Abstract
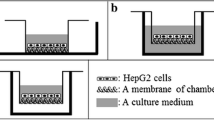
A bioartificial liver bioreactor requires a bifunctional hollow fiber that is hemocompatible on one side and cytocompatible on the other side. In this study, we developed a single-layer skin polyethersulfone (PES) hollow fiber with smooth inner surface and rough/porous outer surface for an artificial liver bioreactor. The hemocompatibility of the inner surface was evaluated by hemolysis, complement activation and clotting time. The cytocompatibility of the outer surface with HepG2 cells was examined by morphology, proliferation and liver-specific functions. The inner surface of the PES hollow fiber exhibited lower hemolysis and complement activation than cellulose acetate (CA) hollow fiber and a prolonged blood coagulation time. HepG2 cells readily adhered to the outer surfaces of the PES hollow fibers, and proliferated to form multicellular aggregates with time. Furthermore, HepG2 cells cultured on the outer surface of the PES hollow fiber exhibited higher proliferation ability and liver-specific functions than those grown on the CA hollow fiber. These results suggest that the single-layer skin PES hollow fiber is a bifunctional hollow fiber with good hemocompatibility on the inner side and cytocompatibility on the outer side. Thus, porous and single-layer skin PES hollow fibers may have potential as materials for an artificial liver bioreactor.







Similar content being viewed by others
References
Liou IW, Larson AM. Role of liver transplantation in acute liver failure. Semin Liver Dis. 2008;28:201–9.
Sgroi A, Serre-Beinier V, Morel P, Buhler L. What clinical alternatives to whole liver transplantation? Current status of artificial devices and hepatocyte transplantation. Transplantation. 2009;87:457–66.
Mizumoto H, Funatsu K. Liver regeneration using a hybrid artificial liver support system. Artif Organs. 2004;28:53–7.
Strain AJ, Neuberger JM. A bioartificial liver—state of the art. Science. 2002;295:1005–9.
Morsiani E, Pazzi P, Puviani AC, Brogli M, Valieri L, Gorini P, Scoletta P, Marangoni E, Ragazzi R, Azzena G, Frazzoli E, Di Luca D, Cassai E, Lombardi G, Cavallari A, Faenza S, Pasetto A, Girardis M, Jovine E, Pinna AD. Early experiences with a porcine hepatocyte-based bioartificial liver in acute hepatic failure patients. Int J Artif Organs. 2002;25:192–202.
Demetriou AA, Brown RS Jr, Busuttil RW, Fair J, McGuire BM, Rosenthal P, Am Esch JS II, Lerut J, Nyberg SL, Salizzoni M, Fagan EA, de Hemptinne B, Broelsch CE, Muraca M, Salmeron JM, Rabkin JM, Metselaar HJ, Pratt D, De La Mata M, McChesney LP, Everson GT, Lavin PT, Stevens AC, Pitkin Z, Solomon BA. Prospective, randomized, multicenter, controlled trial of a bioartificial liver in treating acute liver failure. Ann Surg. 2004;239:660–7; discussion 7–70.
Poyck PP, Pless G, Hoekstra R, Roth S, Van Wijk AC, Schwartlander R, Van Gulik TM, Sauer IM, Chamuleau RA. In vitro comparison of two bioartificial liver support systems: MELS CellModule and AMC-BAL. Int J Artif Organs. 2007;30:183–91.
Kataoka K, Nagao Y, Nukui T, Akiyama I, Tsuru K, Hayakawa S, Osaka A, Huh NH. An organic–inorganic hybrid scaffold for the culture of HepG2 cells in a bioreactor. Biomaterials. 2005;26:2509–16.
Park J, Li Y, Berthiaume F, Toner M, Yarmush ML, Tilles AW. Radial flow hepatocyte bioreactor using stacked microfabricated grooved substrates. Biotechnol Bioeng. 2008;99:455–67.
Lv G, Zhao L, Zhang A, Du W, Chen Y, Yu C, Pan X, Zhang Y, Song T, Xu J, Li L. Bioartificial liver system based on choanoid fluidized bed bioreactor improve the survival time of fulminant hepatic failure pigs. Biotechnol Bioeng. 2011;108:2229–36.
Hoque ME, Mao HQ, Ramakrishna S. Hybrid braided 3-D scaffold for bioartificial liver assist devices. J Biomater Sci Polym Ed. 2007;18:45–58.
van de Kerkhove MP, Di Florio E, Scuderi V, Mancini A, Belli A, Bracco A, Scala D, Scala S, Zeuli L, Di Nicuolo G, Amoroso P, Calise F, Chamuleau RA. Bridging a patient with acute liver failure to liver transplantation by the AMC-bioartificial liver. Cell Transplant. 2003;12:563–8.
Chen G, Palmer AF. Hemoglobin regulates the metabolic, synthetic, detoxification, and biotransformation functions of hepatoma cells cultured in a hollow fiber bioreactor. Tissue Eng Part A. 2010;16:3231–40.
Park JK, Lee DH. Bioartificial liver systems: current status and future perspective. J Biosci Bioeng. 2005;99:311–9.
Mazariegos GV, Patzer JF II, Lopez RC, Giraldo M, Devera ME, Grogan TA, Zhu Y, Fulmer ML, Amiot BP, Kramer DJ. First clinical use of a novel bioartificial liver support system (BLSS). Am J Transplant. 2002;2:260–6.
Ho Ye S, Watanabe J, Takai M, Iwasaki Y, Ishihara K. High functional hollow fiber membrane modified with phospholipid polymers for a liver assist bioreactor. Biomaterials. 2006;27:1955–62.
De Bartolo L, Salerno S, Curcio E, Piscioneri A, Rende M, Morelli S, Tasselli F, Bader A, Drioli E. Human hepatocyte functions in a crossed hollow fiber membrane bioreactor. Biomaterials. 2009;30:2531–43.
Ran F, Nie S, Zhao W, Li J, Su B, Sun S, Zhao C. Biocompatibility of modified polyethersulfone membranes by blending an amphiphilic triblock co-polymer of poly(vinyl pyrrolidone)-β-poly(methyl methacrylate)-β-poly(vinyl pyrrolidone). Acta Biomater. 2011;7:3370–81.
Lu HF, Lim WS, Zhang PC, Chia SM, Yu H, Mao HQ, Leong KW. Galactosylated poly(vinylidene difluoride) hollow fiber bioreactor for hepatocyte culture. Tissue Eng. 2005;11:1667–77.
Eash HJ, Jones HM, Hattler BG, Federspiel WJ. Evaluation of plasma resistant hollow fiber membranes for artificial lungs. ASAIO J. 2004;50:491–7.
Zhang SC, Liu T, Wang YJ. Porous and single-skinned polyethersulfone membranes support the growth of HepG2 cells: a potential biomaterial for bioartificial liver systems. J Biomater Appl. 2011. doi:10.1177/0885328211406299.
Dahe GJ, Teotia RS, Kadam SS, Bellare JR. The biocompatibility and separation performance of antioxidative polysulfone/vitamin E TPGS composite hollow fiber membranes. Biomaterials. 2011;32:352–65.
Unger RE, Wolf M, Peters K, Motta A, Migliaresi C, James Kirkpatrick C. Growth of human cells on a non-woven silk fibroin net: a potential for use in tissue engineering. Biomaterials. 2004;25:1069–75.
Lee KD, Kuo TK, Whang-Peng J, Chung YF, Lin CT, Chou SH, Chen JR, Chen YP, Lee OK. In vitro hepatic differentiation of human mesenchymal stem cells. Hepatology. 2004;40:1275–84.
Kinasiewicz A, Smietanka A, Dudzinski K, Chwojnowski A, Gajkowska B, Werynski A. Spongy polyethersulfone membrane for hepatocyte cultivation: studies on human hepatoma C3A cells. Artif Organs. 2008;32:747–52.
De Bartolo L, Morelli S, Rende M, Salerno S, Giorno L, Lopez LC, Favia P, d’Agostino R, Drioli E. Galactose derivative immobilized glow discharge processed polyethersulfone membranes maintain the liver cell metabolic activity. J Nanosci Nanotechnol. 2006;6:2344–53.
De Bartolo L, Morelli S, Lopez LC, Giorno L, Campana C, Salerno S, Rende M, Favia P, Detomaso L, Gristina R, d’Agostino R, Drioli E. Biotransformation and liver-specific functions of human hepatocytes in culture on RGD-immobilized plasma-processed membranes. Biomaterials. 2005;26:4432–41.
Patzer JF 2nd. Advances in bioartificial liver assist devices. Ann N Y Acad Sci. 2001;944:320–33.
Miyauchi T, Yamada M, Yamamoto A, Iwasa F, Suzawa T, Kamijo R, Baba K, Ogawa T. The enhanced characteristics of osteoblast adhesion to photofunctionalized nanoscale TiO2 layers on biomaterials surfaces. Biomaterials. 2010;31:3827–39.
Bettahalli NM, Vicente J, Moroni L, Higuera GA, van Blitterswijk CA, Wessling M, Stamatialis DF. Integration of hollow fiber membranes improves nutrient supply in three-dimensional tissue constructs. Acta Biomater. 2011;7:3312–24.
Tsunoda N, Kokubo K, Sakai K, Fukuda M, Miyazaki M, Hiyoshi T. Surface roughness of cellulose hollow fiber dialysis membranes and platelet adhesion. ASAIO J. 1999;45:418–23.
Su BH, Fu P, Li Q, Tao Y, Li Z, Zao HS, Zhao CS. Evaluation of polyethersulfone highflux hemodialysis membrane in vitro and in vivo. J Mater Sci Mater Med. 2008;19:745–51.
Krieter DH, Lemke HD. Polyethersulfone as a high-performance membrane. Contrib Nephrol. 2011;173:130–6.
Liu Z, Deng X, Wang M, Chen J, Zhang A, Gu Z, Zhao C. BSA-modified polyethersulfone membrane: preparation, characterization and biocompatibility. J Biomater Sci Polym Ed. 2009;20:377–97.
Sperling C, Houska M, Brynda E, Streller U, Werner C. In vitro hemocompatibility of albumin-heparin multilayer coatings on polyethersulfone prepared by the layer-by-layer technique. J Biomed Mater Res A. 2006;76:681–9.
De Bartolo L, Catapano G, Della Volpe C, Drioli E. The effect of surface roughness of microporous membranes on the kinetics of oxygen consumption and ammonia elimination by adherent hepatocytes. J Biomater Sci Polym Ed. 1999;10:641–55.
Unger RE, Peters K, Huang Q, Funk A, Paul D, Kirkpatrick CJ. Vascularization and gene regulation of human endothelial cells growing on porous polyethersulfone (PES) hollow fiber membranes. Biomaterials. 2005;26:3461–9.
Lin YC, Brayfield CA, Gerlach JC, Rubin JP, Marra KG. Peptide modification of polyethersulfone surfaces to improve adipose-derived stem cell adhesion. Acta Biomater. 2009;5:1416–24.
Acknowledgments
This research was supported by grants from the National Natural Science Foundation of China (Grant No. 30800237, 31076328 and 30470458). We gratefully acknowledge Deyuan Science & Technology Development Co., Ltd. for preparing the hollow fibers. We thank all members of our laboratory for sharing reagents and advice. We thank American Journal Experts for editorial assistance.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, S., Liu, T., Chen, L. et al. Bifunctional polyethersulfone hollow fiber with a porous, single-layer skin for use as a bioartificial liver bioreactor. J Mater Sci: Mater Med 23, 2001–2011 (2012). https://doi.org/10.1007/s10856-012-4673-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-012-4673-8