Abstract
Purpose
To determine the efficacy and identify the relevant factors for durable lesion creation in pulmonary vein isolation (PVI) using a high-power short-duration (HPSD) strategy.
Methods
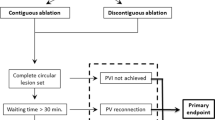
Thirty-two consecutive patients who underwent PVI using HPSD (50 W) (HP group: HP-G) were compared with 32 controls using normal power (25–40 W) (conventional group: C-G). The segments were divided into 12 segments per group; thus, there were 768 segments for analysis. Radiofrequency (RF) ablation (RFA) was mainly performed under guidance with a unipolar electrogram at the distal tip of the ablation catheter in both groups. The high-power strategy reduced radiofrequency energy (P < 0.0001), RFA time (P < 0.0001), acute pulmonary vein reconnection (PVR) segments (P = 0.02), and several three-dimensional-mapping-related indices except for minimum impedance drop (Imp-min).
Results
There was a significant difference only in Imp-min between the subjects with acute PVR and those without in the HP-G (P = 0.002). Multivariate analysis revealed Imp-min to be the only independent predictor of the absence of PVR after adjusting for maximum inter-lesion distance and minimum ablation index (odds ratio [OR] 1.22, 95% confidence interval [CI] 1.07–1.39, P = 0.001). In the region-specific analysis, this was attenuated in posterior segments, where the HP strategy independently predicted the absence of PVR (OR 2.80 [95% CI 1.32–6.30], P = 0.007).
Conclusion
The HPSD strategy reduced RF time, RF energy, and three-dimensional mapping-related indices but also improved the acute outcome. The HP strategy may be a sophisticated strategy under guidance with the impedance drop rather than the ablation index.





Similar content being viewed by others
References
Jais P, Cauchemez B, Macle L, Daoud E, Khairy P, Subbiah R, et al. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation. 2008;118:2498–505.
Terasawa T, Balk EM, Chung M, Garlitski AC, Alsheikh-Ali AA, Lau J, et al. Systematic review: comparative effectiveness of radiofrequency catheter ablation for atrial fibrillation. Ann Intern Med. 2009;151:191–202.
Kautzner J, Neuzil P, Lambert H, Peichl P, Petru J, Chiak R, et al. EFFICAS II: optimization of catheter contact force improves outcome of pulmonary vein isolation for paroxysmal atrial fibrillation. Europace. 2015;17:1229–35.
Nakagawa H, Ikeda A, Constantine G, Govari A, Sharma T, Pitha JV, et al. Controlling lesion size and incidence of steam pop by controlling contact force, radiofrequency power and application time (Force-Power-Time Index) in canine beating heart. Heart Rhythm. 2012;9:S5.
Bhaskaran A, Chik W, Pouliopoulos J, Nalliah C, Qian P, Barry T, et al. Five seconds of 50-60 W radio frequency atrial ablations were transmural and safe: an in vitro mechanistic assessment and force-controlled in vivo validation. Europace. 2017;19:874–80.
Winkle RA, Mead RH, Engel G, Patrawala RA. Atrial fibrillation ablation: “perpetual motion” of open irrigated tip catheters at 50 W is safe and improves outcomes. Pacing Clin Electrophysiol. 2011;34:531–9.
Winkle RA, Moskovitz R, Mead RH, Engel G, Kong MH, Fleming W, et al. Atrial fibrillation ablation using very short duration 50 W ablations and contact force sensing catheters. J Interv Card Electrophysiol. 2018;52:1–8.
Winkle RA, Mohanty S, Patrawala RA, Mead RH, Kong MH, Engel G, et al. Low complication rates using high power (45-50 W) for short duration for atrial fibrillation ablations. Heart Rhythm. 2019;16:165–9.
Ejima K, Henmi R, Iwanami Y, Yagishita D, Shoda M, Hagiwara N. Comparison of the efficacy of empiric thoracic vein isolation for the treatment of paroxysmal and persistent atrial fibrillation in patients without structural heart disease. J Cardiovasc Electrophysiol. 2017;28:266–72.
Bortone A, Braut-Noble G, Apetiti A, Marijon E. Elimination of the negative component of the unipolar atrial electrogram as an in vivo marker of transmural lesion creation: acute study in canines. Circ Arrhythm Electrophysiol. 2015;8:905–11.
Bortone A, Apperiri A, Bouzeman A, Maupas E, Ciovotaru V, Boulenc JM, et al. Unipolar signal modification as a guide for lesion creation during radiofrequency application in the left atrium: prospective study in humans in the setting of paroxysmal atrial fibrillation catheter ablation. Circ Arrhythm Electrophysiol. 2013;6:1095–102.
Nakagawa H, Yamanashi WS, Pitha JV, Arruda M, Wang X, Ohtomo K, et al. Comparison of in vivo tissue temperature profile and lesion geometry for radiofrequency ablation with a saline-irrigated electrode versus temperature control in a canine thigh muscle preparation. Circulation. 1995;91:2264–73.
Bourier F, Duchateau J, Vlachos K, Lam A, Martin CA, Takigawa M, et al. High-power short-duration versus standard radiofrequency ablation: insights on lesion metrics. J Cardiovasc Electrophysiol. 2018;29:1570–5.
Dhillon G, Ahsan S, Honarbakhsh S, Lim W, Baca M, Graham A, et al. A multicentered evaluation of ablation at higher power guided by ablation index: establishing ablation targets for pulmonary vein isolation. J Cardiovasc Electrophysiol. 2019;30:357–65.
Ullah W, Hunter RJ, Finlay MC, Mclean A, Dhinoja MB, Sporton S, et al. Ablation index and surround flow catheter irrigation: impedance-based appraisal in clinical ablation. JACC Clin Electrophysiol. 2017;3:1080–8.
Phlips T, Taghji P, El Haddad M, Wolf M, Knecht S, Vandekerckhove Y, et al. Improving procedural and one-year outcome after contact force-guided pulmonary vein isolation: the role of interlesion distance, ablation index, and contact force variability in the ‘CLOSE’-protocol. Europace. 2018;20:419–27.
Ikeda A, Nakagawa H, Lambert H, Shar DC, Fonck E, Yulzari A, et al. Relationship between catheter contact force and radiofrequency lesion size and incidence of steam pop in the beating canine heart: electrogram amplitude, impedance, and electrode temperature are poor predictors of electrode-tissue contact force and lesion size. Circ Arrhythm Electrophysiol. 2014;7:1174–80.
Chinitz JS, Kapur S, Barbhajya C, Kumar S, John R, Epstein LM, et al. Sites with small impedance decrease during catheter ablation for atrial fibrillation are associated with recovery of pulmonary vein conduction. J Cardiovasc Electrophysiol. 2016;27:1390–8.
Reichlin T, Knecht S, Lane C, Kuhne M, Nof E, Chopra N, et al. Initial impedance decrease as an indicator of good catheter contact: insights from radiofrequency ablation with force sensing catheters. Heart Rhythm. 2014;11:194–201.
Muller P, Dietrich JW, Halbfass P, Abouarab A, Fochler F, Szollosi A, et al. Higher incidence of esophageal lesions after ablation of atrial fibrillation related to the use of esophageal temperature probes. Heart Rhythm. 2015;12:1464–9.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by our institutional review board and was performed in accordance with institutional guidelines. All patients provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yazaki, K., Ejima, K., Kanai, M. et al. Impedance drop predicts acute electrical reconnection of the pulmonary vein-left atrium after pulmonary vein isolation using short-duration high-power exposure. J Interv Card Electrophysiol 59, 575–584 (2020). https://doi.org/10.1007/s10840-019-00691-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00691-z