Abstract
Purpose
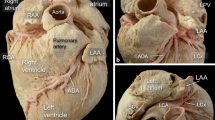
The left ventricular summit (LVS) is a source of difficult-to-treat arrhythmias because of anatomical limitations. The aim of this study was to perform detailed research of the left atrial appendage (LAA) anatomy of cadaveric hearts to analyze their complex anatomy and coverage of the LVS.
Methods and results
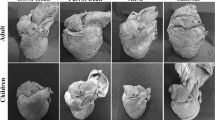
Eighty human formalin fixed hearts (mean age 44.4 ± 15.5, 27.5% females) were investigated. Each LAA size, type, and its relationship to the LVS were analyzed, as well as possible access sites for mapping/ablating electrode. Four types of LAA were observed over two LVS sites that are either accessible or not. The highest coverage over an inaccessible LVS area was observed in the Broccoli type, followed by the Windsock then the Chicken Wing and finally the Cactus types; over the accessible area of the LVS was observed in the Windsock, then in the Chicken Wing, then in the Cactus, and finally in the Broccoli types. The attainable coverage for electrode access is diminished from 25 to 65% because of the complex pectinate muscles and sharp angles. The highest density of the LAA floor made by pectinate muscles can be found in the Broccoli type (p < 0.005), while the Chicken Wing had the highest number of paper-thin-like pouches.
Conclusions
The LAA appears to be a promising entry for ablation-qualified patients with the LV summit originate arrhythmias. The complex internal structure of the LAA may complicate ablation procedures. More prominent appendages are promising in more extensive mapping areas over the LVS.




Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- BSA:
-
Body surface area
- Cx:
-
Circumflex branch
- Dg:
-
Diagonal branch
- EAT:
-
Epicardial adipose tissue
- GCV:
-
Great cardiac vein
- LA:
-
Left atrium
- LAA:
-
Left atrial appendage
- LAD:
-
Left anterior descending artery
- LCA:
-
Left coronary artery
- LV:
-
Left ventricle
- LVS:
-
Left ventricular summit
- OM:
-
Obtuse marginal branch
- PT:
-
Pulmonary trunk
- RFCA:
-
Radiofrequency catheter ablation
- SP:
-
Septal perforator
- VA:
-
Ventricular arrhythmia
References
Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999;82(5):547–54. https://doi.org/10.1136/hrt.82.5.547.PMID:10525506;PMCID:PMC1760793.
Regazzoli D, Ancona F, Trevisi N, Guarracini F, Radinovic A, Oppizzi M, Agricola E, Marzi A, Sora NC, Della Bella P, Mazzone P. Left atrial appendage: physiology, pathology, and role as a therapeutic target. Biomed Res Int. 2015;2015:205013. doi: https://doi.org/10.1155/2015/205013. Epub 2015 Jul 7. PMID: 26236716; PMCID: PMC4508372.
Hołda MK, Koziej M, Wszołek K, Pawlik W, Krawczyk-Ożóg A, Sorysz D, Łoboda P, Kuźma K, Kuniewicz M, Lelakowski J, Dudek D, Klimek-Piotrowska W. Left atrial accessory appendages, diverticula, and left-sided septal pouch in multi-slice computed tomography. Association with atrial fibrillation and cerebrovascular accidents. Kardiologia Polska 2018; 76, 3: 510–519; DOI: https://doi.org/10.5603/KP.a2018.0001
Saygi S. Atrial fibrillation and the role of LAA in pathophysiology and clinical outcomes? J Atr Fibrillation. 2012;5(3):480. https://doi.org/10.4022/jafib.480.PMID:28496767;PMCID:PMC5153207.
Kuniewicz M, Baszko A, Ali D, Karkowski G, Loukas M, Walocha JA, Hołda MK. Left ventricular summit-concept, anatomical structure and clinical significance. Diagnostics (Basel). 2021;11(8):1423. https://doi.org/10.3390/diagnostics11081423.PMID:34441357;PMCID:PMC8393416.
Yamada T, Doppalapudi H, Murakami Y, Yoshida Y, Yoshida N, Okada T, Tsuboi N, Inden Y, Murohara T, Epstein AE, Plumb VJ, Singh SP, Neal Kay G. Idiopathic ventricular arrhythmias originating from the aortic root prevalence, electrocardiographic and electrophysiologic characteristics, and results of radiofrequency catheter ablation. 2008; 52(2) 139–147. J. Am. Coll. Cardiol. https://doi.org/10.1016/j.jacc.2008.03.040
Chung FP, Lin CY, Shirai Y, Futyma P, Santangeli P, Lin YJ, Chang SL, Lo LW, Hu YF, Chang HY, Marchlinski FE, Chen SA. Outcomes of catheter ablation of ventricular arrhythmia originating from the left ventricular summit: a multicenter study. Heart Rhythm. 2020;17(7):1077–83. https://doi.org/10.1016/j.hrthm.2020.02.027 (Epub 2020 Feb 28 PMID: 32113894).
Kuniewicz M, Krupiński M, Gosnell M, Budnicka K, Jakob N, Karkowski G, Urbańczyk-Zawadzka M, Lelakowski J, Walocha J. Applicability of computed tomography preoperative assessment of the LAA in LV summit ablations. J Interv Card Electrophysiol. 2021 Aug;61(2):357–363. doi: https://doi.org/10.1007/s10840-020-00817-8. Epub 2020 Jul 14. PMID: 32666410; PMCID: PMC8324620.
Sosa E, Scanavacca M, d’Avila A. Catheter ablation of the left ventricular outflow tract tachycardia from the left atrium. J Interv Card Electrophysiol. 2002;7:61–5.
Benhayon D, Cogan J, Young M. Left atrial appendage as a vantage point for mapping and ablating premature ventricular contractions originating in the epicardial left ventricular summit. 2018; 6(6):1124-1127; https://doi.org/10.1002/ccr3.1525
Yakubov A, Salayev O, Hamrayev R, Sultankhonov S. A case of successful ablation of ventricular tachycardia focus in the left ventricular summit through the left atrial appendage: a case report. European Heart Journal - Case Reports. 2018;2(4):1–5. https://doi.org/10.1093/ehjcr/yty110.
Igarashi, M., Nogami, A., Fukamizu, S., Sekiguchi, Y., Nitta, J., Sakamoto, N., … Ieda, M. (2020). Acute and long-term results of bipolar radiofrequency catheter ablation of refractory ventricular arrhythmias of deep intramural origin. Heart Rhythm,
Whiteman, S.; Saker, E.; Courant, E.; Salandy, S.; Gielecki, J.; Zurada, A.; Loukas, M. An anatomical review of the left atrium, Translational Research in Anatomy, 2019, Volume 17, 100052, ISSN 2214-854X, https://doi.org/10.1016/j.tria.2019.100052
Beigel R, Wunderlich NC, Ho SY, Arsanjani R, Siegel RJ. The left atrial appendage: anatomy, function, and noninvasive evaluation. JACC Cardiovasc Imaging. 2014;7(12):1251–65. https://doi.org/10.1016/j.jcmg.2014.08.009 (PMID: 25496544).
Su P, McCarthy KP, Ho SY. Occluding the left atrial appendage: anatomical considerations. Heart. 2008;94:1166–70. https://doi.org/10.1136/hrt.2006.111989.
Wang Y, Di Biase L, Horton RP, et al. Left atrial appendage studied by computed tomography to help planning for appendage closure device placement. J Cardiovasc Electrophysiol. 2010;21(9):973–82. https://doi.org/10.1111/j.1540-8167.2010.01814.x,indexedinPubmed:20550614.
Korhonen M, Parkkonen J, Hedman M, Muuronen A, Onatsu J, Mustonen P, Vanninen R, Taina M. Morphological features of the left atrial appendage in consecutive coronary computed tomography angiography patients with and without atrial fibrillation. PLoS ONE. 2017;12(3): e0173703. https://doi.org/10.1371/journal.pone.0173703.PMID:28288200;PMCID:PMC5348027.
Kimura T, Takatsuki S, Inagawa K, Katsumata Y, Nishiyama T, Nishiyama N, Fukumoto K, Aizawa Y, Tanimoto Y, Tanimoto K, Jinzaki M, Fukuda K. Anatomical characteristics of the left atrial appendage in cardiogenic stroke with low CHADS2 scores. Heart Rhythm 2013;10:921–925.17(9), 1500–1507.
Wu L, Liang E, Fan S, Zheng L, Du Z, Liu S, Hu F, Fan X, Chen G, Ding L, Yao Y. Relation of left atrial appendage morphology determined by computed tomography to prior stroke or to increased risk of stroke in patients with atrial fibrillation. Am J Cardiol. 2019;123(8):1283–6. https://doi.org/10.1016/j.amjcard.2019.01.024 (Epub 2019 Jan 23 PMID: 30709597).
Wang K, Ho SY, Gibson DG, Anderson RH. Architecture of atrial musculature in humans. Br Heart J. 1995;73(6):559–65. https://doi.org/10.1136/hrt.73.6.559.PMID:7626357;PMCID:PMC483920.
Ho SY, Cabrera JA, Sanchez-Quintana D. Left atrial anatomy revisited. Circ Arrhythm Electrophysiol. 2012;5(1):220–8. https://doi.org/10.1161/CIRCEP.111.962720,indexedinPubmed:22334429.
Obel, O. A., Avila, A., Neuzil, P., Saad, E. B., Ruskin, J. N., & Reddy, V. Y. (2006). Ablation of left ventricular epicardial outflow tract tachycardia from the distal great cardiac vein. Journal of the American College of Cardiology, 48(9), 6–10. https://doi.org/10.1016/j.jacc.2006.06.006
Di Biase L, Santangeli P, Anselmino M, Mohanty P, Salvetti I, Gili S, Horton R, Sanchez JE, Bai R, Mohanty S, Pump A, Cereceda Brantes M, Gallinghouse GJ, Burkhardt JD, Cesarani F, Scaglione M, Natale A, Gaita F. Does the left atrial appendage morphology correlate with the risk of stroke in patients with atrial fibrillation? Results from a multicenter study. J Am Coll Cardiol. 2012;60(6):531–8. https://doi.org/10.1016/j.jacc.2012.04.032 (PMID: 22858289).
Lupercio F, Carlos Ruiz J, Briceno DF, et al. Left atrial appendage morphology assessment for risk stratification of embolic stroke in patients with atrial fibrillation: a meta-analysis. Heart Rhythm. 2016;13(7):1402–9. https://doi.org/10.1016/j.hrthm.2016.03.042.
Kimura T, Takatsuki S, Inagawa K, Katsumata Y, Nishiyama T, Nishiyama N, Fukumoto K, Aizawa Y, Tanimoto Y, Tanimoto K, Jinzaki M, Fukuda K. Anatomical characteristics of the left atrial appendage in cardiogenic stroke with low CHADS2 scores. Heart Rhythm. 2013;10(6):921–5. https://doi.org/10.1016/j.hrthm.2013.01.036 (Epub 2013 Feb 4 PMID: 23384894).
Enriquez A, Malavassi F, Saenz LC, Supple G, Santangeli P, Marchlinski FE, Garcia FC. How to map and ablate left ventricular summit arrhythmias. Heart Rhythm. 2017;14(1):141–8.
Altmann DR, Knecht S, Sticherling C, Ammann P, Osswald S, Kühne M. Ventricular tachycardia originating from the “ Bermuda Triangle.” Cardiovascular Medicine. 2013;16(7–8):208–10.
Żabówka A, Hołda J, Strona M, Koziej M, Krawczyk-Ożóg A, Jasińska KA, Kuniewicz M, Lelakowski J, Hołda MK. Morphology of the Vieussens valve and its imaging in cardiac multislice computed tomography. J Cardiovasc Electrophysiol. 2019;30(8):1325–9. https://doi.org/10.1111/jce.14018 (Epub 2019 Jun 18 PMID: 31187551).
Mazur M, Żabówka A, Bolechała F, Kopacz P, Klimek-Piotrowska W, Hołda MK. Variations and angulation of the coronary sinus tributaries: implications for left ventricular pacing. Pacing Clin Electrophysiol. 2019;42(4):423–30. https://doi.org/10.1111/pace.13618 (Epub 2019 Feb 21 PMID: 30740749).
Singh M, Edwards WD, Holmes DR Jr, Tajil AJ, Nishimura RA. Anatomy of the first septal perforating artery: a study with implications for ablation therapy for hypertrophic cardiomyopathy. Mayo Clin Proc. 2001;76(8):799–802 (PMID: 11499819).
Author information
Authors and Affiliations
Contributions
M.K.: concept and design, anatomical dissections, photography, data collection, writing manuscript. B.K., D.M., J.N., C.N., D.R., G.M., W.T.: anatomical dissections, photography, data collection, English language support. H.D.: revising article critically for important intellectual content, English language support. M.H.: providing important intellectual content. J.W.: revising article critically for important intellectual content, final approval of submitted version. All authors have approved the final article.
Corresponding author
Ethics declarations
Ethics approval
This study was conducted at the Department of Anatomy of the Jagiellonian University Medical College and was approved by the Bioethical Committee of the Jagiellonian University in Cracow, Poland (1072.6120.131.2018). The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. The methods were carried out in accordance with the approved guidelines.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kuniewicz, M., Budnicka, K., Dusza, M. et al. Gross anatomic relationship between the human left atrial appendage and the left ventricular summit region: implications for catheter ablation of ventricular arrhythmias originating from the left ventricular summit. J Interv Card Electrophysiol 66, 301–310 (2023). https://doi.org/10.1007/s10840-022-01172-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01172-6