Abstract
Purpose
Ablation of atypical atrial flutter (AAFL) can be challenging. High-density (HD) mapping of ablation targets may potentially increase procedural success and freedom from recurrent AAFL. The objective of the present study was to explore whether employing HD mapping leads to a more favorable outcome in ablation of AAFL.
Methods
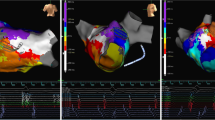
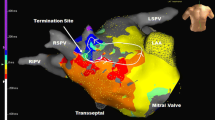
We compared baseline and procedural characteristics, procedural success, safety and outcome of mapping and ablation of atypical flutter in three groups. (1) HD Grid catheter + the high-density electroanatomical mapping (EAM) system EnSite Precision; (2) standard 10-pole circular mapping catheter (CMC) + EnSite Precision; (3) CMC + the low-density EnSite Velocity EAM. Voltage and propagation maps were constructed.
Results
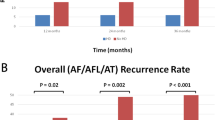
Mapping of 142 AAFL in 82 patients was performed. Acute ablation success was 78%, 68%, and 51% in groups 1, 2, and 3 (p = 0.037 between group 1 and 3, non-significant between groups otherwise). Moreover, 8%, 27%, and 36% of flutters were unmappable in groups 1, 2, and 3, respectively (p < 0.05 between group 1 and both groups 2 and 3). AAFL recurrence at 1-year FU was 26%, 36%, and 62% in groups 1, 2, and 3 (p = 0.007 between groups 1 and 3, p = 0.05 between groups 2 and 3). AAFL-free survival was significantly higher in patients mapped with Precision than with Velocity (p = 0.011). No strokes or mortality occurred within 30 days.
Conclusions
Acute procedural success of ablation of atypical atrial flutter is higher and the number of unmappable flutters is lower using the HD Grid mapping catheter in combination with the high-density EnSite Precision system, as compared to a decapolar circular mapping catheter and the low-density EnSite Velocity EAM system. This may lead to increased freedom from recurrent AAFL at 1 year. HD mapping is safe.




Similar content being viewed by others
Data Availability
All data are available on request.
References
Knecht S, Veenhuyzen G, O’Neill MD, Wright M, Nault I, Weerasooriya R, et al. Atrial tachycardias encountered in the context of catheter ablation for atrial fibrillation part II: mapping and ablation. Pacing Clin Electrophysiol. 2009;32(4):528–38. https://doi.org/10.1111/j.1540-8159.2009.02315.x.
Calkins H, Hindricks G, Cappato R, Kim Y-H, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation: executive summary. J Arrhythm. 2017;33(5):369–409. https://doi.org/10.1016/j.joa.2017.08.001.
Chae S, Oral H, Good E, Dey S, Wimmer A, Crawford T, et al. Atrial tachycardia after circumferential pulmonary vein ablation of atrial fibrillation. J Am Coll Cardiol. 2007;50(18):1781–7. https://doi.org/10.1016/j.jacc.2007.07.044.
Sawhney N, Anousheh R, Chen W, Feld GK. Circumferential pulmonary vein ablation with additional linear ablation results in an increased incidence of left atrial flutter compared with segmental pulmonary vein isolation as an initial approach to ablation of paroxysmal atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(3):243–8. https://doi.org/10.1161/CIRCEP.109.924878.
Wasmer K, Mönnig G, Bittner A, Dechering D, Zellerhoff S, Milberg P, et al. Incidence, characteristics, and outcome of left atrial tachycardias after circumferential antral ablation of atrial fibrillation. Heart Rhythm. 2012;9(10):1660–6. https://doi.org/10.1016/j.hrthm.2012.06.007.
Matsuo S, Wright M, Knecht S, Nault I, Lellouche N, Lim K-T, et al. Peri-mitral atrial flutter in patients with atrial fibrillation ablation. Heart Rhythm. 2010;7(1):2–8. https://doi.org/10.1016/j.hrthm.2009.09.067.
van Laar C, Bentala M, Weimar T, Doll N, Swaans MJ, Molhoek SG, et al. Thoracoscopic ablation for the treatment of atrial fibrillation: a systematic outcome analysis of a multicentre cohort. EP Europace. 2019;21(6):893–9. https://doi.org/10.1093/europace/euy323.
McElderry HT, McGiffin DC, Plumb VJ, Nanthakumar K, Epstein AE, Yamada T, et al. Proarrhythmic aspects of atrial fibrillation surgery: mechanisms of postoperative macroreentrant tachycardias. Circulation. 2008;117(2):155–62. https://doi.org/10.1161/CIRCULATIONAHA.107.688358.
Cosío FG. Atrial flutter, typical and atypical: a review. Arrhythmia Electrophysiol Rev. 2017;6(2):55. https://doi.org/10.15420/aer.2017.5.2.
Daoud EG, Weiss R, Augostini R, Hummel JD, Kalbfleisch SJ, Van Deren JM, et al. Proarrhythmia of circumferential left atrial lesions for management of atrial fibrillation. J Cardiovasc Electrophysiol. 2006;17(2):157–65. https://doi.org/10.1111/j.1540-8167.2006.00312.x.
Page RL, Joglar JA, Caldwell MA, Calkins H, Conti JB, Deal BJ, et al. 2015 ACC/AHA/HRS guideline for the management of adult patients with supraventricular tachycardia. J Am Coll Cardiol. 2016;67(13):e27–e115. https://doi.org/10.1016/j.jacc.2015.08.856.
Marrouche NF, Natale A, Wazni OM, Cheng J, Yang Y, Pollack H, et al. Left septal atrial flutter. Circulation. 2004;109(20):2440–7. https://doi.org/10.1161/01.CIR.0000129439.03836.96.
Aktas MK, Khan MN, Di Biase L, Elayi C, Martin D, Saliba W, et al. Higher rate of recurrent atrial flutter and atrial fibrillation following atrial flutter ablation after cardiac surgery. J Cardiovasc Electrophysiol. 2010. https://doi.org/10.1111/j.1540-8167.2009.01709.x.
Vlachos K, Denis A, Takigawa M, Kitamura T, Martin CA, Frontera A, et al. The role of Marshall bundle epicardial connections in atrial tachycardias after atrial fibrillation ablation. Heart Rhythm. 2019;16(9):1341–7. https://doi.org/10.1016/j.hrthm.2019.05.019.
Takigawa M, Derval N, Frontera A, Martin R, Yamashita S, Cheniti G, et al. Revisiting anatomic macroreentrant tachycardia after atrial fibrillation ablation using ultrahigh-resolution mapping: implications for ablation. Heart Rhythm. 2018;15(3):326–33. https://doi.org/10.1016/j.hrthm.2017.10.029.
Anter E, Tschabrunn CM, Josephson ME. High-resolution mapping of scar-related atrial arrhythmias using smaller electrodes with closer interelectrode spacing. Circ Arrhythm Electrophysiol. 2015;8(3):537–45. https://doi.org/10.1161/CIRCEP.114.002737.
Frontera A, Takigawa M, Martin R, Thompson N, Cheniti G, Massoullié G, et al. Electrogram signature of specific activation patterns: analysis of atrial tachycardias at high-density endocardial mapping. Heart Rhythm. 2018;15(1):28–37. https://doi.org/10.1016/j.hrthm.2017.08.001.
Bun S-S, Delassi T, Latcu DG, El Jamili M, Ayari A, Errahmouni A, et al. A comparison between multipolar mapping and conventional mapping of atrial tachycardias in the context of atrial fibrillation ablation. Arch Cardiovasc Dis. 2018;111(1):33–40. https://doi.org/10.1016/j.acvd.2017.04.005.
Kapa S, Desjardins B, Callans DJ, Marchlinski FE, Dixit S. Contact electroanatomic mapping derived voltage criteria for characterizing left atrial scar in patients undergoing ablation for atrial fibrillation. J Cardiovasc Electrophysiol. 2014;25(10):1044–52. https://doi.org/10.1111/jce.12452.
Rolf S, Kircher S, Arya A, Eitel C, Sommer P, Richter S, et al. Tailored atrial substrate modification based on low-voltage areas in catheter ablation of atrial fibrillation. Circ Arrhythm Electrophysiol. 2014;7(5):825–33. https://doi.org/10.1161/CIRCEP.113.001251.
Jadidi AS, Cochet H, Shah AJ, Kim SJ, Duncan E, Miyazaki S, et al. Inverse relationship between fractionated electrograms and atrial fibrosis in persistent atrial fibrillation: combined magnetic resonance imaging and high-density mapping. J Am Coll Cardiol. 2013;62(9):802–12. https://doi.org/10.1016/j.jacc.2013.03.081.
Miyazaki S, Shah AJ, Hocini M, Haïssaguerre M, Jaïs P. Recurrent spontaneous clinical perimitral atrial tachycardia in the context of atrial fibrillation ablation. Heart Rhythm. 2015;12(1):104–10. https://doi.org/10.1016/j.hrthm.2014.09.055.
Deisenhofer I, Estner H, Zrenner B, Schreieck J, Weyerbrock S, Hessling G, et al. Left atrial tachycardia after circumferential pulmonary vein ablation for atrial fibrillation: incidence, electrophysiological characteristics, and results of radiofrequency ablation. EP Europace. 2006;8(8):573–82. https://doi.org/10.1093/europace/eul077.
Coffey JO, d’Avila A, Dukkipati S, Danik SB, Gangireddy SR, Koruth JS, et al. Catheter ablation of scar-related atypical atrial flutter. EP Europace. 2013;15(3):414–9. https://doi.org/10.1093/europace/eus312.
Jaïs P, Shah DC, Haïssaguerre M, Hocini M, Peng JT, Takahashi A, et al. Mapping and ablation of left atrial flutters. Circulation. 2000;101(25):2928–34. https://doi.org/10.1161/01.cir.101.25.2928.
Tan VH, Lyu MZ, Tan PC, Wong LC, Yeo C, Wong KCK. Utility of directional high-density mapping catheter (AdvisorTM HD Grid) in complex scar-related atrial tachycardia. J Arrhythm. 2020;36(1):180–3. https://doi.org/10.1002/joa3.12256.
Kumagai K. Editorial to utility of directional high-density mapping catheter (Advisor HD Grid) in complex scar-related atrial tachycardia. J Arrhythm. 2020;36(1):184–5. https://doi.org/10.1002/joa3.12272.
Ouyang F, Ernst S, Vogtmann T, Goya M, Volkmer M, Schaumann A, et al. Characterization of reentrant circuits in left atrial macroreentrant tachycardia. Circulation. 2002;105(16):1934–42. https://doi.org/10.1161/01.CIR.0000015077.12680.2E.
Masuda M, Asai M, Iida O, Okamoto S, Ishihara T, Nanto K, et al. Left atrial voltage mapping with a direction-independent grid catheter: comparison with a conventional circular mapping catheter. J Cardiovasc Electrophysiol. 2019;30(12):2834–40. https://doi.org/10.1111/jce.14263.
Chugh A, Gurm HS, Krishnasamy K, Saeed M, Lohawijarn W, Hornsby K, et al. Spectrum of atrial arrhythmias using the ligament of Marshall in patients with atrial fibrillation. Heart Rhythm. 2018;15(1):17–24. https://doi.org/10.1016/j.hrthm.2017.07.033.
Chen S, Lu X, Liu S. Elaborating endocardial mapping the Marshall bundle revealed a perimitral flutter mediated by ligament of Marshall. Europace. 2020;22(2):258. https://doi.org/10.1093/europace/euz240.
Reddy VY, Dukkipati SR, Neuzil P, Natale A, Albenque J-P, Kautzner J, et al. Randomized, controlled trial of the safety and effectiveness of a contact force-sensing irrigated catheter for ablation of paroxysmal atrial fibrillation: results of the TactiCath Contact Force Ablation Catheter Study for Atrial Fibrillation (TOCCASTAR) Study. Circulation. 2015;132(10):907–15. https://doi.org/10.1161/CIRCULATIONAHA.114.014092.
Ullah W, McLean A, Tayebjee MH, Gupta D, Ginks MR, Haywood GA, et al. Randomized trial comparing pulmonary vein isolation using the SmartTouch catheter with or without real-time contact force data. Heart Rhythm. 2016;13(9):1761–7. https://doi.org/10.1016/j.hrthm.2016.05.011.
Kimura M, Sasaki S, Owada S, Horiuchi D, Sasaki K, Itoh T, et al. Comparison of lesion formation between contact force-guided and non-guided circumferential pulmonary vein isolation: a prospective, randomized study. Heart Rhythm. 2014;11(6):984–91. https://doi.org/10.1016/j.hrthm.2014.03.019.
Fichtner S, Wakili R, Rizas K, Siebermair J, Sinner MF, Wiktor T, et al. Benefit of contact force sensing catheter technology for successful left atrial anterior line formation: a prospective randomized trial. Biomed Res Int. 2018;2018:9784259–8. https://doi.org/10.1155/2018/9784259.
Conti S, Weerasooriya R, Novak P, Champagne J, Lim HE, Macle L, et al. Contact force sensing for ablation of persistent atrial fibrillation: a randomized, multicenter trial. Heart Rhythm. 2018;15(2):201–8. https://doi.org/10.1016/j.hrthm.2017.10.010.
Winkle R, Moskovitz R, Mead R, Engel G, Kong M, Fleming W, et al. Ablation of atypical atrial flutters using ultra high density-activation sequence mapping. J Interv Card Electrophysiol. 2017;48(2):177–84. https://doi.org/10.1007/S10840-016-0207-5.
Asferg C, Chen C, Pehrson S, Jacobsen P. Catheter ablation of atypical flutter using new 3-dimensional electroanatomic mapping software focusing on areas of conduction block. HeartRhythm Case Rep. 2019;5(4):225–8. https://doi.org/10.1016/J.HRCR.2019.01.003.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.B. reports a consulting fee of 1120 Euro from Abbott to the R&D Department. M.K., B.M., V.v.D., M.W., and L.B. have nothing to declare.
Disclaimer
Abbott was not in any way involved in the design, conduction, analysis, or publication of this registry.
Ethics approval
The study was conducted in compliance with Good Clinical Practice Guidelines and was approved by the Ethics Committee and local institutional review board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Balt, J.C., Klaver, M.N., Mahmoodi, B.K. et al. High-density versus low-density mapping in ablation of atypical atrial flutter. J Interv Card Electrophysiol 62, 587–599 (2021). https://doi.org/10.1007/s10840-021-00939-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-021-00939-7