Abstract
Background
The impact of psychosocial risk factors (PSRFs) on outcomes in patients undergoing percutaneous left atrial appendage occlusion (LAAO) device implantation is unclear. We aimed to analyze the association of psychosocial risk factors with outcomes in patients undergoing LAAO.
Methods
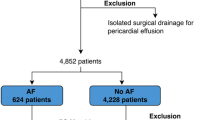
Data were extracted from the Nationwide readmissions database for the calendar years 2016-2019. LAAO device implantations were identified using ICD-10-CM code 02L73DK. The outcomes of interest included procedural complications, inpatient mortality, resource utilization, and 30-day readmissions. Patients were divided into two cohorts based on the absence or presence of PSRFs.
Results
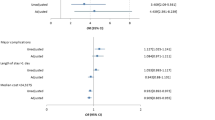
Our cohort included a total of 54,900 patients, of which, 19,984 (36.4%) had ≥ 1 PSRF as compared to 34,916 (63.6%) with no PSRFs. The prevalence of major complications (3.3% vs 2.8%, p=0.03) was significantly higher in patients with ≥ 1 PSRF as compared to no PSRFs. Furthermore, patients with ≥ 1 PSRF had a significantly higher 30-day readmission rate (6.9% vs 6.2%, p=0.02). In the multivariable model, the presence of ≥ 1 PSRF was associated with significantly higher odds of overall complications [adjusted odds ratio (aOR):1.11; 95% confidence interval (CI): 1.01-1.21; p=0.02]. Additionally, the presence of ≥ 1 PSRF was associated with higher odds of prolonged hospital stay for more than one day (aOR: 1.30; 95% CI: 1.21-1.40; p<0.01).
Conclusion
The high prevalence of PSRFs may be associated with poorer outcomes in patients with AF patients undergoing LAAO device implantations. These data merit further study to help in the selection process of patients for LAAO for improved outcomes.


Similar content being viewed by others
References
Go AS, Mozaffarian D, Roger VL, et al. Executive summary: heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):399–410. https://doi.org/10.1161/01.cir.0000442015.53336.12.
Saposnik G, Gladstone D, Raptis R, Zhou L, Hart RG. Investigators of the Registry of the Canadian Stroke Network (RCSN) and the Stroke Outcomes Research Canada (SORCan) Working Group. Atrial fibrillation in ischemic stroke: predicting response to thrombolysis and clinical outcomes. Stroke. 2013;44(1):99–104. https://doi.org/10.1161/STROKEAHA.112.676551.
Ruff CT, Giugliano RP, Braunwald E, et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: a meta-analysis of randomised trials. Lancet. 2014;383(9921):955–62. https://doi.org/10.1016/S0140-6736(13)62343-0.
Marzec LN, Wang J, Shah ND, et al. Influence of direct oral anticoagulants on rates of oral anticoagulation for atrial fibrillation. J Am Coll Cardiol. 2017;69(20):2475–84. https://doi.org/10.1016/j.jacc.2017.03.540.
Schauer DP, Moomaw CJ, Wess M, Webb T, Eckman MH. Psychosocial risk factors for adverse outcomes in patients with nonvalvular atrial fibrillation receiving warfarin. J Gen Intern Med. 2005;20(12):1114–9. https://doi.org/10.1111/j.1525-1497.2005.0242.x.
Ravvaz K, Weissert JA, Jahangir A, Ruff CT. Evaluating the effects of socioeconomic status on stroke and bleeding risk scores and clinical events in patients on oral anticoagulant for new onset atrial fibrillation. PloS One. 2021;16(3):e0248134. https://doi.org/10.1371/journal.pone.0248134.
Reddy VY, Sievert H, Halperin J, Doshi SK, Buchbinder M, Neuzil P, et al. Percutaneous left atrial appendage closure vs warfarin for atrial fibrillation: a randomized clinical trial [published correction appears in JAMA. 2015 Mar 10;313(10):1061]. JAMA. 2014;312(19):1988–98. https://doi.org/10.1001/jama.2014.15192.
"Healthcare Cost and Utilization Project. Overview of the Nationwide Readmissions Database (NRD)". https://www.hcup-us.ahrq.gov/nrdoverview.jsp. Accessed January 23, 2023.
Khan MZ, Munir MB, Darden D, Pasupula DK, Balla S, Han FT, et al. Racial disparities in in-hospital adverse events among patients with atrial fibrillation implanted with a Watchman left atrial appendage occlusion device: a US national perspective. Circ Arrhythm Electrophysiol. 2021;14(5):e009691. https://doi.org/10.1161/CIRCEP.120.009691.
Munir MB, Khan MZ, Darden D, Pasupula DK, Balla S, Han FT, et al. Pericardial effusion requiring intervention in patients undergoing percutaneous left atrial appendage occlusion: Prevalence, predictors, and associated in-hospital adverse events from 17,700 procedures in the United States. Heart Rhythm. 2021;18(9):1508–15. https://doi.org/10.1016/j.hrthm.2021.05.017.
Newell P, Zogg C, Shirley H, et al. The effect of psychosocial risk factors on outcomes after aortic valve replacement. JACC Cardiovasc Interv. 2022;15(22):2326–35.
DeFilippis EM, Breathett K, Donald EM, et al. Psychosocial risk and its association with outcomes in continuous-flow left ventricular assist device patients. Circ Heart Fail. 2020;13(9):e006910. https://doi.org/10.1016/j.jcin.2022.08.014.
Nielsen S, Giang KW, Wallinder A, et al. Social factors, sex, and mortality risk after coronary artery bypass grafting: a Population‐Based cohort study. J Am Heart Assoc. 2019;8(6):e011490. https://doi.org/10.1161/JAHA.118.011490.
Stirbu I, Looman C, Nijhof GJ, Reulings PG, Mackenbach JP. Income inequalities in case death of ischaemic heart disease in the Netherlands: a national record-linked study. J Epidemiol Community Health. 2012;66(12):1159–66. https://doi.org/10.1136/jech-2011-200924.
Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132(9):873–98. https://doi.org/10.1161/CIR.0000000000000228.
Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802–13. https://doi.org/10.1097/01.psy.0000146332.53619.b2.
van Reedt Dortland AK, Giltay EJ, van Veen T, Zitman FG, Penninx BW. Longitudinal relationship of depressive and anxiety symptoms with dyslipidemia and abdominal obesity. Psychosom Med. 2013;75(1):83–9. https://doi.org/10.1097/PSY.0b013e318274d30f.
Thomas AJ, Kalaria RN, O'Brien JT. Depression and vascular disease: what is the relationship? J Affect Disord. 2004;79(1-3):81–95. https://doi.org/10.1016/S0165-0327(02)00349-X.
Darden D, Duong T, Du C, et al. Sex Differences in Procedural Outcomes Among Patients Undergoing Left Atrial Appendage Occlusion: Insights From the NCDR LAAO Registry [published correction appears in JAMA Cardiol. 2021 Oct 20;]. JAMA Cardiol. 2021;6(11):1275–84. https://doi.org/10.1001/jamacardio.2021.3021.
Bjørnnes AK, Parry M, Lie I, Falk R, Leegaard M, Rustøen T. The association between hope, marital status, depression and persistent pain in men and women following cardiac surgery. BMC Womens Health. 2018;18(1):2. https://doi.org/10.1186/s12905-017-0501-0.
Bunker SJ, Colquhoun DM, Esler MD, et al. "Stress" and coronary heart disease: psychosocial risk factors. Med J Aust. 2003;178(6):272–6. https://doi.org/10.5694/j.1326-5377.2003.tb05193.x.
Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sørensen HT. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol. 2011;11:83.
Henderson T, Shepheard J, Sundararajan V. Quality of diagnosis and procedure coding in ICD-10 administrative data. Med Care. 2006;44(11):1011–9.
Alhajji M, Kawsara A, Alkhouli M. Validation of acute ischemic stroke codes using the international classification of diseases tenth revision. Am J Cardiol. 2020;125(7):1135.
Hirji S, Zogg CK, Kaneko T. The utility of the nationwide readmissions database in understanding contemporary transcatheter aortic valve replacement outcomes. Eur Heart J. 2020;41(45):4358–9. https://doi.org/10.1093/eurheartj/ehaa581.
Eshelman AK, Mason S, Nemeh H, Williams C. LVAD destination therapy: applying what we know about psychiatric evaluation and management from cardiac failure and transplant. Heart Fail Rev. 2009;14(1):21–8. https://doi.org/10.1007/s10741-007-9075-5.
Acknowledgments
None
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
Due to the de-identified nature of the NRD dataset, the need for informed consent and Institutional Review Board approval is waived.
Conflicts of Interest
None of the authors have conflicts of interest related to this manuscript.
Informed Consent
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Agarwal, S., Munir, M.B., Khan, M.Z. et al. Impact of Psychosocial Risk Factors on Outcomes of Atrial Fibrillation Patients undergoing Left Atrial Appendage Occlusion Device Implantation. J Interv Card Electrophysiol 66, 2031–2040 (2023). https://doi.org/10.1007/s10840-023-01546-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-023-01546-4