Abstract
Background
Although outflow tract (OT) ventricular arrhythmias (VAs) are generally regarded as benign, the relationship between circulation pressure and VAs has received considerable attention in recent years. Previous studies have shown that the ratio of main pulmonary artery (MPA) to ascending aorta (AA) diameter is associated with pulmonary pressure. Here, we investigated whether an elevated MPA/AA ratio is associated with right ventricular OT (RVOT) VAs.
Methods
A total of 67 patients with OT VAs (47 patients with RVOT and 20 patients with LVOT) who underwent cardiac multidetector computed tomography and radiofrequency ablation were enrolled in this study. MPA and AA diameters were measured at the level of the bifurcation of the pulmonary artery. According to the MPA/AA ratio, patients were further divided into two groups: the MPA/AA ratio abnormal group (n = 19), which is defined as MPA/AA ratio ≥ 0.9, and the MPA/AA ratio normal group (n = 48) consisting of patients with an MPA/AA ratio < 0.9.
Results
Patients with RVOT VAs exhibited an elevated MPA/AA ratio (0.84 ± 0.11 vs. 0.75 ± 0.11, p = 0.006). Furthermore, this MPA/AA ratio was shown to be an independent predictor for RVOT VAs (p = 0.013, 95% confidence interval: 1.016–1.145), with an abnormal MPA/AA ratio increasing the odds of RVOT VAs 5.1-fold in patients with OT VAs.
Conclusion
Patients with RVOT VAs exhibited significantly higher MPA/AA ratios compared with those LVOT VAs. The MPA/AA ratio was showed to be an independent predictor RVOT VAs.

Similar content being viewed by others
References
Bandorski D, Erkapic D, Stempfl J, Höltgen R, Grünig E, Schmitt J, et al. Ventricular tachycardias in patients with pulmonary hypertension: an underestimated prevalence? A prospective clinical study. Herzschrittmacherther Elektrophysiol. 2015;26:155–62.
Cronin EM, Bogun FM, Maury P, Peichl P, Chen M, Namboodiri N, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2019;21:1143–4.
Cuttica MJ, Bhatt SP, Rosenberg SR, Beussink L, Shah SJ, Smith LJ, et al. Pulmonary artery to aorta ratio is associated with cardiac structure and functional changes in mild-to-moderate COPD. Int J Chronic Obstructive Pulm Disease. 2017;12:1439–46.
Deroubaix E, Folliguet T, Rücker-Martin C, Dinanian S, Boixel C, Validire P, et al. Moderate and chronic hemodynamic overload of sheep atria induces reversible cellular electrophysiologic abnormalities and atrial vulnerability. J Am Coll Cardiol. 2004;44:1918–26.
Gami AS, Noheria A, Lachman N, Edwards WD, Friedman PA, Talreja D, et al. Anatomical correlates relevant to ablation above the semilunar valves for the cardiac electrophysiologist: a study of 603 hearts. J Interv Cardiac Electrophysiol: an international journal of arrhythmias and pacing. 2011;30:5–15.
Iyer AS, Wells JM, Vishin S, Bhatt SP, Wille KM, Dransfield MT. CT scan-measured pulmonary artery to aorta ratio and echocardiography for detecting pulmonary hypertension in severe COPD. Chest. 2014;145:824–32.
Korshunov V, Penela D, Linhart M, Acosta J, Martinez M, Soto-Iglesias D, et al. Prediction of premature ventricular complex origin in left vs. right ventricular outflow tract: a novel anatomical imaging approach. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2019;21:147–53.
Kovacs G, Avian A, Tscherner M, Foris V, Bachmaier G, Olschewski A, et al. Characterization of patients with borderline pulmonary arterial pressure. Chest. 2014;146:1486–93.
Lange TJ, Dornia C, Stiefel J, et al. Increased pulmonary artery diameter on chest computed tomography can predict borderline pulmonary hypertension. Pulmonary Circulation. 2013;3:363–8.
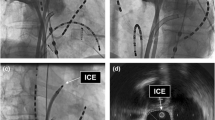
Liu CF, Cheung JW, Thomas G, Ip JE, Markowitz SM, Lerman BB. Ubiquitous myocardial extensions into the pulmonary artery demonstrated by integrated intracardiac echocardiography and electroanatomic mapping: changing the paradigm of idiopathic right ventricular outflow tract arrhythmias. Circ Arrhythm Electrophysiol. 2014;7:691–700.
Markowitz SM, Weinsaft JW, Waldman L, et al. Reappraisal of cardiac magnetic resonance imaging in idiopathic outflow tract arrhythmias. J Cardiovasc Electrophysiol. 2014;25:1328–35.
Maron BA, Hess E, Maddox TM, Opotowsky AR, Tedford RJ, Lahm T, et al. Association of borderline pulmonary hypertension with mortality and hospitalization in a large patient cohort: insights from the veterans affairs clinical assessment, reporting, and tracking program. Circulation. 2016;133:1240–8.
Nucifora G, Muser D, Masci PG, Barison A, Rebellato L, Piccoli G, et al. Prevalence and prognostic value of concealed structural abnormalities in patients with apparently idiopathic ventricular arrhythmias of left versus right ventricular origin: a magnetic resonance imaging study. Circ Arrhythm Electrophysiol. 2014;7:456–62.
Penela D, De Riva M, Herczku C, et al. An easy-to-use, operator-independent, clinical model to predict the left vs. right ventricular outflow tract origin of ventricular arrhythmias. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2015;17:1122–8.
Shin SY, Jo WM, Min TJ, Kim BK, Song DH, Hyeon SH, et al. Gap junction remodelling by chronic pressure overload is related to the increased susceptibility to atrial fibrillation in rat heart. Europace: European pacing, arrhythmias, and cardiac electrophysiology: journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology. 2015;17:655–63.
Simpson RJ Jr, Cascio WE, Schreiner PJ, Crow RS, Rautaharju PM, Heiss G. Prevalence of premature ventricular contractions in a population of African American and white men and women: the atherosclerosis risk in communities (ARIC) study. Am Heart J. 2002;143:535–40.
Tandri H, Bluemke DA, Ferrari VA, Bomma C, Nasir K, Rutberg J, et al. Findings on magnetic resonance imaging of idiopathic right ventricular outflow tachycardia. Am J Cardiol. 2004;94:1441–5.
Truong QA, Massaro JM, Rogers IS, Mahabadi AA, Kriegel MF, Fox CS, et al. Reference values for normal pulmonary artery dimensions by noncontrast cardiac computed tomography: the Framingham heart study. Circ Cardiovasc Imaging. 2012;5:147–54.
Zeltser I, Gaynor JW, Petko M, Myung RJ, Birbach M, Waibel R, et al. The roles of chronic pressure and volume overload states in induction of arrhythmias: an animal model of physiologic sequelae after repair of tetralogy of Fallot. J Thorac Cardiovasc Surg. 2005;130:1542–8.
Zhang J, Tang C, Zhang Y, Su X. Pulmonary sinus cusp mapping and ablation: a new concept and approach for idiopathic right ventricular outflow tract arrhythmias. Heart Rhythm. 2018;15:38–45.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The study was approved by the West China Hospital Ethics Committee.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jia, R., Xu, Y., Luo, Y. et al. The ratio of main pulmonary artery to ascending aorta diameter is associated with the right ventricular outflow tract ventriculararrhythmias. J Interv Card Electrophysiol 62, 57–62 (2021). https://doi.org/10.1007/s10840-020-00872-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00872-1