Abstract
Purpose
In this study, we analyzed PFO implications in atrial fibrillation (AF) ablation.
Methods
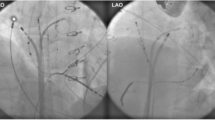
Six hundred and twenty-five consecutive patients with AF undergoing PV isolation were included. We considered that a large and/or compliant PFO was present if the catheters advanced gently into the LA without puncturing the septum. Atrial tachyarrhythmias after the 3-month blanking period were classified as a recurrence.
Results
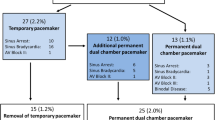
Out of the 625 patients included, 36 (5.8%) were found to have PFO. No significant differences were observed in the clinical characteristics of patients with PFO compared with patients without PFO. Nevertheless, patients with PFO had lower acute success in PV isolation compared with patients without PFO (98.2% vs. 88.5%; p = 0.006) even after adjusting for age, sex, type of AF, LA area, cardiomyopathy, time from AF diagnosis to the ablation, and ablation technique (odds ratio: 0.1; 95% confidence interval (CI): 0.02–0.9; p = 0.039). In 546 patients followed more than 6 months, the recurrence rate of any atrial tachyarrhythmia after 18.6 ± 11.9 months was significantly higher in patients with PFO compared with patients without PFO (41.9 vs. 70%; p = 0.012). This difference remained significant after adjusting for age, sex, type of AF, LA area, cardiomyopathy, time from AF diagnosis to the ablation, and ablation technique (hazard ratio: 1.9; 95% CI: 1.1–3.3; p = 0.015).
Conclusions
The presence of a large and/or compliant PFO is an independent factor for PV isolation failure and arrhythmia recurrence rate after the ablation.


Similar content being viewed by others
Data availability
We declare that the data of this study are available for any request.
Code availability
Not applicable
References
Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. J Interv Card Electrophysiol. 2012;33:171–257.
Arya A, Hindricks G, Sommer P, et al. Long-term results and the predictors of outcome of catheter ablation of atrial fibrillation using steerable sheath catheter navigation after single procedure in 674 patients. Europace. 2010;12:173–80.
Kuck KH, Brugada J, Fürnkranz A, FIRE AND ICE Investigators, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235–45.
Kircher S, Arya A, Altmann D, et al. Individually tailored vs. standardized substrate modification during radiofrequency catheter ablation for atrial fibrillation: a randomized study. Europace. 2017. https://doi.org/10.1093/europace/eux310.
Calkins H, Reynolds MR, Spector P, et al. Treatment of atrial fibrillation with antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews and meta-analyses. Circ Arrhythm Electrophysiol. 2009;2:349–61.
Cappato R, Calkins H, Chen SA, et al. Updated worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3:32–8.
Liu X, Dong J, Mavrakis HE, Hu F, et al. Achievement of pulmonary vein isolation in patients undergoing circumferential pulmonary vein ablation: a randomized comparison between two different isolation approaches. J Cardiovasc Electrophysiol. 2006;17:1263–70.
Barrio-López MT, Castellanos E, Ortiz M, et al. Atrial mapping during pulmonary vein pacing to detect conduction gaps in a second pulmonary vein isolation procedure. J Interv Card Electrophysiol. 2018;53:195–205.
Barrio-Lopez MT, Sanchez-Quintana D, Garcia-Martinez J, et al. Epicardial connections involving pulmonary veins: the prevalence, predictors, and implications for ablation outcome. Circ Arrhythm Electrophysiol. 2020;13:e007544.
Bisbal F, Alarcón F, Ferrero-De-Loma-Osorio A, et al. Diagnosis-to-ablation time in atrial fibrillation: a modifiable factor relevant to clinical outcome. J Cardiovasc Electrophysiol. 2019;30:1483–90.
Schwartzman D, Ren JF, Devine WA, Callans DJ. Cardiac swelling associated with linear radiofrequency ablation in the atrium. J Interv Card Electrophysiol. 2001;5:159–66.
Knecht S, Wright M, Lellouche N, et al. Impact of a patent foramen ovale on paroxysmal atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2008;19:1236–41.
Sweda R, Haeberlin A, Seiler J, et al. How to reach the left atrium in atrial fibrillation ablation?: patent foramen ovale versus transseptal puncture. Circ Arrhythm Electrophysiol. 2019;12:e006744.
Barrio-López T, Ortiz M, Castellanos E, et al. Relationship between left atrium catheter contact force and pacing threshold. J Interv Card Electrophysiol. 2017;49:147–55.
Arentz T, Weber R, Bürkle G, et al. Small or large isolation areas around the pulmonary veins for the treatment of atrial fibrillation? Results from a prospective randomized study. Circulation. 2007;115:3057–63.
Kuck KH, Brugada J, Fürnkranz A, FIRE AND ICE Investigators, et al. Cryoballoon or radiofrequency ablation for paroxysmal atrial fibrillation. N Engl J Med. 2016;374:2235–45.
Wilber Su, Kowal R, Kowalski M, et al. Best practice guide for cryoballoon ablation in atrial fibrillation: the compilation experience of more than 3000 procedures. Heart Rhythm. 2015;12:1658–66.
Hagen P, Scholz D, Edwards W. Incidence and size of patent foramen ovale during the first 10 decades of life: an autopsy study of 965 normal hearts. Mayo Clin Proc. 1984;59:17–20.
Fisher DC, Fisher EA, Budd JH, Rosen SE, Goldman ME. The incidence of patent foramen ovale in 1,000 consecutive patients: a contrast transesophageal echocardiography study. Chest. 1995;107:1504–9.
Meissner I, Whisnant JP, Khandheria BK, et al. Prevalence of potential risk factors for stroke assessed by transesophageal echocardiography and carotid ultrasonography: the SPARC study. Stroke Prevention: Assessment of Risk in a Community. Mayo Clin Proc. 1999;74:862–9.
Homma S, Sacco RL. Patent foramen ovale and stroke. Circulation. 2005;112:1063–72.
Ho SY, McCarthy KP, Rigby ML. Morphological features pertinent to interventional closure of patent oval foramen. J Interv Cardiol. 2003;16:33–8.
Marshall AC, Lock JE. Structural and compliant anatomy of the patent foramen ovale in patients undergoing transcatheter closure. Am Heart J. 2000;140:303–7.
Naqvi N, McCarthy KP, Ho SY. Anatomy of the atrial septum and interatrial communications. J Thorac Dis. 2018;10(Suppl 24):S2837–47.
Naqvi N, McCarthy KP, Ho SY. Anatomy of the atrial septum and interatrial communications. J Thorac Dis. 2018;10(Suppl 24):S2837–47.
Lehrmann H, Schneider J, Jadidi AS, et al. Transseptal access for left atrial ablation: the catheter-probing techniques are not without risk. J Cardiovasc Electrophysiol. 2014;25:479–84.
Funding
This work is funded by the Spanish Government Official Agency for funding biomedical research-Instituto de Salud Carlos III (ISCIII), with competitive grants through the Fondo de Investigación Sanitaria y Fondo Europeo de Desarrollo Regional (PI17/00718, PI17/ 00748, PI17/01870), and the Spanish Society of Cardiology (FEC/ 2017).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Hospital Ethics Committee.
Consent to participate
Given the retrospective nature of the study, it was not considered compulsory to obtain a specific informed consent.
Consent for publication
All authors have given their consent to publish this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Barrio-Lopez, M.T., Castellanos, E., Betancur, A. et al. The presence of a large patent foramen ovale reduces acute and chronic success in atrial fibrillation ablation. J Interv Card Electrophysiol 64, 705–713 (2022). https://doi.org/10.1007/s10840-022-01134-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01134-y