Abstract
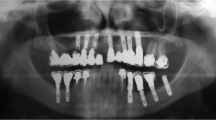
The long term effect of the human body on a pyrolytic carbon covered C/C composite maxillofacial implant (CarBulatTm) was investigated by comparing the structure, the surface morphology and composition of an implant retrieved after 8 years to a sterilized, but not implanted one. Although the thickness of the carbon fibres constituting the implants did not change during the 8 year period, the surface of the implant retrieved was covered with a thin surface layer not present on the unimplanted implant. The composition of this layer is identical to the composition of the underlying carbon fibres. Calcium can only be detected on the surface as a trace element implying that the new layer is not formed by bone tissue. Residual soft tissue penetrating the bulk material between the carbon fibre bunches was found on the retrieved implant indicating the importance of the surface morphology in tissue growth and adhering to implants.







Similar content being viewed by others
References
Scholz M-S, Blanchfield JP, Bloom LD, Coburn BH, Elkington M, Fuller JD, Gilbert ME, Muflahi SA, Pernice MF, Rae SI, Trevarthen JA, White SC, Weaver PM, Bond IP. The use of composite materials in modern orthopaedic medicine and prosthetic devices: a review. Compos Sci Technol. 2011;71:1791–803.
Golecki I. Rapid vapor-phase densification of refractory composites. Mat Sci Eng R. 1997;20:37–124.
Jenkins DHR, Forster IW, McKibbin, Ralis ZA. Induction of tendon ligament formation by carbon implants. J Bone Joint Surg. (Br). 1977;59:53–7.
Adams D, Williams DF. The response of bone to carbon–carbon composites. Biomaterials. 1984;5:59–64.
More N, Baquey C, Barthe X, Rouais F, Rivel J, Trinquecoste M, Marchand A. Biocompatibility of carbon–carbon materials: in vivo study of their erosion using 14carbon labelled samples. Biomaterials. 1988;9:328–34.
Czajkowska B, Blazewicz M. Phagocytosis of chemically modified carbon materials. Biomaterials. 1997;18:69–74.
Pesakova V, Klezl Z, Balik K, Adam M. Biomechanical and biological properties of the implant material carbon–carbon composite covered with pyrolytic carbon. J Mater Sci Mater Med. 2000;11:793–8.
Blazewicz M. Carbon Materials in the treatment of soft and hard tissue injuries. Eur Cell Mater. 2001;2:21–9.
Stary V, Bacakova L, Horník J, Chmelík V. Bio-compatibility of the surface layer of pyrolytic graphite. Thin Solid Films. 2003;433:191–8.
Grabinski C, Hussain S, Lafdi K, Braydich-Stolle L, Schlager J. Effect of particle dimension on biocompatibility of carbon nanomaterials. Carbon. 2007;45:2828–35.
Rajzer I, Menaszek E, Bacakova L, Rom M, Blazewicz M. In vitro and in vivo studies on biocompatibility of carbon fibres. J Mater Sci Mater Med. 2010;21:2611–22.
Kieswetter K, Schwartz Z, Dean DD, Doyan BD. The role of implant surface characteristics in the healing of bone. Crit Rev Oral Biol Med. 1996;7:329–45.
Bordji K, Jouzeau JY, Mainard D, Payan E, Delagoutte JP, Netter P. Evaluation of the effect of three surface treatments on the biocompatibility of 316L stainless steel using human differentiated cells. Biomaterials. 1996;17:491–500.
Puleo DA, Nanci A. Understanding and controlling the bone-implant interface. Biomaterials. 1999;20:2311–21.
Jones FH. Teeth and bones: applications of surface science to dental materials and related biomaterials. Surf Sci Rep. 2001;42:75–205.
Pesakova V, Kubies D, Hulejova H, Himmlova L. The influence of implant surface properties on cell adhesion and proliferation. J Mater Sci Mater Med. 2007;18:465–73.
Stanford CM. Surface modification of biomedical and dental implants and the processes of inflammation, wound healing and bone formation. Int J Mol Sci. 2010;11:354–69.
Bacakova L, Filova E, Parizek M, Ruml T, Svorcik V. Modulation of cell adhesion, proliferation and differentiation on materials designed for body implants. Biotechnol Adv. 2011;29:739–67.
Anil S, Anand PS, Alghamdi H and Jansen JA. Dental implant surface enhancement and osseointegration, implant dentistry—a rapidly evolving practice, Prof. Ilser Turkyilmaz (Ed.), ISBN: 978-953-307-658-4, InTech 2011, Available from: http://www.intechopen.com/books/implant-dentistry-a-rapidly-evolving-practice/dental-implant-surface-enhancement-and-osseointegration.
Bacaková L, Stary V, Kofronova O, Lisa V. Polishing and coating carbon fiber-reinforced carbon composites with a carbon-titanium layer enhances adhesion and growth of osteoblast-like MG63 cells and vascular smooth muscle cells in vitro. J Biomed Mat Res. 2001;54:567–78.
Litzler PY, Benard L, Barbier-Frebourg N, Vilain S, Jouenne T, Beucher E, Bunel C, Lemeland JF, Bessou JP. Biofilm on pyrolytic carbon heart valves: Influence of surface free energy, roughness and bacterial species. J Thorac Cardiov Surg. 2007;134:1025–32.
Ning C, Qiang-xiu W, Jian-wen D, Guang-zheng H, Mu-sen L. Characterization and biological behavior of carbon fiber/carbon composite scaffold with a porous surface for bone tissue reconstruction. New Carbon Mater. 2010;25:232–6.
Lewandowska-Szumiel M, Komender J, Chlopek J. Interaction between carbon composites and bone after itrabone implantation. J Biomed Mater Res. 1999;48:289–96.
Szabo G, Barabas J and Nemeth Z. Long-term comparison of CarBulat™ (pure carbon) and titanium mandibular reconstruction plates. In: Raspal G and Lagunas J G, editors. XVIII Congress of the European Association for Cranio-Maxillo Facial Surgery 2006 Barcelona, Medimond International Proceedings.
Offele D, Harbeck M, Dobberstein RC, von Wurmb-Schwark N, Ritz-Timme S. Soft Tissue removal by maceration and feeding of Dermestes sp.: impact on morphological and biomolecular analyses of dental tissues in forensic medicine. Int J Legal Med. 2007;121:341–8.
Kanaya K, Okayama S. Penetration and energy-loss theory of electrons in solid targets. J Phys D Appl Phys. 1972;5:43–58.
Acknowledgments
The authors would like to thank the help and work of V. K. Josepovits, M. Tóth, K. N. László at the Budapest University of Technology and Economics, E. Felszeghy at the Semmelweis University (Budapest) and Éva Sebők at the University of Copenhagen (Denmark). The authors are especially grateful to Mr. M. Gottesman the director of Ametist Goldy Management LLC (USA) for supplying the implants. This work was supported by the NHDP TÁMOP-4.2.1/B-09/1/KMR-2010-0002 programme.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sebők, B., Kiss, G., Szabó, P.J. et al. SEM and EDS investigation of a pyrolytic carbon covered C/C composite maxillofacial implant retrieved from the human body after 8 years. J Mater Sci: Mater Med 24, 821–828 (2013). https://doi.org/10.1007/s10856-012-4840-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4840-y