant bone adaptations to overloading in rat tibiae: experimental investigations and numerical predictions. Clin Oral Implants Res. 2016;27:1444–53.
Neves J, de Araújo Nobre M, Oliveira P, Martins Dos Santos J, Malo P. Risk factors for implant failure and peri-implant pathology in systemic compromised patients. J Prosthodont. 2018;27:409–15.
Poli PP, Beretta M, Grossi GB, Maiorana C. Risk indicators related to peri-implant disease: an observational retrospective cohort study. J Periodontal Implant Sci. 2016;46:266–76.
Jin Y, Xu L, Hu X, Liao S, Pathak JL, Liu J. Lithium chloride enhances bone regeneration and implant osseointegration in osteoporotic conditions. J bone miner metab. 2017;35:497–503.
Cha JY, Pereira MD, Smith AA, Houschyar KS, Yin X, Mouraret S, et al. Multiscale analyses of the bone-implant interface. J Dent Res. 2015;94:482–90.
Yin X, Li J, Chen T, Mouraret S, Dhamdhere G, Brunski JB, et al. Rescuing failed oral implants via Wnt activation. J Clin Periodontol. 2016;43:180–92.
Lee HJ, Lee J, Lee JT, Hong JS, Lim BS, Park HJ, et al. Microgrooves on titanium surface affect peri-implant cell adhesion and soft tissue sealing; an in vitro and in vivo study. J Periodontal Implant Sci. 2015;45:120–6.
Xie L, Liao X, Yin G, Huang Z, Yan D, Yao Y, et al. Preparation, characterization, in vitro bioactivity, and osteoblast adhesion of multi-level porous titania layer on titanium by two-step anodization treatment. J Biomed Mater Res Part A. 2011;98:312–20.
Gasik M, Braem A, Chaudhari A, Duyck J, Vleugels J. Titanium implants with modified surfaces: meta-analysis of in vivo osteointegration. Mater Sci Eng C Mater Biol Appl. 2015;49:152–8.
Kammerer TA, Palarie V, Schiegnitz E, Topalo V, Schroter A, Al-Nawas B, et al. A biphasic calcium phosphate coating for potential drug delivery affects early osseointegration of titanium implants. J Oral Pathol Med. 2017;46:61–6.
Karaji ZG, Houshmand B, Faghihi S. Surface modification of porous titanium granules for improving bioactivity. Int J Oral Maxillofac Implants. 2016;31:1274–80.
Sahrmann P, Mohn D, Zehnder M, Stark WJ, Imfeld T, Weber FE. Effect of direct current on surface structure and cytocompatibility of titanium dental implants. Int J Oral Maxillofac Implants. 2014;29:735–42.
Guo Z, Zhou L, Rong M, Ding J, Zhu A, Li S, et al. Bone augmentation in a titanium cap with a porous surface modified by microarc oxidation. Int J Oral Maxillofac Implants. 2013;28:767–73.
Guo Z, Zhou L, Rong M, Zhu A, Geng H. Bone response to a pure titanium implant surface modified by laser etching and microarc oxidation. Int J Oral Maxillofac Implants. 2010;25:130–6.
Liu CG, Han HY, Zhang JT, Kankala RK, Wang SB, Chen AZ. Rerouting engineered metal-dependent shapes of mesoporous silicananocontainers to biodegradable Janus-type (sphero-ellipsoid) nanoreactorsfor chemodynamic therapy. Chem Eng J. 2019;370:1188–99.
Chen BQ, Kankala RK, Chen AZ, Yang DZ, Cheng XX, Jiang NN, et al. Investigation of silk fibroin nanoparticle-decorated poly(l-lactic acid) composite scaffolds for osteoblast growth and differentiation. Int J Nanomed. 2017;12:1877–90.
Kankala RK, Zhang YS, Wang SB. et al. Supercritical fluid technology: an emphasis on drug delivery and related biomedical applications. Adv Healthc Mater. 2017;6:1700433
Szmukler-Moncler S, Perrin D, Ahossi V, Magnin G, Bernard JP. Biological properties of acid etched titanium implants: effect of sandblasting on bone anchorage. J Biomed Mater Res Part B Appl Biomater. 2004;68:149–59.
Chung CJ, Long HY. Systematic strontium substitution in hydroxyapatite coatings on titanium via micro-arc treatment and their osteoblast/osteoclast responses. Acta Biomater. 2011;7:4081–7.
Sul YT, Johansson CB, Jeong Y, Roser K, Wennerberg A, Albrektsson T. Oxidized implants and their influence on the bone response. J Mater Sci Mater Med. 2001;12:1025–31.
Şimşek S, Özeç İ, Kürkçü M, Benlidayı E. Histomorphometric Evaluation of bone formation in peri-implant defects treated with different regeneration techniques: an experimental study in a rabbit model. J Oral Maxillofac Surg. 2016;74:1757–64.
Li Y, Li Q, Zhu S, Luo E, Li J, Feng G, et al. The effect of strontium-substituted hydroxyapatite coating on implant fixation in ovariectomized rats. Biomaterials. 2010;31:9006–14.
Gabet Y, Muller R, Levy J, Dimarchi R, Chorev M, Bab I, et al. Parathyroid hormone 1-34 enhances titanium implant anchorage in low-density trabecular bone: a correlative micro-computed tomographic and biomechanical analysis. Bone. 2006;39:276–82.
Li P, Tong Z, Huo L, Yang F, Su W. Antibacterial and biological properties of biofunctionalized nanocomposites on titanium for implant application. J Biomater Appl. 2016;31:205–14.
Le Guehennec L, Soueidan A, Layrolle P, Amouriq Y. Surface treatments of titanium dental implants for rapid osseointegration. Dent Mater. 2007;23:844–54.
Chang JZ, Chen YJ, Tung YY, Chiang YY, Lai EH, Chen WP, et al. Effects of thread depth, taper shape, and taper length on the mechanical properties of mini-implants. Am J Orthod Dentofac Orthop. 2012;141:279–88.
Cunha AC, Freitas AO, Marquezan M, Nojima LI Mechanical influence of thread pitch on orthodontic mini-implant stability. Braz Oral Res. 2015;29:42.
Ma P, Xiong W, Tan B, Geng W, Liu J, Li W, et al. Influence of thread pitch, helix angle, and compactness on micromotion of immediately loaded implants in three types of bone quality: a three-dimensional finite element analysis. Biomed Res Int. 2014;2014:983103.
Becker W, Becker BE, Ricci A, Bahat O, Rosenberg E, Rose LF, et al. A prospective multicenter clinical trial comparing one- and two-stage titanium screw-shaped fixtures with one-stage plasma-sprayed solid-screw fixtures. Clin Implant Dent Relat Res. 2000;2:159–65.
Masaki C, Schneider GB, Zaharias R, Seabold D, Stanford C. Effects of implant surface microtopography on osteoblast gene expression. Clin Oral Implants Res. 2005;16:650–6.
Schwartz Z, Nasazky E, Boyan BD. Surface microtopography regulates osteointegration: the role of implant surface microtopography in osteointegration. Alpha Omegan. 2005;98:9–19.
Hansson S, Norton M. The relation between surface roughness and interfacial shear strength for bone-anchored implants. A mathematical model. J Biomech. 1999;32:829–36.
Jager M, Zilkens C, Zanger K, Krauspe R. Significance of nano- and microtopography for cell-surface interactions in orthopaedic implants. J Biomed Biotechnol. 2007;2007:69036.
Webster TJ, Ergun C, Doremus RH, Siegel RW, Bizios R. Specific proteins mediate enhanced osteoblast adhesion on nanophase ceramics. J Biomed Mater Res. 2000;51:475–83.
Wei D, Zhou Y, Jia D, Wang Y. Characteristic and in vitro bioactivity of a microarc-oxidized TiO(2)-based coating after chemical treatment. Acta Biomater. 2007;3:817–27.
Acknowledgements
We thank Prof. Guangfu Yin and colleagues from College of Materials Science and Engineering, Sichuan University, who provided technical support and contributed to this work. This work was supported by Key Research and Development Project and Applied Basic Research Programs of Science and Technology Department Foundation of Sichuan Province (Grant No. 2019YFS0358 and 2018JY0139), National Natural Science Foundation of China (81801019), Sichuan University Postdoctoral Research Fund (2018SCU12020) and West China Hospital of Stomatology Sichuan University (WCHS-201702).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
He, W., Yin, X., Xie, L. et al. Enhancing osseointegration of titanium implants through large-grit sandblasting combined with micro-arc oxidation surface modification. J Mater Sci: Mater Med 30, 73 (2019). https://doi.org/10.1007/s10856-019-6276-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-019-6276-0