Abstract
Purpose
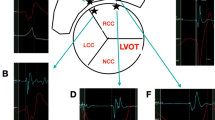
Precise automatic annotation of local activation time (LAT) is crucial for rapid high-density activation mapping in arrhythmia. However, it is still challenging in voltage-transitional areas where local low-amplitude near-field potentials are often obscured by large far-field potentials. The aim of this study was to explore the viability and validity of automatic identification of the earliest activation (EA) in idiopathic right ventricular outflow tract ventricular arrhythmias (RVOT VAs) using a novel Lumipoint algorithm.
Methods and results
Twenty-seven patients with RVOT VAs were mapped with Rhythmia mapping system. Lumipoint algorithms were applied to reannotate the initial activation regions retrospectively. The results showed that LATs were reannotated in 35.0 ± 11.4% points in the initial activation area from bipolar activation breakout time (BBO) to the its 40 ms earlier timepoint. The automatically determined bipolar earliest activation time after Lumipoint reannotation (BEAT-lu: − 111.26 ± 12.13 ms) was significantly earlier than that before (BEAT: − 108.67 ± 12.25 ms, P = 0.000). Compared with manually corrected earliest activation time (EAT), the difference between EAT and BEAT-lu (DEAT-BEAT-lu: 6 (2–7) ms) was significantly smaller than that between EAT and BEAT (DEAT-BEAT/DEAT-UEA: 7 (4–11) ms, P = 0.000). The incidence of EAT and BEAT-lu being the same site was significantly higher than that between EAT and BEAT (48.15% vs 18.52%, P = 0.021).
Conclusions
RVOT VAs often originate from voltage-transitional zone, and automatic annotation of LAT usually located at later high-amplitude far-field potential. Lumipoint algorithms could improve the accuracy of LAT automatic annotation, and it was plausible to ablate RVOT VAs just according to the automatically annotated BEAS-lu.


Similar content being viewed by others
References
Takigawa M, Derval N, Martin CA, Vlachos K, Denis A, Kitamura T, et al. A simple mechanism underlying the behavior of reentrant atrial tachycardia during ablation. Heart Rhythm. 2019;16(4):553–61. https://doi.org/10.1016/j.hrthm.2018.10.031.
Knecht S, Spies F, Altmann D, Reichlin T, Sticherling C, Kuhne M. Electroanatomic mapping of atrial tachycardia-manual vs automated annotation. Heart Rhythm Case Rep. 2017;3(2):145–7. https://doi.org/10.1016/j.hrcr.2016.11.002.
Liu M, Jiang J, Su C, Li J, Chen X, Ma Y, et al. Electrophysiological characteristics of the earliest activation site in idiopathic right ventricular outflow tract arrhythmias under mini-electrode mapping. J Cardiovasc Electrophysiol. 2019;30(5):642–50. https://doi.org/10.1111/jce.13856.
Martin CA, Takigawa M, Martin R, Maury P, Meyer C, Wong T, et al. Use of novel electrogram "Lumipoint" algorithm to detect critical isthmus and abnormal potentials for ablation in ventricular tachycardia. JACC Clin Electrophysiol. 2019;5(4):470–9. https://doi.org/10.1016/j.jacep.2019.01.016.
Wang Z, Zhang H, Peng H, Shen X, Sun Z, Zhao C, et al. Voltage combined with pace mapping is simple and effective for ablation of noninducible premature ventricular contractions originating from the right ventricular outflow tract. Clin Cardiol. 2016;39(12):733–8. https://doi.org/10.1002/clc.22598.
Yamashina Y, Yagi T, Namekawa A, Ishida A, Sato H, Nakagawa T, et al. Distribution of successful ablation sites of idiopathic right ventricular outflow tract tachycardia. Pacing Clin Electrophysiol. 2009;32(6):727–33. https://doi.org/10.1111/j.1540-8159.2009.02358.x.
Liao Z, Zhan X, Wu S, Xue Y, Fang X, Liao H, et al. Idiopathic ventricular arrhythmias originating from the pulmonary sinus cusp: prevalence, electrocardiographic/electrophysiological characteristics, and catheter ablation. J Am Coll Cardiol. 2015;66(23):2633–44. https://doi.org/10.1016/j.jacc.2015.09.094.
Liang Z, Ren X, Zhang T, Han Z, Dong J, Wang Y. Mapping and ablation of RVOT-type arrhythmias: comparison between the conventional and reversed U curve methods. J Interv Card Electrophysiol. 2018;52(1):19–30. https://doi.org/10.1007/s10840-018-0365-8.
Zhang J, Tang C, Zhang Y, Su X. Pulmonary sinus cusp mapping and ablation: a new concept and approach for idiopathic right ventricular outflow tract arrhythmias. Heart Rhythm. 2018;15(1):38–45. https://doi.org/10.1016/j.hrthm.2017.08.007.
Tada H, Tadokoro K, Miyaji K, Ito S, Kurosaki K, Kaseno K, et al. Idiopathic ventricular arrhythmias arising from the pulmonary artery: prevalence, characteristics, and topography of the arrhythmia origin. Heart Rhythm. 2008;5(3):419–26. https://doi.org/10.1016/j.hrthm.2007.12.021.
Tedrow UB, Stevenson WG. Recording and interpreting unipolar electrograms to guide catheter ablation. Heart Rhythm. 2011;8(5):791–6. https://doi.org/10.1016/j.hrthm.2010.12.038.
Pathik B, Lee G, Sacher F, Haissaguerre M, Jais P, Massoullie G, et al. Epicardial-endocardial breakthrough during stable atrial macroreentry: evidence from ultra-high-resolution 3-dimensional mapping. Heart Rhythm. 2017;14(8):1200–7. https://doi.org/10.1016/j.hrthm.2017.04.043.
Mantziari L, Butcher C, Kontogeorgis A, Panikker S, Roy K, Markides V, et al. Utility of a novel rapid high-resolution mapping system in the catheter ablation of arrhythmias: an initial human experience of mapping the atria and the left ventricle. JACC Clin Electrophysiol. 2015;1(5):411–20. https://doi.org/10.1016/j.jacep.2015.06.002.
Nakagawa H, Ikeda A, Sharma T, Lazzara R, Jackman WM. Rapid high resolution electroanatomical mapping: evaluation of a new system in a canine atrial linear lesion model. Circ Arrhythm Electrophysiol. 2012;5(2):417–24. https://doi.org/10.1161/CIRCEP.111.968602.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, M., Yang, D., Su, C. et al. Automatic annotation of local activation time was improved in idiopathic right ventricular outflow tract ventricular arrhythmia by novel electrogram “Lumipoint” algorithm. J Interv Card Electrophysiol 61, 79–85 (2021). https://doi.org/10.1007/s10840-020-00773-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00773-3