Abstract
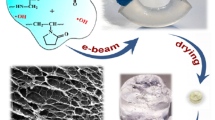
Hydrogels are suitable materials to promote cell proliferation and tissue support because of their hydrophilic nature, porous structure and sticky properties. However, hydrogel synthesis involves the addition of additives that can increase the risk of inducing cytotoxicity. Sterilization is a critical process for hydrogel clinical use as a proper scaffold for tissue engineering. In this study, poly(ethylene glycol) (PEG), poly(ethylene glycol)-chitosan (PEG-CH) and multi-arm PEG hydrogels were synthesized by free radical polymerization and sterilized by gamma irradiation or disinfected using 70 % ethanol. The biocompatibility assessment in human fibroblasts and hemocompatibility studies (hemolysis, platelet aggregation, morphology of mononuclear cells and viability) in peripheral blood from healthy volunteers (ex vivo), were performed. The sterilization or disinfection effect on hydrogel structures was evaluated by FT-IR spectroscopy. Results indicated that hydrogels do not induce any damage to fibroblasts, erythrocytes, platelets or mononuclear cells. Moreover, there was no significant difference in the biocompatibility after the sterilization or disinfection treatment. However, after gamma irradiation, several IR spectroscopic bands were shifted to higher or lower energies with different intensity in all hydrogels. In particular, several bands associated to carboxyl or hydroxyl groups were slightly shifted, possibly associated to scission reactions. The disinfection treatment (70 % ethanol) and γ-irradiation at 13.83 ± 0.7 kGy did not induce morphological damages and yielded sterile and biocompatible PEG hydrogels potentially useful for clinical applications.





Similar content being viewed by others
References
Bhat S, Kumar A. Biomaterials and bioengineering tomorrow’s healthcare. Biomatter. 2013;3:e24717.
Duffy C, Venturato A, Callanan A, Lilienkampf A, Bradley M. Arrays of 3D double-network hydrogels for the high-throughput discovery of materials with enhanced physical and biological properties. Acta Biomater. 2016;34:104–12.
Hoffman AS. Hydrogels for biomedical applications. Adv Drug Deliv Rev. 2012;64:18–23.
Zhang M, Li X, Gong Y, Zhao N, Zhang X. Properties and biocompatibility of chitosan films modified by blending with PEG. Biomaterials. 2002;23:2641–8.
Franco RA, Min Y-K, Yang H-M, Lee B-T. Fabrication and biocompatibility of novel bilayer scaffold for skin tissue engineering applications. J Biomater Appl. 2013;27:605–15.
Aziz MA, Cabral JD, Brooks HJ, McConnell MA, Fitzpatrick C, Hanton LR, et al. In vitro biocompatibility and cellular interactions of a chitosan/dextran‐based hydrogel for postsurgical adhesion prevention. J Biomed Mater Res B Appl Biomater. 2015;103:332–41.
Tohfafarosh M, Baykal D, Kiel JW, Mansmann K, Kurtz SM. Effects of gamma and e-beam sterilization on the chemical, mechanical and tribological properties of a novel hydrogel. J Mech Behav Biomed Mater. 2016;53:250–6.
Zhang X, Xu B, Puperi DS, Yonezawa AL, Wu Y, Tseng H, et al. Integrating valve-inspired design features into poly (ethylene glycol) hydrogel scaffolds for heart valve tissue engineering. Acta Biomater. 2015;14:11–21.
Kar M, Shih Y-RV, Velez DO, Cabrales P, Varghese S. Poly (ethylene glycol) hydrogels with cell cleavable groups for autonomous cell delivery. Biomaterials. 2016;77:186–97.
Zhu J. Bioactive modification of poly (ethylene glycol) hydrogels for tissue engineering. Biomaterials. 2010;31:4639–56.
Hamid ZA, Lim K. Evaluation of UV-crosslinked Poly (ethylene glycol) Diacrylate/Poly (dimethylsiloxane) Dimethacrylate Hydrogel: Properties for Tissue Engineering Application. Procedia Chem.. 2016;19:410–8.
Ruedinger F, Lavrentieva A, Blume C, Pepelanova I, Scheper T. Hydrogels for 3D mammalian cell culture: a starting guide for laboratory practice. Appl Microbiol Biotechnol. 2015;99:623–36.
Zhang X, Yang D, Nie J. Chitosan/polyethylene glycol diacrylate films as potential wound dressing material. Int J Biol Macromol. 2008;43:456–62.
Holy CE, Cheng C, Davies JE, Shoichet MS. Optimizing the sterilization of PLGA scaffolds for use in tissue engineering. Biomaterials. 2000;22:25–31.
de CPdlF, Mexicanos. lEU. Farmacopea de los Estados Unidos Mexicanos. Mexico 2014.
Guo X, Wang W, Wu G, Zhang J, Mao C, Deng Y, et al. Controlled synthesis of hydroxyapatite crystals templated by novel surfactants and their enhanced bioactivity. New J Chem. 2011;35:663–71.
Chieng BW, Ibrahim NA, Yunus WMZW, Hussein MZ. Poly (lactic acid)/poly (ethylene glycol) polymer nanocomposites: effects of graphene nanoplatelets. Polymers. 2013;6:93–104.
Cao Y, Guan Y, Du J, Luo J, Peng Y, Yip C, et al. Hydrogen-bonded polymer network—poly (ethylene glycol) complexes with shape memory effect. J Mater Chem. 2002;12:2957–60.
Mansur HS, Oréfice RL, Mansur AA. Characterization of poly (vinyl alcohol)/poly (ethylene glycol) hydrogels and PVA-derived hybrids by small-angle X-ray scattering and FTIR spectroscopy. Polymer (Guildf). 2004;45:7193–202.
Lee SY, Zhong X, Valtchev P, Dehghani F. Synthesis of a biodegradable polymer in gas expanded solution: effect of the process on cytocompatibility. Green Chem. 2013;15:1280–91.
Jovančić P, Vílchez A, Molina R. Synthesis of thermo‐sensitive hydrogels from free radical copolymerization of NIPAAm with MBA initiated by atmospheric plasma treatment. Plasma Process Polym. 2016. doi:10.1002/ppap.201500194
Yildiz S, Sahiner M, Sahiner N. Ionic liquid hydrogel templates: bulkgel, cryogel, and microgel to be used for metal nanoparticle preparation and catalysis. Eur Polymer J. 2015;70:66–78.
Li R, Liu N, Li B, Wang Y, Wu G, Ma J. Synthesis and properties of temperature-sensitive and chemically crosslinkable poly (ether-urethane) hydrogel. Polymer Chem. 2015;6:3671–84.
He C, Cheng C, Ji H-F, Shi Z-Q, Ma L, Zhou M, et al. Robust, highly elastic and bioactive heparin-mimetic hydrogels. Polymer Chem. 2015;6:7893–901.
Faucitano A, Buttafava A, Montanari L, Cilurzo F, Conti B, Genta I, et al. Radiation-induced free radical reactions in polymer/drug systems for controlled release: an EPR investigation. Rad Phys Chem. 2003;67:61–72.
Mellott MB, Searcy K, Pishko MV. Release of protein from highly cross-linked hydrogels of poly (ethylene glycol) diacrylate fabricated by UV polymerization. Biomaterials. 2001;22:929–41.
Jiang Y, Meng X, Wu Z, Qi X. Modified chitosan thermosensitive hydrogel enables sustained and efficient anti-tumor therapy via intratumoral injection. Carbohydr Polym. 2016;144:245–53.
da Silva Aquino KA. Sterilization by gamma irradiation: INTECH Open Access Publisher; 2012.
Pal K, Banthia A, Majumdar D. Biomedical evaluation of polyvinyl alcohol–gelatin esterified hydrogel for wound dressing. J Mater Sci Mater Med. 2007;18:1889–94.
Ghobril C, Grinstaff M. The chemistry and engineering of polymeric hydrogel adhesives for wound closure: a tutorial. Chem Soc Rev. 2015;44:1820–35.
Dobić SN, Jovašević JS, Vojisavljević MD, Tomić SL. Hemocompatibility and swelling studies of poly (2-hydroxyethyl methacrylate-co-itaconic acid-co-poly (ethylene glycol) dimethacrylate) hydrogels. Hemijska Industrija. 2011;65:675–85.
Kumar A, Jaiswal M. Design and in vitro investigation of nanocomposite hydrogel based in situ spray dressing for chronic wounds and synthesis of silver nanoparticles using green chemistry. J Appl Polym Sci. 2016;133:43260–74. doi:10.1002/app.43260-74.
Balakrishnan B, Kumar D, Yoshida Y, Jayakrishnan A. Chemical modification of poly (vinyl chloride) resin using poly (ethylene glycol) to improve blood compatibility. Biomaterials. 2005;26:3495–502.
Amarnath LP, Srinivas A, Ramamurthi A. In vitro hemocompatibility testing of UV-modified hyaluronan hydrogels. Biomaterials. 2006;27:1416–24.
Jang JY, Lee DY, Park SJ, Byun Y. Immune reactions of lymphocytes and macrophages against PEG-grafted pancreatic islets. Biomaterials. 2004;25:3663–9.
Farace C, Sánchez-Moreno P, Orecchioni M, Manetti R, Sgarrella F, Asara Y, et al. Immune cell impact of three differently coated lipid nanocapsules: pluronic, chitosan and polyethylene glycol. Sci Rep. 2016;6:43260–74. doi:10.1038/srep18423.
Naves AF, Motay M, Mérindol R, Davi CP, Felix O, Catalani LH, et al. Layer-by-Layer assembled growth factor reservoirs for steering the response of 3T3-cells. Colloids Surf B Biointerfaces. 2016;139:79–86.
Pires F, Ferreira Q, Rodrigues CA, Morgado J, Ferreira FC. Neural stem cell differentiation by electrical stimulation using a cross-linked PEDOT substrate: expanding the use of biocompatible conjugated conductive polymers for neural tissue engineering. Biochim Biophys Acta. 2015;1850:1158–68.
Acknowledgments
The authors gratefully acknowledge financial support from UAEM (grant number: 3890/2015FS) and the ININ-AS-503 project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Escudero-Castellanos, A., Ocampo-García, B.E., Domínguez-García, M.V. et al. Hydrogels based on poly(ethylene glycol) as scaffolds for tissue engineering application: biocompatibility assessment and effect of the sterilization process. J Mater Sci: Mater Med 27, 176 (2016). https://doi.org/10.1007/s10856-016-5793-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10856-016-5793-3