Abstract
Purpose
Cardiac conduction disturbance necessitating pacemaker implantation is common among elderly patients. However, patients often have comorbidities and increased frailty which may result in limited life prognosis and a high rate of procedure-related complications. We evaluated pacemaker implantation in older patients by comparing life prognosis and complication rate in patients aged ≥ and < 85 years.
Methods
We retrospectively enrolled 262 consecutive patients who underwent initial pacemaker implantation for bradycardia (age, 77 ± 10 years old; male, 132 (50%); dual chamber pacemaker, 222 (85%) patients). Acute and long-term outcomes were compared between patients aged ≥ 85 and < 85 years. Primary outcome was a composite of all-cause death and severe procedure-related complications.
Results
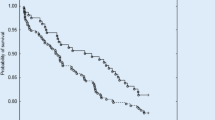
Seven (14%) patients aged ≥ 85 years (n = 50; 19%) were non-ambulatory. During 2-year follow-up, primary outcome (death or severe complication) occurred in 47 (18%). Freedom from primary outcome was similar between age groups (81.6% versus 80.8%; p = 0.98). Freedom from all-cause death and from severe complication in the study period were also similar (all-cause death, 91.6% versus 88.7%, p = 0.70; severe complication, 89.7% versus 91.5%, p = 0.75). On multivariate analysis, sick sinus syndrome (hazard ratio (HR) 2.7, 95% confidence interval (CI) 1.1–6.4, p = 0.03), immunosuppressant use (HR 21 (95% CI 3.3–134), p < 0.01), and high C-reactive protein (HR 1.5 (95% CI 1.2–1.9), p < 0.01) were independent predictors of primary outcome.
Conclusions
Life prognosis and severe complication rates after pacemaker implantation were similar between patients aged ≥ and < 85 years.


Similar content being viewed by others
References
Birnie D, Williams K, Guo A, Mielniczuk L, Davis D, Lemery R, et al. Reasons for escalating pacemaker implants. Am J Cardiol. 2006;98:93–7.
Udo EO, van Hemel NM, Zuithoff NP, Kelder JC, Crommentuijn HA, Koopman-Verhagen AM, et al. Long-term outcome of cardiac pacing in octogenarians and nonagenarians. Europace. 2012;14:502–8.
Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95.
Poole JE, Gleva MJ, Mela T, Chung MK, Uslan DZ, Borge R, et al. REPLACE registry investigators complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE registry. Circulation. 2010;122:1553–61.
Connolly SJ, Kerr CR, Gent M, Roberts RS, Yusuf S, Gillis AM, et al. Effects of physiologic pacing versus ventricular pacing on the risk of stroke and death due to cardiovascular causes. Canadian trial of physiologic pacing investigators. N Engl J Med. 2000;342:1385–91.
Møller M, Arnsbo P, Asklund M, Christensen PD, Gadsbøll N, Svendsen JH, et al. Quality assessment of pacemaker implantations in Denmark. Europace. 2002;4:107–12.
Yamaguchi T, Miyamoto T, Iwai T, Yamaguchi J, Hijikata S, Miyazaki R, et al. Prognosis of super-elderly healthy Japanese patients after pacemaker implantation for bradycardia. J Cardiol. 2017;70:18–22.
Aida J, Cable N, Zaninotto P, Tsuboya T, Tsakos G, Matsuyama Y, et al. Social and behavioural determinants of the difference in survival among older adults in Japan and England. Gerontology. 2018;64:266–77.
Molah Karim SA, Ali Ghalib HH, Mohammed SA, Fattah FHR. The incidence, age at diagnosis of breast cancer in the Iraqi Kurdish population and comparison to some other countries of middle-east and west. Int J Surg. 2015;13:71–5.
Takii T, Yasuda S, Takahashi J, Ito K, Shiba N, Shirato K, et al. MIYAGI-AMI Study Investigators. Trends in acute myocardial infarction incidence and mortality over 30 years in Japan: report from the MIYAGI-AMI registry study. Circ J. 2010;74:93–100.
Mordi IR, Badar AA, Irving RJ, Weir-McCall JR, Houston JG, Lang CC. Efficacy of noninvasive cardiac imaging tests in diagnosis and management of stable coronary artery disease. Vasc Health Risk Manag. 2017;13:427–37.
Benussi S, de Maat GE. Atrial remodelling and function: implications for atrial fibrillation surgery. Eur J Cardiothorac Surg. 2018;53:i2–8.
Tung RT, Shen WK, Hayes DL, Hammill SC, Bailey KR, Gersh BJ. Long-term survival after permanent pacemaker implantation for sick sinus syndrome. Am J Cardiol. 1994;74:1016–20.
Bamoulid J, Staeck O, Halleck F, Khadzhynov D, Brakemeier S, Dürr M, et al. The need for minimization strategies: current problems of immunosuppression. Transpl Int. 2015;28:891–900.
Zhang Z, Ni H. C-reactive protein as a predictor of mortality in critically ill patients: a meta-analysis and systematic review. Anaesth Intensive Care. 2011;39:854–61.
Feng JF, Wang L, Jiang YH, Yang X. C-reactive protein to prealbumin ratio (CPR): a novel inflammatory-nutritional prognostic factor for predicting cancer-specific survival (CSS) and overall survival (OS) in patients with resectable esophageal squamous cell carcinoma. J Oncol. 2019;4359103. https://doi.org/10.1155/2019/4359103.
Kou S, Caballero L, Dulgheru R, Voilliot D, De Sousa C, Kacharava G, et al. Echocardiographic reference ranges for normal cardiac chamber size: results from the NORRE study. Eur Heart J Cardiovasc Imaging. 2014;15:680–90.
Kawata H, Patel J, McGarry T, Joshi R, Krummen D, Feld G, et al. Obese female patients have higher rates of lead dislodgement after ICD or CRT-D implantation. Int J Cardiol. 2014;172:e522–4.
Lin YS, Hung SP, Chen PR, Yang CH, Wo HT, Chang PC, et al. Risk factors influencing complications of cardiac implantable electronic device implantation: infection, pneumothorax and heart perforation: a nationwide population-based cohort study, Medicine (Baltimore). 2014;93:e213.
Yang PS, Jeong J, You SJ, Yu HT, Kim TH, Sung JH, et al. The burden and risk factors for infection of transvenous cardiovascular implantable electronic device: a nationwide cohort study. Korean Circ J. 2019;49:742–52.
Acknowledgments
We thank Guy Harris DO from DMC Corp. (www.dmed.co.jp <http://www.dmed.co.jp/>) for editing drafts of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study complied with the Declaration of Helsinki. Written informed consent for pacemaker implantation and participation in the study was obtained from all patients, and the protocol was approved by our institution’s institutional review board.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Matsuda, Y., Masuda, M., Asai, M. et al. Comparison of prognosis and safety of pacemaker implantation in patients aged less than or 85 years and older. J Interv Card Electrophysiol 61, 171–179 (2021). https://doi.org/10.1007/s10840-020-00797-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00797-9