Abstract
Purpose
Distinguishing between left bundle branch pacing (LBBP) and left ventricular septal pacing (LVSP) is challenging. This study aimed to compare the echocardiographic distance from the pacing lead tip to the left ventricular (LV) septal endocardium between patients who underwent LBBP and those who underwent LVSP successfully.
Methods
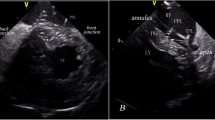
Fifty-nine consecutive patients (age 71.9 ± 12.0 years, 35.6% male) with traditional indications for permanent cardiac pacing were included (LBBP group, n = 46; LVSP group, n = 13). Unipolar pacing from the final pacing sites generated narrow QRS complexes with a right bundle branch block pattern in all patients. After the procedure, a physician blinded to the group allocation performed echocardiographic measurements of the distance between the lead tip and the LV septal endocardium.
Results
The mean paced QRS duration was comparable between the LBBP group and the LVSP group (105.3 ± 15.6 ms vs. 109.2 ± 9.6 ms, P = 0.287). In the LBBP group, the interval from the left bundle branch potential to QRS onset was 28.7 ± 9.0 ms. During diastole, the mean distance between the lead tip and the LV septal endocardium was 0.6 ± 0.9 mm in the LBBP group and 3.0 ± 1.6 mm in the LVSP group (P < 0.001). During systole, the distance was 1.5 ± 1.4 mm in the LBBP group and 4.3 ± 2.6 mm in the LVSP group (P < 0.001).
Conclusions
The landing zone of the lead tip was closer to the LV septal endocardium in the patients who underwent LBBP. There is a need for real-time intraprocedural monitoring of the distance between the lead tip and the LV septal endocardium when performing LBBP.



Similar content being viewed by others
Data Availability
Data are available from the corresponding author upon reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- AVB:
-
Atrioventricular block
- ECG:
-
Electrocardiography
- EGM:
-
Electrogram
- HBP:
-
His bundle pacing
- LAO30°:
-
Left anterior oblique 30°
- LBB:
-
Left bundle branch
- LBBB:
-
Left bundle branch block
- LBBP:
-
Left bundle branch pacing
- LV:
-
Left ventricular
- LVAT:
-
Left ventricular activation time
- LVEDd:
-
Left ventricular end-diastolic dimension
- LVEF:
-
Left ventricular ejection fraction
- LVESd:
-
Left ventricular end-systolic dimension
- LVSP:
-
Left ventricular septal pacing
- MR:
-
Mitral regurgitation
- RAO30°:
-
Right anterior oblique 30°
- RBBB:
-
Right bundle branch block
- RV:
-
Right ventricular
- Stim-LVAT:
-
Stimulus to left ventricular activation time (interval from stimulus to LV activation)
- TR:
-
Tricuspid regurgitation
References
Su L, Wang S, Wu S, Xu L, Huang Z, Chen X, Zheng R, et al. Long-term safety and feasibility of left bundle branch pacing in a large single-center study[J]. Circ Arrhythm Electrophysiol. 2021;14(2):e9261. https://doi.org/10.1161/CIRCEP.120.009261.
Chen X, Jin Q, Bai J, Wang W, Qin S, Wang J, Liang Y, et al. The feasibility and safety of left bundle branch pacing vs. right ventricular pacing after mid-long-term follow-up: a single-centre experience[J]. Europace. 2020;22(Suppl_2):i36–44. https://doi.org/10.1093/europace/euaa294.
Li X, Li H, Ma W, Ning X, Liang E, Pang K, Yao Y, et al. Permanent left bundle branch area pacing for atrioventricular block: feasibility, safety, and acute effect[J]. Heart Rhythm. 2019;16(12):1766–73. https://doi.org/10.1016/j.hrthm.2019.04.043.
Wu S, Chen X, Wang S, Xu L, Xiao F, Huang Z, Zheng R, et al. Evaluation of the criteria to distinguish left bundle branch pacing from left ventricular septal pacing[J]. JACC Clin Electrophysiol. 2021. https://doi.org/10.1016/j.jacep.2021.02.018.
Hou X, Qian Z, Wang Y, Qiu Y, Chen X, Jiang H, Jiang Z, et al. Feasibility and cardiac synchrony of permanent left bundle branch pacing through the interventricular septum[J]. Europace. 2019;21(11):1694–702. https://doi.org/10.1093/europace/euz188.
Heckman LIB, Luermans JGLM, Curila K, Van Stipdonk AMW, Westra S, Smisek R, Prinzen FW, et al. Comparing ventricular synchrony in left bundle branch and left ventricular septal pacing in pacemaker patients[J]. J Clin Med, 2021,10(4). https://doi.org/10.3390/jcm10040822.
Vijayaraman P, Nayak HM, Ellenbogen KA. Left ventricular septal versus left bundle branch pacing: a new beginning in cardiac resynchronization therapy? [J]. J Am Coll Cardiol. 2020;75(4):360–2. https://doi.org/10.1016/j.jacc.2019.11.041.
Writing Committee Members, Kusumoto FM, Schoenfeld MH, Barrett C, Edgerton JR, Ellenbogen KA, Gold MR, Goldschlager NF, et al. 2018 ACC/AHA/HRS guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society[J]. Heart Rhythm. 2019;16(9):e128–226. https://doi.org/10.1016/j.hrthm.2018.10.037.
Huang W, Chen X, Su L, Wu S, Xia X, Vijayaraman P. A beginner’s guide to permanent left bundle branch pacing[J]. Heart Rhythm. 2019;16(12):1791–6. https://doi.org/10.1016/j.hrthm.2019.06.016.
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC, Horton K, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography[J]. J Am Soc Echocardiogr. 2019;32(1):1–64. https://doi.org/10.1016/j.echo.2018.06.004.
Writing Committee Members, Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[J]. J Am Coll Cardiol. 2021;77(4):450–500. https://doi.org/10.1016/j.jacc.2020.11.035.
Salden FCWM, Luermans JGLM, Westra SW, Weijs B, Engels EB, Heckman LIB, Lamerichs LJM, et al. Short-term hemodynamic and electrophysiological effects of cardiac resynchronization by left ventricular septal pacing[J]. J Am Coll Cardiol. 2020;75(4):347–59. https://doi.org/10.1016/j.jacc.2019.11.040.
Curila K, Jurak P, Jastrzebski M, Prinzen F, Waldauf P, Halamek J, Vernooy K, et al. Left bundle branch pacing compared to left ventricular septal myocardial pacing increases interventricular dyssynchrony but accelerates left ventricular lateral wall depolarization[J]. Heart Rhythm. 2021;18(8):1281–9. https://doi.org/10.1016/j.hrthm.2021.04.025.
Vijayaraman P, Subzposh FA, Naperkowski A, Panikkath R, John K, Mascarenhas V, Bauch TD, et al. Prospective evaluation of feasibility and electrophysiologic and echocardiographic characteristics of left bundle branch area pacing[J]. Heart Rhythm. 2019;16(12):1774–82. https://doi.org/10.1016/j.hrthm.2019.05.011.
Chen X, Wu S, Su L, Su Y, Huang W. The characteristics of the electrocardiogram and the intracardiac electrogram in left bundle branch pacing[J]. J Cardiovasc Electrophysiol. 2019;30(7):1096–101. https://doi.org/10.1111/jce.13956.
Jastrzębski M, Kiełbasa G, Curila K, Moskal P, Bednarek A, Rajzer M, Vijayaraman P. Physiology-based electrocardiographic criteria for left bundle branch capture[J]. Heart Rhythm. 2021;18(6):935–43. https://doi.org/10.1016/j.hrthm.2021.02.021.
Jiang Z, Chang Q, Wu Y, Ji L, Zhou X, Shan Q. Typical BBB morphology and implantation depth of 3830 electrode predict QRS correction by left bundle branch area pacing[J]. Pacing Clin Electrophysiol. 2020;43(1):110–7. https://doi.org/10.1111/pace.13849.
Zhang J, Wang Z, Zu L, Cheng L, Su R, Wang X, Liang Z, et al. Simplifying physiological left bundle branch area pacing using a new nine-partition method[J]. Can J Cardiol. 2021;37(2):329–38. https://doi.org/10.1016/j.cjca.2020.05.011.
Feng XF, Zhang PP, Liu B, Zhao Y, Lu QF, Li YG. Permanent left bundle branch area pacing utilizing intracardiac echocardiogram[J]. BMC Cardiovasc Disord. 2020;20(1):377. https://doi.org/10.1186/s12872-020-01649-0.
Vijayaraman P, Panikkath R. Intracardiac echocardiography-guided left bundle branch pacing in a patient with tricuspid valve replacement[J]. J Cardiovasc Electrophysiol. 2019;30(11):2525–7. https://doi.org/10.1111/jce.14205.
Jastrzębski M, Moskal P, Hołda MK, Strona M, Bednarek A, Kiełbasa G, Czarnecka D. Deep septal deployment of a thin, lumenless pacing lead: a translational cadaver simulation study[J]. Europace. 2020;22(1):156–61. https://doi.org/10.1093/europace/euz270.
Funding
This study was supported by grants from Beijing Natural Science Foundation (Grant No. 7202050).
Author information
Authors and Affiliations
Contributions
Concept/design: Xing-Peng Liu. Data collection: Xin-Yi Peng, Yan-Jiang Wang, Lan-Lan Sun. Procedure performing: Xing-Peng Liu, Ying Tian, Liang Shi, Yan-Jiang Wang. Data analysis/interpretation: Xin-Yi Peng, Chao-Di Cheng, Li-Hong Huang. Drafting article: Xin-Yi Peng. Critical revision of the article: Xing-Peng Liu, Ying Tian. Approval of article, statistics: Ying Tian. Funding secured by: Xing-Peng Liu.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Each participant has agreed to be included in this research by giving written or oral informed consent. The scope and methods of this study were approved by the Ethics Committee of Beijing Chaoyang Hospital before patients were included.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peng, XY., Wang, YJ., Sun, LL. et al. Is the pacing site closer to the left ventricular septal endocardium in left bundle branch pacing or in left ventricular septal pacing?. J Interv Card Electrophysiol 66, 539–549 (2023). https://doi.org/10.1007/s10840-022-01143-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01143-x