Abstract
Background
A very high-power short-duration (vHPSD) strategy of radiofrequency (RF) ablation aims to minimize conductive heating and increase resistive heating. We evaluated the feasibility, efficacy and safety of the vHPSD ablation of the cavotricuspid isthmus (CTI) in patients presenting with typical atrial flutter (AFL).
Methods
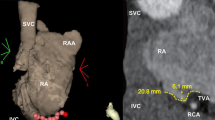
This prospective non-randomized study enrolled 28 consecutive patients (FAST Group) with typical AFL undergoing CTI ablation. The vHPSD ablation was performed applying 90 W, for 4 s, with an irrigation of 8 ml/min. Thirty consecutive patients who, previously, underwent CTI ablation by means of a contact force surrounding flow catheter guided by ablation index (500) served as control group (AI Group).
Results
In the FAST Group, the mean CTI length was 29 ± 6 mm, and the mean number of RF tags was 20 ± 9. The CTI bidirectional “first pass” block was reached in 25 (89%) patients. There were no major procedural complications. After a mean follow-up of 6 ± 2 months, one (3.5%) patient had arrhythmia recurrence. The vHPSD ablation was as effective as AI-guided ablation in achieving acute CTI block (rate of first pass 89% vs 93%, p = 0.59), with a shorter RF time (88 ± 40 s vs 492 ± 269 s, p < 0.001) and similar procedure (30 ± 4 min vs 34 ± 10 min, p = 0.5) and fluoroscopy time (103 ± 29 vs 108 ± 52 s, p = 0.7). At 8 months, the freedom from AFL recurrence was 96% in the FAST group and 97% in the AI group.
Conclusions
Our preliminary data show that the vHPSD ablation represents an effective and safe ablation strategy to achieve bidirectional block for the treatment of typical AFL.


Similar content being viewed by others
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Habibi M, Berger RD, Calkins H. Radiofrequency ablation: technological trends, challenges, and opportunities. Europace. 2021;23:511–9.
Stabile G, Schillaci V, Strisciuglio T, Arestia A, Agresta A, Shopova G, De Simone A, Solimene F. In vivo biophysical characterization of very high power, short duration, temperature-controlled lesions. Pacing Clin Electrophysiol. 2021;44:1717–23.
Leshem E, Zilberman I, Tschabrunn CM, Barkagan M, Contreras-Valdes FM, Govari A, Anter E. High-power and short-duration ablation for pulmonary vein isolation: biophysical characterization. JACC Clin Electrophysiol. 2018;4:467–79.
Barkagan M, Contreras-Valdes FM, Leshem E, Buxton AE, Nakaagawa H, Anter E. High-power and short-duration ablation for pulmonary vein isolation: safety, efficacy, and long-term durability. J Cardiovasc Electrophysiol. 2018;29:1287–96.
Reddy VY, Grimaldi M, De Potter T, Vijgen MJ, Bulava A, Duytschaever MF, Martinek M, Natale A. Pulmonary vein isolation with very high power, short duration, temperature-controlled lesions: the QDOT-FAST Trial. JACC Clin Electrophysiol. 2019;5:778–86.
Richard Tilz R, Sano M, Vogler J, Fink T, Saraei R, Sciacca V, Kirstein B, Phan HL, Hatahet S, Delgado Lopez L, Traub A, Eitel C, Schlüter M, Kuck KH, Heeger CH. Very high-power short-duration temperature-controlled ablation versus conventional power-controlled ablation for pulmonary vein isolation: the fast and furious - AF study. Int J Cardiol Heart Vasc. 2021;35:100847.
Saoudi N, Cosio F, Waldo A, Chen SA, Iesaka Y, Lesh M, Saksena S, Salerno J, Schoels W. Classification of atrial flutter and regular atrial tachycardia according to electrophysiologic mechanism and anatomic bases: a statement from a joint expert group from the Working Group of Arrhythmias of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. J Cardiovasc Electrophysiol. 2001;12:852–66.
Viola G, Stabile G, Bandino S, Rossi L, Marrazzo N, Pecora D, Bottoni N, Solimene F, Schillaci V, Scaglione M, Ocello S, Baiocchi C, Santoro A, Donzelli S, De Ruvo E, Lavalle C, Sanchez-Gomez JM, Pastor JFA, Grandio PC, Ferraris F, Castro A, Rebellato L, Marchese P, Adao L, Primo J, Barra S, Casu G. Safety, efficacy, and reproducibility of cavotricuspid isthmus ablation guided by the ablation index: acute results of the FLAI study. Europace. 2021;23:264–70.
Harvey M, Kim YN, Sousa J, el-Atassi R, Morady F, Calkins H, Langberg JJ. Impedance monitoring during radiofrequency catheter ablation in humans. Pacing Clin Electrophysiol. 1992;15:22–7.
De Bortoli A, Sun LZ, Solheim E, Hoff PI, Schuster P, Ohm OJ, Chen J. Ablation effect indicated by impedance fall is correlated with contact force level during ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24:1210–5.
Haines DE. The biophysics of radiofrequency catheter ablation in the heart: the importance of temperature monitoring. Pacing Clin Electrophysiol. 1993;16:586–91.
Kwon HJ, Lee SS, Park YJ, Park SJ, Park KM, Kim JS, On YK. Effectiveness and safety of high-power and short-duration ablation for cavotricuspid isthmus ablation in atrial flutter. Pacing Clin Electrophysiol. 2020;43:941–6.
Yavin HD, Leshem E, Shapira-Daniels A, Sroubek J, Barkagan M, Haffajee CI, Cooper JM, Anter E. Impact of high-power short-duration radiofrequency ablation on long-term lesion durability for atrial fibrillation ablation. JACC Clin Electrophysiol. 2020;6:973–85.
Golian M, Ramirez FD, Alqarawi W, Hansom SP, Nery PB, Redpath CJ, Nair GM, Shaw GC, Davis DR, Birnie DH, Sadek MM. High-power short-duration radiofrequency ablation of typical atrial flutter. Heart Rhythm. 2020;O2(1):317–23.
Kottmaier M, Deisenhofer I. Is ablation using high power short duration always suitable? Heart Rhythm O2. 2020;1(5):324–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study protocol was approved by the Institutional Ethics Committee.
Consent to participate
Each patient provided informed consent to participate in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schillaci, V., Strisciuglio, T., Stabile, G. et al. Cavotricuspid isthmus ablation by means of very high power, short-duration, temperature-controlled lesions. J Interv Card Electrophysiol 65, 97–102 (2022). https://doi.org/10.1007/s10840-022-01197-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01197-x