Abstract
Purpose
A significant proportion of patients undergoing catheter ablation for atrial fibrillation (AF) experience arrhythmia recurrence. This is mostly due to pulmonary vein reconnection (PVR). Whether mapping using High-Density Wave (HDW) technology is superior to standard bipolar (SB) configuration at detecting PVR is unknown. We aimed to evaluate the efficacy of HDW technology compared to SB mapping in identifying PVR.
Methods
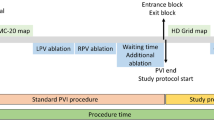
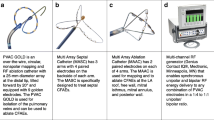
High-Density (HD) multipolar Grid catheters were used to create left atrial geometries and voltage maps in 36 patients undergoing catheter ablation for AF (either due to recurrence of an atrial arrhythmia from previous AF ablation or de novo AF ablation). Nineteen SB maps were also created and compared. Ablation was performed until pulmonary vein isolation was achieved.
Results
Median time of mapping with HDW was 22.3 [IQR: 8.2] min. The number of points collected with HDW (13299.6±1362.8 vs 6952.8±841.9, p<0.001) and used (2337.3±158.0 vs 1727.5±163.8, p<0.001) was significantly higher compared to SB. Moreover, HDW was able to identify more sleeves (16 for right and 8 for left veins), where these were confirmed electrically silent by SB, with significantly increased PVR sleeve size as identified by HDW (p<0.001 for both right and left veins). Importantly, with the use of HDW, the ablation strategy changed in 23 patients (64% of targeted veins) with a significantly increased number of lesions required as compared to SB for right (p=0.005) and left veins (p=0.003).
Conclusion
HDW technology is superior to SB in detecting pulmonary vein reconnections. This could potentially result into a significant change in ablation strategy and possibly to increased success rate following pulmonary vein isolation.




Similar content being viewed by others
References
Nery PB, Belliveau D, Nair GM, Bernick J, Redpath CJ, Szczotka A, et al. Relationship Between Pulmonary Vein Reconnection and Atrial Fibrillation Recurrence: A Systematic Review and Meta-Analysis. JACC Clin Electrophysiol. 2016;2:474–83.
Morillo CA, Verma A, Connolly SJ, Kuck KH, Nair GM, Champagne J, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): a randomized trial. JAMA. 2014;311:692–700.
Lin D, Santangeli P, Zado ES, et al. Electrophysiologic findings and long-term outcomes in patients undergoing third or more catheter ablation procedures for atrial fibrillation. J Cardiovasc Electrophysiol. 2015;26:371–7.
Kuck KH, Hoffmann BA, Ernst S, et al. Impact of Complete Versus Incomplete Circumferential Lines Around the Pulmonary Veins During Catheter Ablation of Paroxysmal Atrial Fibrillation: Results From the Gap-Atrial Fibrillation-German Atrial Fibrillation Competence Network 1 Trial. Circ Arrhythm Electrophysiol. 2016;9:e003337.
Nanthakumar K, Plumb VJ, Epstein AE, Veenhuyzen GD, Link D, Kay GN. Resumption of electrical conduction in previously isolated pulmonary veins: rationale for a different strategy? Circulation. 2004;109:1226–9.
Hussein A, Das M, Riva S, et al. Use of Ablation Index-Guided Ablation Results in High Rates of Durable Pulmonary Vein Isolation and Freedom From Arrhythmia in Persistent Atrial Fibrillation Patients. Circ Arrhythm Electrophysiol. 2018;11:e006576.
Hutchinson MD, Garcia FC, Mandel JE, Elkassabany N, Zado ES, Riley MP, et al. Efforts to enhance catheter stability improve atrial fibrillation ablation outcome. Heart Rhythm. 2013;10:347–53.
Park CI, Lehrmann H, Keyl C, et al. Mechanisms of pulmonary vein reconnection after radiofrequency ablation of atrial fibrillation: the deterministic role of contact force and interlesion distance. J Cardiovasc Electrophysiol. 2014;25:701–8.
Piorkowski C, Eitel C, Rolf S, Bode K, Sommer P, Gaspar T, et al. Steerable versus non steerable sheath technology in atrial fibrillation ablation: a prospective, randomized study. Circ Arrhythm Electrophysiol. 2011;4:157–65.
Chen S, Meng W, Sheng He D, et al. Blocking the pulmonary vein to left atrium conduction in addition to the entrance block enhances clinical efficacy in atrial fibrillation ablation. Pacing Clin Electrophysiol. 2012;35:524–31.
Anter E, Contreras-Valdes FM, Shvilkin A, Tschabrunn CM, Josephson ME. Acute pulmonary vein reconnection is a predictor of atrial fibrillation recurrence following pulmonary vein isolation. J Interv Card Electrophysiol. 2014;39:225–32.
Porta-Sánchez A, Magtibay K, Nayyar S, Bhaskaran A, Lai PFH, Massé S, et al. Omnipolarity applied to equi-spaced electrode array for ventricular tachycardia substrate mapping. Europace. 2019;21:813–21.
Kanamori N, Kato T, Sakagami S, Saeki T, Kato C, Kawai K, et al. Optimal lesion size index to prevent conduction gap during pulmonary vein isolation. J Cardiovasc Electrophysiol. 2018;29:1616–23.
Whitaker J, Fish J, Harrison J, et al. Lesion Index-Guided Ablation Facilitates Continuous, Transmural, and Durable Lesions in a Porcine Recovery Model. Circ Arrhythm Electrophysiol. 2018;11:e005892.
Mattia L, Crosato M, Indiani S, Causin E, Licciardello C, Maria Squasi PA, et al. Prospective Evaluation of Lesion Index-Guided Pulmonary Vein Isolation Technique in Patients with Paroxysmal Atrial Fibrillation: 1-year Follow-Up. J Atr Fibrillation. 2018;10:1858.
Lin C-Y, Te ALD, Lin Y-J, et al. High-resolution mapping of pulmonary vein potentials improved the successful pulmonary vein isolation using small electrodes and inter-electrode spacing catheter. Int J Cardiol. 2018;272:90–6.
Anter E, Tschabrunn CM, Josephson ME. High-Resolution Mapping of Scar-Related Atrial Arrhythmias Using Smaller Electrodes With Closer Interelectrode Spacing. Circ Arrhythm Electrophysiol. 2015;8:537–45.
Masuda M, Fujita M, Iida O, Okamoto S, Ishihara T, Nanto K, et al. The identification of conduction gaps after pulmonary vein isolation using a new electroanatomic mapping system. Heart Rhythm. 2017;14:1606–14.
Tedrow UB, Stevenson WG. Recording and interpreting unipolar electrograms to guide catheter ablation. Heart Rhythm. 2011;8:791–6.
Iso K, Watanabe I, Kogawa R, Okumura Y, Nagashima K, Takahashi K, et al. Wavefront direction and cycle length affect left atrial electrogram amplitude. J Arrhythm. 2017;33:269–74.
Garcia-Bolao I, Ballesteros G, Ramos B, et al. Identification of pulmonary vein reconnection gaps with high-density mapping in redo atrial fibrillation procedures. Europace. 2018;20:f351–8.
McGarry TJ, Narayan SM. The Anatomical Basis of Pulmonary Vein Reconnection After Ablation for Atrial Fibrillation: Wounds That Never Felt a Scar? J Am Coll Cardiol. 2012;59:939–41.
Kowalski M, Grimes MM, Perez FJ, Kenigsberg DN, Koneru J, Kasirajan V, et al. Histopathologic Characterization of Chronic Radiofrequency Ablation Lesions for Pulmonary Vein Isolation. J Am Coll Cardiol. 2012;59:930–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr Chow receives research grant funding from Abbott and Boston Scientific Inc.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Figure S1.
(DOCX 1714 kb)
Rights and permissions
About this article
Cite this article
Papageorgiou, N., Karim, N., Williams, J. et al. Initial experience of the High-Density Grid catheter in patients undergoing catheter ablation for atrial fibrillation. J Interv Card Electrophysiol 63, 259–266 (2022). https://doi.org/10.1007/s10840-021-00950-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-00950-y