Abstract
Purpose
Left ventricular (LV) lead complications in cardiac resynchronization therapy are challenging and poorly reported. We aimed to establish prevalence, causes and outcomes of LV lead complications requiring re-intervention.
Methods
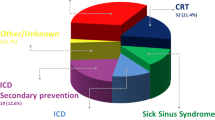
We analysed the rate of complications in 2551 consecutive patients who received a transvenous de novo LV lead as part of a cardiac resynchronization therapy device between 2000 and 2018. LV lead complications requiring re-intervention were identified; those due to infection were excluded. Patient, procedural and device characteristics, and outcomes were examined for non-infective LV lead complications requiring re-intervention.
Results
During a median of 4.7 years, 142 (5.6%) patients required re-intervention for non-infective LV lead complications with a decrease from 10.7% between 2000 and 2004, 8.7% between 2005 and 2009, 3.2% between 2010 and 2014 to 3.2% after 2014. The most common complications were LV lead displacement (50%), high pacing threshold (28%) and phrenic nerve stimulation (15%). Of the complications, 79 (56%) occurred within 90 days post-implant and 63 (44%) later. At the end of the study period, 132/142 patients (93%) had a functional LV lead. Lead re-intervention was associated with higher risk of complications (20%), but no increase in mortality (P = 0.19). Quadripolar leads had longer longevity and lower risk of complications compared with unipolar and bipolar LV leads.
Conclusions
A small but significant proportion of patients required LV lead re-intervention for complications following de novo implant. Lead displacement accounted for half of the re-interventions. Re-intervention was associated with a higher complication rate, but 92% of these patients had functional LV leads at the end of follow-up.



Similar content being viewed by others
References
Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J. 2013;34(29):2281–329. https://doi.org/10.1093/eurheartj/eht150.
Leon AR, Abraham WT, Curtis AB, Daubert JP, Fisher WG, Gurley J, et al. Safety of transvenous cardiac resynchronization system implantation in patients with chronic heart failure: combined results of over 2,000 patients from a multicenter study program. J Am Coll Cardiol. 2005;46(12):2348–56. https://doi.org/10.1016/j.jacc.2005.08.031.
Poole JE, Gleva MJ, Mela T, Chung MK, Uslan DZ, Borge R, et al. Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation. 2010;122(16):1553–61. https://doi.org/10.1161/CIRCULATIONAHA.110.976076.
Palmisano P, Accogli M, Zaccaria M, Luzzi G, Nacci F, Anaclerio M, et al. Rate, causes, and impact on patient outcome of implantable device complications requiring surgical revision: large population survey from two centres in Italy. Europace. 2013;15(4):531–40. https://doi.org/10.1093/europace/eus337.
Cheng A, Wang Y, Curtis JP, Varosy PD. Acute lead dislodgements and in-hospital mortality in patients enrolled in the national cardiovascular data registry implantable cardioverter defibrillator registry. J Am Coll Cardiol. 2010;56(20):1651–6. https://doi.org/10.1016/j.jacc.2010.06.037.
van Rees JB, de Bie MK, Thijssen J, Borleffs CJ, Schalij MJ, van Erven L. Implantation-related complications of implantable cardioverter-defibrillators and cardiac resynchronization therapy devices: a systematic review of randomized clinical trials. J Am Coll Cardiol. 2011;58(10):995–1000. https://doi.org/10.1016/j.jacc.2011.06.007.
Turagam MK, Afzal MR, Iskander S, Madhu R, Biase LD, Natale A, et al. A meta-analysis of quadripolar versus bipolar left ventricular leads on post-procedural outcomes. J Atr Fibrillation. 2016;9(2):1472. https://doi.org/10.4022/jafib.1472.
Kirkfeldt RE, Johansen JB, Nohr EA, Jorgensen OD, Nielsen JC. Complications after cardiac implantable electronic device implantations: an analysis of a complete, nationwide cohort in Denmark. Eur Heart J. 2014;35(18):1186–94. https://doi.org/10.1093/eurheartj/eht511.
Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–90. https://doi.org/10.2147/CLEP.S91125.
Pedersen CB, Gotzsche H, Moller JO, Mortensen PB. The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull. 2006;53(4):441–9.
Mortensen PT, Herre JM, Chung ES, Bax JJ, Gerritse B, Kruijshoop M, et al. The effect of left ventricular pacing site on cardiac resynchronization therapy outcome and mortality: the results of a PROSPECT substudy. Europace. 2010;12(12):1750–6. https://doi.org/10.1093/europace/euq324.
Kutyifa V, Kosztin A, Klein HU, Biton Y, Nagy VK, Solomon SD, et al. Left ventricular lead location and long-term outcomes in cardiac resynchronization therapy patients. JACC Clin Electrophysiol. 2018;4(11):1410–20. https://doi.org/10.1016/j.jacep.2018.07.006.
Behon A, Schwertner WR, Merkel ED, Kovács A, Lakatos BK, Zima E, et al. Lateral left ventricular lead position is superior to posterior position in long-term outcome of patients who underwent cardiac resynchronization therapy. ESC Heart Fail. 2020;7:3374–82. https://doi.org/10.1002/ehf2.13066.
Gras D, Bocker D, Lunati M, Wellens HJ, Calvert M, Freemantle N, et al. Implantation of cardiac resynchronization therapy systems in the CARE-HF trial: procedural success rate and safety. Europace. 2007;9(7):516–22. https://doi.org/10.1093/europace/eum080.
Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009;361(14):1329–38. https://doi.org/10.1056/NEJMoa0906431.
Nof E, Gurevitz O, Carraso S, Bar-Lev D, Luria D, Bachar S, et al. Comparison of results with different left ventricular pacing leads. Europace. 2008;10(1):35–9. https://doi.org/10.1093/europace/eum241.
Ahsan SY, Saberwal B, Lambiase PD, Chaubey S, Segal OR, Gopalamurugan AB, et al. An 8-year single-centre experience of cardiac resynchronisation therapy: procedural success, early and late complications, and left ventricular lead performance. Europace. 2013;15(5):711–7. https://doi.org/10.1093/europace/eus401.
Chapman M, Bates MGD, Behar JM, Williams I, Dewhurst M, Monkhouse C, et al. A novel quadripolar active fixation left-ventricular pacing lead for cardiac resynchronization therapy: initial United Kingdom experience. JACC Clin Electrophysiol. 2019;5(9):1028–35. https://doi.org/10.1016/j.jacep.2019.05.005.
Duray GZ, Israel CW, Pajitnev D, Hohnloser SH. Upgrading to biventricular pacing/defibrillation systems in right ventricular paced congestive heart failure patients: prospective assessment of procedural parameters and response rate. Europace. 2008;10(1):48–52. https://doi.org/10.1093/europace/eum259.
Lecoq G, Leclercq C, Leray E, Crocq C, Alonso C, de Place C, et al. Clinical and electrocardiographic predictors of a positive response to cardiac resynchronization therapy in advanced heart failure. Eur Heart J. 2005;26(11):1094–100. https://doi.org/10.1093/eurheartj/ehi146.
van Bommel RJ, Ypenburg C, Mollema SA, Borleffs CJ, Delgado V, Bertini M, et al. Site of latest activation in patients eligible for cardiac resynchronization therapy: patterns of dyssynchrony among different QRS configurations and impact of heart failure etiology. Am Heart J. 2011;161(6):1060–6. https://doi.org/10.1016/j.ahj.2011.03.014.
Sommer A, Kronborg MB, Norgaard BL, Poulsen SH, Bouchelouche K, Bottcher M, et al. Multimodality imaging-guided left ventricular lead placement in cardiac resynchronization therapy: a randomized controlled trial. Eur J Heart Fail. 2016;18(11):1365–74. https://doi.org/10.1002/ejhf.530.
Kronborg MB, Johansen JB, Riahi S, Petersen HH, Haarbo J, Jorgensen OD, et al. An anterior left ventricular lead position is associated with increased mortality and non-response in cardiac resynchronization therapy. Int J Cardiol. 2016;222:157–62. https://doi.org/10.1016/j.ijcard.2016.07.235.
Dickstein K, Bogale N, Priori S, Auricchio A, Cleland JG, Gitt A, et al. The European cardiac resynchronization therapy survey. Eur Heart J. 2009;30(20):2450–60. https://doi.org/10.1093/eurheartj/ehp359.
Buiten MS, van der Heijden AC, Klautz RJ, Schalij MJ, van Erven L. Epicardial leads in adult cardiac resynchronization therapy recipients: a study on lead performance, durability, and safety. Heart Rhythm. 2015;12(3):533–9. https://doi.org/10.1016/j.hrthm.2014.11.004.
Rademakers LM, van Gelder BM, Scheffer MG, Bracke FA. Mid-term follow up of thromboembolic complications in left ventricular endocardial cardiac resynchronization therapy. Heart Rhythm. 2014;11(4):609–13. https://doi.org/10.1016/j.hrthm.2014.01.031.
Rickard J, Johnston DR, Price J, Tedford R, Baranowski B, Bassiouny M, et al. Reverse ventricular remodeling and long-term survival in patients undergoing cardiac resynchronization with surgically versus percutaneously placed left ventricular pacing leads. Heart Rhythm. 2015;12(3):517–23. https://doi.org/10.1016/j.hrthm.2014.11.013.
Giraldi F, Cattadori G, Roberto M, Carbucicchio C, Pepi M, Ballerini G, et al. Long-term effectiveness of cardiac resynchronization therapy in heart failure patients with unfavorable cardiac veins anatomy comparison of surgical versus hemodynamic procedure. J Am Coll Cardiol. 2011;58(5):483–90. https://doi.org/10.1016/j.jacc.2011.02.065.
Funding
This work was supported by the Danish Council for Independent Research (grant number 12-127221), the Central Denmark Region Research Foundation and Fabrikant Karl G. Andersens Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study was approved by the Danish Health and Medicines Authority and the Danish Data Protection Agency.
Conflict of interest
Jens Cosedis Nielsen is supported by the Novo Nordisk Foundation (NNF16OC0018658). The other authors report no relationships that could be construed as a conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Witt, C.T., Ng Kam Chuen, M.J., Kronborg, M.B. et al. Non-infective left ventricular lead complications requiring re-intervention following cardiac resynchronization therapy: prevalence, causes and outcomes. J Interv Card Electrophysiol 63, 69–75 (2022). https://doi.org/10.1007/s10840-021-00947-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-00947-7