Abstract
Background
The study aimed to explore the resolution of left atrial and left atrial appendage (LAA) spontaneous echo-contrast or thrombus in patients with nonvalvular atrial fibrillation/flutter (AF/AFL) under chronic oral anticoagulation (OAC).
Methods
A single-center retrospective analysis of patients who underwent a transesophageal echocardiography (TOE) for an electrical cardioversion was conducted.
Results
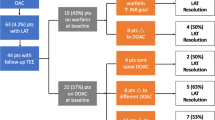
Among 277 TOE performed, 73 cases (26%) of LAA echo-contrast or thrombus were detected, 53 patients with LAA/LA echo-contrast (19%) and 20 (7%) with a thrombus. All patients were under chronic anticoagulation with a VKA (65%) or with a NOAC (35%). The Echo-contrast Group maintained the same OAC strategy in 49 patients (93%). The Thrombus Group kept the same OAC strategy with a NOAC in 6 cases (30%) and changed the strategy in 14 patients (70%), titrating NOAC dose in 1 (5%) and the VKA dose in 4 (20%) and switching from NOAC to VKA in 5 (25%), from VKA to NOAC in 3 (15%), and from NOAC to NOAC in 1 (5%). Smoke resolution was observed in 4/40 cases (10%) of the smoke group and thrombus resolution in 8/15 (53%) of the thrombus group. Patients with thrombus resolution had a lower CHA2DS2-Vasc score (3.5 ± 2 vs 4 ± 1, p = 0.05), were more often under NOAC (37.5 vs 28%, p = 0.07), and had a longer anticoagulation time (7.5 vs 4 months, p = 0.08).
Conclusion (s)
Changing OAC strategy is associated with thrombus resolution in more than 50% of chronically anticoagulated patients.


Similar content being viewed by others
Data availability
Data collected using the Estensa Software in use at the Azienda Ospedaliero Universitaria Pisana, University Hospital of Pisa.
Abbreviations
- AF:
-
Atrial fibrillation
- AFL:
-
Atrial flutter
- LA:
-
Left atrium
- LAA:
-
Left atrial appendage
- LVEF:
-
Left ventricular ejection fraction
- NOAC:
-
Direct oral anticoagulants
- OAC:
-
Oral anticoagulation
- SEC:
-
Spontaneous echo-contrast
- TEE:
-
Transesophageal echocardiography
- VKA:
-
Vitamin K anticoagulant
References
Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Europace. 2016;18(11):1609–78.
Al-Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999;82:547–54.
Watson T, Shantsila E, Lip GY. Mechanisms of thrombo-genesis in atrial fibrillation: Virchow’s triad revisited. Lancet. 2009;373:155–66.
Al Saady NM, Obel OA, Camm AJ. Left atrial appendage: structure, function, and role in thromboembolism. Heart. 1999;82:547–54.
Hohnloser SH, Basic E, Nabauer M. Uptake in anti-thrombotic treatment and its association with stroke incidence in atrial fibrillation: insights from a large German claims database. Clin Res Cardiol. 2019;108:1042–52.
McNamara K, Witry M, Bryant G, et al. A prospective, multi-center cohort study: investigating the ability of warfarin-treated patients to predict their INR. Clin Res Cardiol. 2019;108:212–7.
Lip GY, Hammerstingl C, Marin F, et al. Left atrial thrombus resolution in atrial fibrillation or flutter: results of a prospective study with rivaroxaban (X-TRA) and a retrospective observational registry providing baseline data (CLOT-AF). Am Heart J. 2016;178:126–34.
Beppu S, Nimura Y, Sakakibara H, Nagata S, Park YD, Izumi S. Smoke-like echo in the left atrial cavity in mitral valve disease: its features and significance. J Am Coll Cardiol. 1985;6:744–9.
Troughton RW, Asher CR, Klein AL. The role of echocardiography in atrial fibrillation and cardioversion. Heart. 2003;89:1447–54.
Erwan Donal, Gregory Y H Lip, Maurizio Galderisi, Andreas Goette, Dipen Shah, Mohamed Marwan, Mathieu Lederlin, Sergio Mondillo, Thor Edvardsen, Marta Sitges, Julia Grapsa, Madalina Garbi, Roxy Senior, Alessia Gimelli, Tatjana S Potpara, Isabelle C Van Gelder, Bulent Gorenek, Philippe Mabo, Patrizio Lancellotti, Karl-Heinz Kuck, Bogdan A Popescu, Gerhard Hindricks, Gilbert Habib, Bernard Cosyns, Victoria Delgado, Kristina H. Haugaa, Denisa Muraru, Koen Nieman, Ariel Cohen, Document Reviewers: For EACVI:, For EHRA:, EACVI/EHRA Expert Consensus Document on the role of multi-modality imaging for the evaluation of patients with atrial fibrillation. Eur Heart J Cardiovasc Imaging. 2016;17: 355–383.
Douglas PS, Garcia MJ, Haines DE et al. ACCF/ASE/AHA/ ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR. Appropriate use criteria for echocardiography. a report of the American college of cardiology foundation appropriate use criteria task force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardio- vascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011;57:1126–66.
Gottdiener JS, Bednarz J, Devereux R, et al. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J Am Soc Echocardiogr. 2004;17:1086–119.
Bozkurt B, Coats AJS, Tsutsui H, Abdelhamid CM, Adamopoulos S, Albert N, Anker SD, Atherton J, Böhm M, Butler J, Drazner MH, Michael Felker G, Filippatos G, Fiuzat M, Fonarow GC, Gomez-Mesa JE, Heidenreich P, Imamura T, Jankowska EA, Januzzi J, Khazanie P, Kinugawa K, Lam CSP, Matsue Y, Metra M, Ohtani T, Francesco Piepoli M, Ponikowski P, Rosano GMC, Sakata Y, Seferović P, Starling RC, Teerlink JR, Vardeny O, Yamamoto K, Yancy C, Zhang J, Zieroth S. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur J Heart Fail. 2021;23(3):352–80.
Kaatz S, Ahmad D, Spyropoulos AC, Schulman S. Definition of clinically relevant non-major bleeding in studies of anticoagulants in atrial fibrillation and venous thromboembolic disease in non-surgical patients: communication from the SSC of the ISTH. J Thromb Haemost. 2015;13:2119–26.
Kapłon-Cieślicka A, Budnik M, Gawałko M, Peller M, Gorczyca I, Michalska A, Babiarz A, Bodys A, Uliński R, Żochowski M, Scisło P, Kochanowski J, Filipiak KJ, Opolski G. Atrial fibrillation type and renal dysfunction as important predictors of left atrial thrombus. Heart. 2019;105(17):1310–5.
Kapłon-Cieślicka A, Budnik M, Gawałko M, Peller M, Gorczyca I, Michalska A, Babiarz A, Bodys A, Uliński R, Żochowski M, Scisło P, Kochanowski J, Filipiak KJ, Opolski G. Atrial fibrillation type and renal dysfunction as important predictors of left atrial thrombus. Heart. 2019;105(17):1310–5.
Budnik M, Gawałko M, Gorczyca I, Uziębło-Życzkowska B, Krzesiński P, Kochanowski J, Scisło P, Michalska A, Jelonek O, Starzyk K, Jurek A, Kiliszek M, Wożakowska-Kapłon B, Gielerak G, Filipiak KJ, Opolski G, Kapłon-Cieślicka A. Risk of left atrial appendage thrombus in patients with atrial fibrillation and chronic kidney disease. Cardiol J. 2020.
Ellis K, Ziada KM, Vivekananthan D, Latif AA, Shaaraoui M, Martin D, Grimm RA. Transthoracic echocardiographic predictors of left atrial appendage thrombus. Am J Cardiol. 2006;97(3):421–5.
Schotten U, Verheule S, Kirchhof P, Goette A. Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol Rev. 2011;91:265–325.
Kapłon-Cieślicka A, Budnik M, Gawałko M, Peller M, Gorczyca I, Michalska A, Babiarz A, Bodys A, Uliński R, Żochowski M, Scisło P, Kochanowski J, Filipiak KJ, Opolski G. Atrial fibrillation type and renal dysfunction as important predictors of left atrial thrombus. Heart. 2019;105(17):1310–5.
Di Cori A, Auricchio A, Regoli F, Blomström-Lundqvist C, Butter C, Dagres N, Deharo JC, Maggioni AP, Kutarski A, Kennergren C, Laroche C, Rinaldi CA, Dovellini EV, Golzio PG, Thøgersen AM, Bongiorni MG, ESC-EHRA ELECTRa Investigators. Clinical impact of antithrombotic therapy in transvenous lead extraction complications: a sub-analysis from the ESC-EORP EHRA ELECTRa (European Lead Extraction ConTRolled) Registry. Europace. 2019;21(7):1096–105.
ProvidenciaR TrigoJ, PaivaL BarraS. The role of echocardiography in thromboembolic risk assessment of patients with nonvalvular atrial fibrillation. J Am Soc Echocardiogr. 2013;26:801–12.
Bertaglia E, Anselmino M, Zorzi A, Russo V, Toso E, Peruzza F, Rapacciuolo A, Migliore F, Gaita F, Cucchini U, De Divitiis M, Iliceto S, Stabile G. NOACs and atrial fibrillation: incidence and predictors of left atrial thrombus in the real world. Int J Cardiol. 2017;15(249):179–83.
Kapłon-Cieślicka A, Budnik M, Gawałko M, Peller M, Gorczyca I, Michalska A, Babiarz A, Bodys A, Uliński R, Żochowski M, Scisło P, Kochanowski J, Filipiak KJ, Opolski G. Atrial fibrillation type and renal dysfunction as important predictors of left atrial thrombus. Heart. 2019;105(17):1310–5.
Ellis K, Ziada KM, Vivekananthan D, Latif AA, Shaaraoui M, Martin D, Grimm RA. Transthoracic echocardiographic predictors of left atrial appendage thrombus. Am J Cardiol. 2006;97(3):421–5.
Donal E, Sallach JA, Murray RD, Drinko JK, Jasper SE, Thomas JD, et al. Contrast-enhanced tissue Doppler imaging of the left atrial appendage is a new quantitative measure of spontaneous echocardiographic contrast in atrial fibrillation. Eur J Echocardiogr. 2008;9:5–11.
Sallach JA, Puwanant S, Drinko JK, Jaffer S, Donal E, Thambidorai SK, et al. Comprehensive left atrial appendage optimization of thrombus using surface echocardiography: the CLOTS multicenter pilot trial. J Am Soc Echocardiogr. 2009;22:1165–72.
Troughton RW, Asher CR, Klein AL. The role of echocardiography in atrial fibrillation and cardioversion. Heart. 2003;89:1447–54.
Bernhardt P, Schmidt H, Hammerstingl C, Hackenbroch M, Sommer T, Lüderitz B, Omran H. Fate of left atrial thrombi in patients with atrial fibrillation determined by transesophageal echocardiography and cerebral magnetic resonance imaging. Am J Cardiol. 2004;94(6):801–4.
Lee WC, Fang CY, Chen YL, Fang HY, Chen HC, Liu WH, Fu M, Chen MC. Left atrial or left atrial appendage thrombus resolution after adjustment of oral anticoagulant treatment. J Stroke Cerebrovasc Dis. 2019;28(1):90–6.
Zzymanski FM, Lip GY, Filipiak KJ, Platek AE, Hrynkiewicz-Szymanska A, Opolski G. Stroke risk factors beyond the CHA2DS2-VASc score: can we improve our identification of “high stroke risk” patients with atrial fibrillation? Am J Cardiol. 2015;116:1781–8.
Kim D, Yang PS, Jang E, Yu HT, Kim TH, Uhm JS, Kim JY, Sung JH, Pak HN, Lee MH, Lip GYH, Joung B. The optimal drug adherence to maximize the efficacy and safety of non-vitamin K antagonist oral anticoagulant in real-world atrial fibrillation patients. Europace. 2020;22(4):547–57.
Klein AL, Grimm RA, Jasper SE, Murray RD, Apperson-Hansen C, Lieber EA, et al. Efficacy of transesophageal echocardiography-guided cardioversion of patients with atrial fibrillation at 6 months: a randomized controlled trial. Am Heart J. 2006;151:380–9.
Author information
Authors and Affiliations
Contributions
Concept/design—Andrea Di Cori, Maria Grazia Bongiorni, Giulio Zucchelli.
Data analysis/interpretation—Andrea Di Cori, Laura Meola.
Drafting article—Andrea Di Cori, Valentina Barletta.
Critical revision of article—Giulio Zucchelli, Maria Grazia Bongiorni, Stefano Viani, Luca Segreti, Raffaele De Lucia, Ezio Soldati.
Approval of article—all authors.
Statistics—Matteo Parollo, Laura Meola, Lorenzo Mazzocchetti.
Data collection—Laura Meola, Giulia Branchitta, Tea Cellamaro, Marisa Carluccio, Francesco Gentile. All authors contributed to the study conception and design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
The participant has consented to the data collection and analysis. No patient’s identifying information is included in this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Cori, A., Barletta, V., Meola, L. et al. Left atrial thrombus and smoke resolution in patients with atrial fibrillation under chronic oral anticoagulation. J Interv Card Electrophysiol 64, 773–781 (2022). https://doi.org/10.1007/s10840-022-01169-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01169-1