Abstract
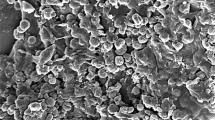
Silver-based products have been proven to be effective in retarding and preventing bacterial growth since ancient times. In the field of restorative dentistry, the use of silver ions/nanoparticles has been explored to counteract bacterial infections, as silver can destroy bacterial cell walls by reacting with membrane proteins. However, it is also cytotoxic towards eukaryotic cells, which are capable of internalizing nanoparticles. In this work, we investigated the biological effects of Chitlac-nAg, a colloidal system based on a modified chitosan (Chitlac), administered for 24–48 h to a co-culture of primary human gingival fibroblasts and Streptococcus mitis in the presence of saliva, developed to mimic the microenvironment of the oral cavity. We sought to determine its efficiency to combat oral hygiene-related diseases without affecting eukaryotic cells. Cytotoxicity, reactive oxygen species production, apoptosis induction, nanoparticles uptake, and lysosome and autophagosome metabolism were evaluated. In vitro results show that Chitlac-nAg does not exert cytotoxic effects on human gingival fibroblasts, which seem to survive through a homoeostasis mechanism involving autophagy. That suggests that the novel biomaterial Chitlac-nAg could be a promising tool in the field of dentistry.






Similar content being viewed by others
References
Yalpani M, Hall LD. Some chemical and analytical aspects of polysaccharide modifications. Formation of branched-chain, soluble chitosan derivatives. Macromolecules. 1984;17:272–81.
Jones DS, Mawhinney HJ. Chitosan. In: Row RC, Sheskey PJ, Quinn ME, editors. Handbook of Pharmaceutical Excipients. New York: American Pharmacists Association and The Pharmaceutical Press; 2009. p. 159–61.
Prabaharan M, Mano JF. Chitosan-based particles as controlled drug delivery systems. Drug Deliv. 2005;12:41–57.
Donati I, Stredanska S, Silvestrini G, Vetere A, Marcon P, Marsich E, Mozetic P, Gamini A, Paoletti S, Vittur F. The aggregation of pig articular chondrocyte and synthesis of extracellular matrix by a lactose-modified chitosan. Biomaterials. 2005;26:987–9.
Marcon P, Marsich E, Vetere A, Mozetic P, Campa C, Donati I, Vittur F, Gamini A, Paoletti S. The role of Galectin-1 in the interaction between chondrocytes and a lactose-modified chitosan. Biomaterials. 2005;26:4975–84.
Donati I, Haug IJ, Scarpa T, Borgogna M, Draget KI, Skjåk-Braek G, Paoletti S. Synergistic effects in semidilute mixed solutions of alginate and lactose-modified chitosan (chitlac). Biomacromolecules. 2007;8:957–62.
Choi BK, Kim KY, Yoo YJ, Oh SJ, Choi JH, Kim CY. In vitro antimicrobial activity of a chitooligosaccharide mixture against Actinobacillus actinomycetemcomitans and Streptococcus mutans. Int J Antimicrob Agents. 2001;18:553–7.
Eberhard J, Pietschmann R, Falk W, Jepsen S, Dommisch H. The immune response of oral epithelial cells induced by single-species and complex naturally formed biofilms. Oral Microbiol Immunol. 2009;24:325–30.
Chen JP. Late angiographic stent thrombosis (LAST): the cloud behind the drug-eluting stent silver lining? J Invasive Cardiol. 2007;19:395–400.
Ghosh M, Sinha S, Chakraborty A, Mallick SK, Bandyopadhyay M, Mukherjee A. In vitro and in vivo genotoxicity of silver nanoparticles. Mutat Res. 2012;749:60–9.
Travan A, Pelillo C, Donati I, Marsich E, Benincasa M, Scarpa T, Semeraro S, Turco G, Gennaro R, Paoletti S. Non-cytotoxic silver nanoparticle-polysaccaride nanocomposite with antimicrobial activity. Biomacromolecules. 2009;10:1429–35.
Travan A, Marsich E, Donati I, Benincasa M, Giazzon M, Felisari L, Paoletti S. Silver-polysaccharide nanocomposite antimicrobial coatings for methacrylic thermosets. Acta Biomater. 2011;7:337–46.
Conner SD, Schmid SL. Regulated portals of entry into the cell. Nature. 2003;422:37–44.
Greulich C, Diendorf J, Simon T, Eggeler G, Epple M, Köller M. Uptake and intracellular distribution of silver nanoparticles in human mesenchymal stem cells. Acta Biomater. 2001;7:347–54.
Glick D, Barth S, Macleod KF. Autophagy: cellular and molecular mechanisms. J Pathol. 2010;221:3–12.
Oczypok EA, Oury TD, Chu CT. It’s a cell-eat-cell world: autophagy and phagocytosis. Am J Pathol. 2013;182:612–22.
Tanida I. Autophagosome formation and molecular mechanism of autophagy. Antioxid Redox Signal. 2011;14:2201–14.
Di Giulio M, D’Ercole S, Zara S, Cataldi A, Cellini L. Streptococcus mitis/human gingival fibroblasts co-culture: the best natural association in answer to the 2-hydroxyethyl methacrylate release. APMIS. 2012;120:139–46.
Ionescu AC, Brambilla E, Travan A, Marsich E, Donati I, Gobbi P, Turco G, Di Lenarda R, Cadenaro M, Paoletti S, Breschi L. Silver-polysaccharide antimicrobial nanocomposite coating for methacrylic surfaces reduces Streptococcus mutans biofilm formation in vitro. J Dent. 2015;43:1483–90.
Marsich E, Bellomo F, Turco G, Travan A, Donati I, Paoletti S. Nano-composite scaffolds for bone tissue engineering containing silver nanoparticles: preparation, characterization and biological properties. J Mater Sci Mater Med. 2013;24:1799–807.
Marsich E, Travan A, Donati I, Turco G, Kulkova J, Moritz N, Aro HT, Crosera M, Paoletti S. Biological responses of silver-coated thermosets: an in vitro and in vivo study. Acta Biomater. 2013;9:5088–99.
di Giacomo V, Pacella S, Rapino M, Di Giulio M, Zara S, Pasquantonio G, Cellini L, Cataldi A. pPKC α regulates through integrin β1 human gingival fibroblasts/Streptococcus mitis adhesion in response to HEMA. Int Endod J. 2013;46:1164–72.
Zhang R, Piao MJ, Kim KC, Kim AD, Choi JY, Choi J, Hyun JW. Endoplasmic reticulum stress signaling is involved in silver nanoparticles-induced apoptosis. Int J Biochem Cell Biol. 2012;44:224–32.
Sancilio S, di Giacomo V, Di Giulio M, Gallorini M, Marsich E, Travan A, Tarusha L, Cellini L, Cataldi A. Biological responses of human gingival fibroblasts (HGFs) in an innovative co-culture model with Streptococcus mitis to thermosets coated with a silver polysaccharide antimicrobial system. PLoS One. 2014;9(5):e96520.
Di Giulio M, Di Bartolomeo S, Di Campli E, Sancilio S, Marsich E, Travan A, Cataldi A, Cellini L. The effect of a silver nanoparticle polysaccharide system on streptococcal and saliva-derived biofilms. Int J Mol Sci. 2013;14:13615–25.
Gallorini M, Cataldi A, di Giacomo V. HEMA-induced cytotoxicity: oxidative stress, genotoxicity and apoptosis. Int Endod J. 2014;4:813–8.
Gallorini M, Sancilio S, Zara S, De Colli M, Di Giulio M, Cataldi A, di Giacomo V. Involvement of mitochondrial signalling pathway in HGFs/S. mitis coculture response to TEGDMA treatment. J Biomed Mater Res A. 2014;102:3931–8.
Miethling-Graff R, Rumpker R, Richter M, Verano-Braga T, Kjeldsen F, Brewer J, Hoyland J, Rubahn HG, Erdmann H. Exposure to silver nanoparticles induces size- and dose-dependent oxidative stress and cytotoxicity in human colon carcinoma cells. Toxicol In Vitro. 2014;28:1280–9.
Honda K. Interleukin-6 and soluble interleukin-6 receptor suppress osteoclastic differentiation by inducing PGE(2) production in chondrocytes. Oral Sci. 2011;53:87–96.
Camporeale A, Poli V. IL-6, IL-17 ans STAT3: a holy trinity in auto-immunity? Front Biosci. 2012;17:2306–26.
Pelissier-Rota MA, Pelosi L, Meresse P, Jacquier-Sarlin MR. Nicotine-induced cellular stresses and autophagy in human cancer colon cells: a supportive effect on cell homeostasis via up-regulation of Cox-2 and PGE2 production. Int J Biochem Cell Biol. 2015;65:239–56.
Teti G, Orsini G, Salvatore V, Focaroli S, Mazzotti MC, Ruggeri A, Mattioli-Belmonte M, Falconi M. HEMA but not TEGDMA induces autophagy in human gingival fibroblast. Front Physiol. 2015;6:275.
Chikte S, Panchal N, Warnes G. Use of LysoTracker dyes: a flow cytometric study of autophagy. Cytometry A. 2014;85:169–78.
Klionsky DJ, Cuervo AM, Seglen PO. Methods for monitoring autophagy from yeast to human. Autophagy. 2007;3:181–206.
Sou YS, Tanida I, Komatsu M, Ueno T, Kominami E. Phosphatidylserine is an in vitro target of the mammalian Atg8 modifiers, LC3, GABARAP, and GATE-16. J Biol Chem. 2005;281:3017–24.
Mizushima N, Yoshimorim T, Levine B. Methods in mammalian autophagy research. Cell. 2010;140:313–26.
Ding Y, Kim S, Lee SY, Koo JK, Wang Z, Choi ME. Autophagy regulates TGF-β expression and suppresses kidney fibrosis induced by unilateral ureteral obstruction. J Am Soc Nephrol. 2014;25:2835–46.
Acknowledgments
This work was supported by a two sources: first, a FIRB project, “Accordi di programma 2010”, directed by Prof. Cataldi (Cod.RBAPI095), on “Processi degenerativi dei tessuti mineralizzati del cavo orale, impieghi di biomateriali e controllo delle interazioni con microrganismi dell’ambiente”; and second, an “ex 60 %” grant held by Dr. di Giacomo. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors would like to thank Sheila Beatty for editing the English usage of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Gallorini, M., di Giacomo, V., Di Valerio, V. et al. Cell-protection mechanism through autophagy in HGFs/S. mitis co-culture treated with Chitlac-nAg. J Mater Sci: Mater Med 27, 186 (2016). https://doi.org/10.1007/s10856-016-5803-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5803-5