Abstract
Purpose
Left ventricular outflow tract (LVOT) arrhythmias are commonly targeted from the aortic sinuses of Valsalva (SOV). Both presystolic potentials during ventricular arrhythmia (VA) and late diastolic potentials during sinus rhythm have been recognized as markers of successful ablation sites. The study aimed to evaluate the utility of high resolution mapping (HRM) with small and closely spaced electrodes for guiding ablation of VA from the SOV.
Methods
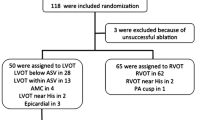
Seventeen patients with LVOT VA underwent HRM in the SOV with either PentaRay (13) or Orion (4) catheters. Ablation was guided by low amplitude high frequency potentials that were identified with HRM and tagged on the electroanatomic map.
Results
High frequency low amplitude potentials during sinus rhythm (late) or VA (early) were demonstrated with HRM in all 17 consecutive patients; while these potentials were either absent or usually had a far-field appearance in the recordings obtained at the same sites with a 3.5-mm standard ablation catheter. On intracardiac echocardiogram, sites with these potentials corresponded to the bases of the sinuses adjacent to the LV ostium. Ablation was acutely successful in 16 out of 17 patients. Significant reduction in VA burden (≥ 90%) was noted in 15 patients.
Conclusions
High frequency low amplitude potentials during sinus rhythm (late) and VA (early) are consistently recorded using HRM in the SOV in patients with VA arising from the aortic sinuses of Valsalva. Standard ablation catheters have limited resolution for detecting these potentials. HRM may potentially improve outcomes of ablation of VA originating from the aortic SOV.





Similar content being viewed by others
References
Yamada T, McElderry T, Doppalapudi H, et al. Idiopathic ventricular arrhythmias originating from the aortic root: prevalence, electrocardiographic and electrophysiologic characteristics, and results of radiofrequency catheter ablation. J Am Coll Cardiol. 2008;52:139–47.
Hayashi T, Liang JL, Shirai Y, et al. Trends in successful ablation sites and outcomes of ablation for idiopathic outflow tract ventricular arrhythmia. J Am Coll Cardiol EP. 2020;6:221–30.
Latchamsetty R, Yokokawa M, Morady F, et al. Multicenter outcomes for catheter ablation of idiopathic premature ventricular complexes. J Am Coll Cardiol EP. 2015;1:116–23.
Anderson R. Clinical anatomy of the aortic root. Heart. 2000;84:670–3.
Yamada T, Litovsky SH, Neal KG. The left ventricular ostium: an anatomic concept relevant to idiopathic ventricular arrhythmia. Circ Arrhythmia Electrophysiol. 2008;1:396–404.
Quyang F, Fotuhi P, Yen S, et al. Repetitive monomorphic ventricular tachycardia originating from the aortic sinus cusp. J Am Coll Cardiol. 2002;39:500–8.
Tada H, Naito S, Ito S, et al. Significance of two potentials for predicting successful catheter ablation from the left sinus of Valsalva for left ventricular epicardial tachycardia. Pacing Clin Electrophysiol. 2004;27:1053–9.
Srivathsan KS, Bunch J, Asirvatham SJ, et al. Mechanism and utility of discrete arterial potentials in the ablation of outflow tract ventricular arrhythmia. Circ Arrhythmia Electrophysiol. 2008;1:30–8.
Hachiya H, Yamauchi Y, Iesaka Y, et al. Discrete potentials as an indicator of successful ablation in patients with coronary cusp ventricular arrhythmia. Circ Arrhythmia Electrophysiol. 2013;6:898–904.
Berte B, Relan J, Sacher F, et al. Impact of electrode type on mapping of scar related VT. J Cardiovasc Electrophysiol. 2015;26:1213–23.
Anter E, McElderry TH, Conteras-Valdes FM, et al. Evaluation of a novel high-resolution mapping technology for ablation of recurrent scar-related atrial tachycardias. Heart Rhythm. 2016;13:2048–55.
Tschabrunn CM, Roujol S, Dorman NC, Nezafat R, Josephson ME, Anter E. High-resolution mapping of ventricular scar: comparison between single and multielectrode catheter. Circ Arrhythmia Electrophysiol. 2016;9:e003841.
Betensky BP, Park RE, Marchlinski FE, et al. The V (2) transition ratio: a new electrocardiographic criterion for distinguishing left from right outflow tract tachycardia origin. J Am Coll Cardiol. 2011;57:2255–62.
Yamada T, Murakami Y, Yoshida N, et al. Preferential conduction across the ventricular outflow septum in ventricular arrhythmias originating from the aortic sinus cusp. J Am Coll Cardiol. 2007;50:884–91.
Kapa S, Mehra N, Deshmukh AJ, Friedman PA, Asirvatham SJ. Left sinus of Valsalva-Electroanatomic basis and outcomes with ablation for outflow tract arrhythmias. J Cardiovasc Electrophysiol. 2020;4:952–9.
Hasdemir C, Aktas S, Govsa F, et al. Demonstration of ventricular myocardial extensions into the pulmonary artery and aorta beyond the ventriculo-arterial junction. Pacing Clin Electrophysiol. 2007;30:534–9.
Anderson RH, Mohun TJ, Sanchez-Quintana D, et al. The anatomic substrates for outflow tract arrhythmias. Heart Rhythm. 2019;16:290–7.
Lerman BB, Stein K, Markowitz SM. Mechanisms of idiopathic left ventricular tachycardia. J Cardiovasc Electrophysiol. 1997;8:571–83.
Li YG, Gronefeld G, Israel C, Hohnloser SH. Sustained monomorphic ventricular tachycardia ablation from the aortic sinus of Valsalva. J Cardiovasc Electrophysiol. 2002;13:130–4.
Josephson ME, Anter E. Substrate mapping for ventricular tachycardia: assumptions and misconceptions. J Am Coll Cardiol EP. 2015;1:341–52.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the institutional review board.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 3572 KB) Video 1: suspected micro-reentrant circuit in the area of the right-left coronary cusp commissure
Rights and permissions
About this article
Cite this article
Matto, F., Venugopal, D., Bhave, P.D. et al. Utility of high resolution mapping to guide ablation of ventricular arrhythmias from the aortic sinuses of Valsalva. J Interv Card Electrophysiol 66, 51–59 (2023). https://doi.org/10.1007/s10840-021-01040-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-01040-9