Abstract
Background
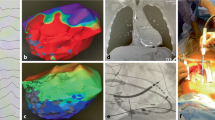
Ventricular tachycardia (VT) ablation of mid- or epicardial substrate is difficult and requires a creative approach in patients with a history of coronary bypass that precludes percutaneous epicardial catheter manipulation. The coronary venous system (CVS) provides limited access to the epicardial surface of the heart. The objective of this study is to assess the feasibility, safety, and efficacy of epicardial mapping and ablation of VT substrates from the CVS in patients with history of coronary bypass.
Methods
Patients undergoing VT ablation at our institution were retrospectively reviewed. Those who had basal to mid ventricular substrate based on computed tomography imaging and history of coronary bypass were included. Endocardial and CVS mapping and ablation was performed in standard fashion using 3D electroanatomic mapping. The primary endpoint was defined as VT circuit elimination, termination, non-inducibility, or perturbation of the circuit.
Results
Of 192 consecutive VT ablations from 2017 to 2020, 35 (18%) had a history of coronary bypass and basal to the mid-ventricular substrate by imaging. There were no significant characteristic differences between the endocardial only (n = 19) vs endocardial + CVS (n = 16) groups. In 14 (88%) of patients undergoing CVS mapping, the VT circuit was identified to be within access from the epicardial surface. Ablation was attempted in 8 (57%) of these patients, and the primary endpoint was reached in 88% of those undergoing CVS ablation. There were no complications related to CVS ablation.
Conclusion
Mapping and ablation of mid- or epicardial VT circuits from the CVS branches are feasible and safe and may be helpful in the treatment of VT in patients who are otherwise not candidates for percutaneous epicardial ablation.





Similar content being viewed by others
References
Guandalini GS, Liang JJ, Marchlinski FE. Ventricular tachycardia ablation: past, present, and future perspectives. JACC Clin Electrophysiol. 2019;5:1363–83. https://doi.org/10.1016/j.jacep.2019.09.015.
Patel D, Hasselblad V, Jackson KP, Pokorney SD, Daubert JP, Al-Khatib SM. Catheter ablation for ventricular tachycardia in patients with ischemic heart disease: a systematic review and a meta-analysis of randomized controlled trials. J Interv Card Electrophysiol. 2016;45:111–7. https://doi.org/10.1007/s10840-015-0083-4.
Aguilar M, Tedrow UB, Tzou WS, et al. Catheter ablation of ventricular tachycardia in patients with prior cardiac surgery: an analysis from the international VT ablation center collaborative group. J Cardiovasc Electrophysiol. 2021;32:409–16. https://doi.org/10.1111/jce.14849.
Liuba I, Frankel DS, Riley MP, Hutchinson MD, Lin D, Garcia FC, Callans DJ, Supple GE, Dixit S, Bala R, Square F, Zado ES, Marchlinski FE. Scar progression in patients with nonischemic cardiomyopathy and ventricular arrhythmias. Heart Rhythm. 2014;11:755–62. https://doi.org/10.1016/j.hrthm.2014.02.012.
Kumareswaran R, Marchlinski FE. Practical guide to ablation for epicardial ventricular tachycardia when to get access how to deal with anticoagulation and how to prevent complications. Arrhythm Electrophysiol Rev. 2018;7:159–64. https://doi.org/10.15420/aer.2018.10.2.
Aryana A, Tung R, d’Avila A. Percutaneous epicardial approach to catheter ablation of cardiac arrhythmias. JACC Clin Electrophysiol. 2020;6:1–20. https://doi.org/10.1016/j.jacep.2019.10.016.
Bhaskaran A, Tung R, Stevenson WG, Kumar S. Catheter ablation of VT in non-ischaemic cardiomyopathies: endocardial, epicardial and intramural approaches. Heart Lung Circ. 2019;28:84–101. https://doi.org/10.1016/j.hlc.2018.10.007.
Liang JJ, Bogun F. Coronary venous mapping and catheter ablation for ventricular arrhythmias. Methodist Debakey Cardiovasc J. 2021;17:13–8. https://doi.org/10.14797/HUZR1007.
Killu AM, Ebrille E, Asirvatham SJ, et al. Percutaneous epicardial access for mapping and ablation is feasible in patients with prior cardiac surgery, including coronary bypass surgery. Circ Arrhythm Electrophysiol. 2015;8:94–101. https://doi.org/10.1161/CIRCEP.114.002349.
Tschabrunn CM, Haqqani HM, Cooper JM, et al. Percutaneous epicardial ventricular tachycardia ablation after noncoronary cardiac surgery or pericarditis. Heart Rhythm. 2013;10:165–9. https://doi.org/10.1016/j.hrthm.2012.10.012.
Briceno DF, Enriquez A, Liang JJ, et al. Septal coronary venous mapping to guide substrate characterization and ablation of intramural septal ventricular arrhythmia. JACC Clin Electrophysiol. 2019;5:789–800. https://doi.org/10.1016/j.jacep.2019.04.011.
Ghannam M, Siontis KC, Cochet H, Jais P, Eng MJ, Latchamsetty R. Value of mapping and ablation of ventricular tachycardia targets within the coronary venous system in patients with nonischemic cardiomyopathy. Heart Rhythm. 2020;17:520–6. https://doi.org/10.1016/j.hrthm.2020.01.010.
Ohta Y, Kitao S, Yunaga H, Fujii S, Mukai N, Yamamoto K, Ogawa T. Myocardial delayed enhancement CT for the evaluation of heart failure: comparison to MRI. Radiology. 2018;288:682–91. https://doi.org/10.1148/radiol.2018172523.
Yamashita S, Sacher F, Mahida S, Berte B, Lim HS, Komatsu Y, Amraoui S, Denis A, Derval N, Laurent F, Sermesant M, Montaudon M, Hocini M, Haissaguerre M, Jair P, Cochet H. Imaging integration to guide catheter ablation in scar-related ventricular tachycardia. J Cardiovasc Electrophysiol. 2016;27:699–708. https://doi.org/10.1111/jce.12963.
Esposito A, Palmisano A, Antunes S, et al. Cardiac CT with delayed enhancement in the characterization of ventricular tachycardia structural substrate: relationship between CT-segmented scar and electro-anatomic mapping. JACC Cardiovasc Imaging. 2016;9:822–32. https://doi.org/10.1016/j.jcmg.2015.10.024.
Palmisano A, Vignale D, Benedetti G, et al. Late iodine enhancement cardiac computed tomography for detection of myocardial scars: impact of experience in the clinical practice. Radiol Med. 2020;125:128–36. https://doi.org/10.1007/s11547-019-01108-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by our institutional review board and informed consent was obtained prior to treatment. The corresponding author is a member of the Editorial Board.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Karimianpour, A., Badertscher, P., Payne, J. et al. Epicardial mapping and ablation of ventricular tachycardia from the coronary venous system in post-coronary bypass patients. J Interv Card Electrophysiol 66, 145–151 (2023). https://doi.org/10.1007/s10840-022-01250-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01250-9