Abstract
Background
Heart Rate Score (HrSc), a novel index found to predict mortality in patients with implantable defibrillator (ICD) and cardiac resynchronization defibrillator (CRT-D) devices, is associated with mortality in ICD and CRT-D recipients when HrSc is ≥ 70%. Implantable defibrillator shocks have also been associated with increased mortality in ICD and CRT-D recipients. The objective of this study was to evaluate the relationships between HrSc, shocks, and mortality in ICD and CRT-D patients.
Methods
HrSc was calculated from atrial sensed and paced rate histograms collected from the 2006–2011 ALTITUDE remote interrogation database. Shocks were determined in the first year of follow-up. Mortality was assessed over the next 4 years by the Social Security Death Index. Four multivariable models were run: ICD and CRT-D, shock and no shock, with mortality as the outcome and HrS as predictor.
Results
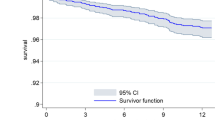
Data from 49,358 ICD and 55,953 CRT-D patients were divided into HrSc: ≥ 70%, 30–69%, and < 30%. Shock rates differed between HrSc groups (p < 0.001) for ICD and CRT-D patients. However, the lowest mortality risk HrSc (< 30%) had the highest shock rate. Both highest HrSc (> 70%; p < 0.001) and shocks (p < 0.001) predicted mortality during follow-up. Mortality was unrelated to interactions between HrSc and shocks in ICD patients (p = 0.275) or CRT-D patients (p < 0.079). Comparing HrSc ≥ 70% to HrSc < 30%, HrSc ≥ 70% predicted mortality in CRT-D (HR 1.40; 95% CI 1.29–1.52) and ICD (HR 1.23; 95% CI 1.11–1.36) patients regardless of shocks (P < 0.001 for both).
Conclusions
Patients with ICDs or CRT-Ds having the lowest mortality risk HrSc had the highest shock rate. Shocks and HrSc appear to complement each other as predictors of mortality.






Similar content being viewed by others
References
Goldenberg I, Vyas AK, Hall WJ, Moss AJ, Wang H, He H, et al. Risk stratification for primary implantation of a cardioverter-defibrillator in patients with ischemic left ventricular dysfunction. J Am Coll Cardiol. 2008;51:288–96.
Daubert JP, Zareba W, Cannom DS, McNitt S, Rosero SZ, Wang P, et al. Inappropriate implantable cardioverter-defibrillator shocks in MADIT II: frequency, mechanisms, predictors, and survival impact. J Am Coll Cardiol. 2008;51:1357–65.
Cygankiewicz I, Gillespie J, Zareba W, Brown MW, Goldenberg I, Klein H, et al. Predictors of long-term mortality in Multicenter Automatic Defibrillator Implantation Trial II (MADIT II) patients with implantable cardioverter-defibrillators. Heart Rhythm. 2009;6:468–73.
Powell BD, Saxon LA, Boehmer JP, Day JD, Gilliam FR 3rd, Heidenreich PA, et al. Survival after shock therapy in implantable cardioverter-defibrillator and cardiac resynchronization therapy-defibrillator recipients according to rhythm shocked. The ALTITUDE survival by rhythm study. J Am Coll Cardiol. 2013;62:1674–9.
Borne RT, Varosy PD, Masoudi FA. Implantable cardioverter-defibrillator shocks: epidemiology, outcomes, and therapeutic approaches. JAMA Intern Med. 2013;173:859–65.
Dichtl W, Wolber T, Paoli U, Brullmann S, Stuhlinger M, Berger T, et al. Appropriate therapy but not inappropriate shocks predict survival in implantable cardioverter defibrillator patients. Clin Cardiol. 2011;34:433–6.
Poole JE, Johnson GW, Hellkamp AS, Anderson J, Callans DJ, Raitt MH, et al. Prognostic importance of defibrillator shocks in patients with heart failure. N Engl J Med. 2008;359:1009–17.
Sun S, Johnson J, Degroot P, Brown ML, Obel O. Effect of ICD therapies on mortality in the OMNI trial. J Cardiovasc Electrophysiol. 2016;27:192–9.
Sweeney MO, Sherfesee L, DeGroot PJ, Wathen MS, Wilkoff BL. Differences in effects of electrical therapy type for ventricular arrhythmias on mortality in implantable cardioverter-defibrillator patients. Heart Rhythm. 2010;7:353–60.
Streitner F, Herrmann T, Kuschyk J, Lang S, Doesch C, Papavassiliu T, et al. Impact of shocks on mortality in patients with ischemic or dilated cardiomyopathy and defibrillators implanted for primary prevention. PLoS One. 2013;8:e63911.
Olshansky B, Richards M, Sharma A, Wold N, Jones P, Perschbacher D, et al. Survival after rate-responsive programming in patients with cardiac resynchronization therapy-defibrillator implants is associated with a novel parameter: the heart rate score. Circ Arrhythm Electrophysiol. 2016;9.
Wilkoff BL, Richards M, Sharma A, Wold N, Jones P, Perschbacher D, et al. A device histogram-based simple predictor of mortality risk in ICD and CRT-D patients: the heart rate score. Pacing Clin Electrophysiol. 2017;40:333–43.
Saxon LA, Hayes DL, Gilliam FR, Heidenreich PA, Day J, Seth M, et al. Long-term outcome after ICD and CRT implantation and influence of remote device follow-up: the ALTITUDE survival study. Circulation. 2010;122:2359–67.
Chang PM, Powell BD, Jones PW, Carter N, Hayes DL, Saxon LA. Implantable cardioverter defibrillator programming characteristics, shocked rhythms, and survival among patients under thirty years of age. J Cardiovasc Electrophysiol. 2016;27:1183–90.
Moss AJ, Schuger C, Beck CA, Brown MW, Cannom DS, Daubert JP, et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med. 2012;367:2275–83.
Elhendy A, Mahoney DW, Khandheria BK, Burger K, Pellikka PA. Prognostic significance of impairment of heart rate response to exercise: impact of left ventricular function and myocardial ischemia. J Am Coll Cardiol. 2003;42:823–30.
Khan MN, Pothier CE, Lauer MS. Chronotropic incompetence as a predictor of death among patients with normal electrograms taking beta blockers (metoprolol or atenolol). Am J Cardiol. 2005;96:1328–33.
Kiviniemi AM, Tulppo MP, Hautala AJ, Makikallio TH, Perkiomaki JS, Seppanen T, et al. Long-term outcome of patients with chronotropic incompetence after an acute myocardial infarction. Ann Med. 2011;43:33–9.
Savonen KP, Kiviniemi V, Laukkanen JA, Lakka TA, Rauramaa TH, Salonen JT, et al. Chronotropic incompetence and mortality in middle-aged men with known or suspected coronary heart disease. Eur Heart J. 2008;29:1896–902.
Zafrir B, Azencot M, Dobrecky-Mery I, Lewis BS, Flugelman MY, Halon DA. Resting heart rate and measures of effort-related cardiac autonomic dysfunction predict cardiovascular events in asymptomatic type 2 diabetes. Eur J Prev Cardiol. 2016;23:1298–306.
Kramer DB, Mitchell SL, Monteiro J, Jones PW, Normand SL, Hayes DL, et al. Patient activity and survival following implantable cardioverter-defibrillator implantation: the ALTITUDE activity study. J Am Heart Assoc. 2015;4.
Richards M, Olshansky B, Sharma AD, Wold N, Jones P, Perschbacher D, et al. Addition of minute ventilation to rate-response pacing improves heart rate score more than accelerometer alone. Heart Rhythm. 2018;15:1730–5.
Olshansky B, Richards M, Sharma A, Wold N, Perschbacher D and Wilkoff BL. Programmed lower rate limit in CRT-Ds - is there one best approach? Circulation. 2017.
Funding
B. Olshansky, B. Wilkoff, and M. Richards received no compensation for this work.
P. Jones, N. Wold, D. Pershbacher, and A. Sharma received salary support from Boston Scientific but not specifically for this project.
Boston Scientific did not charge for the database.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Brian Olshansky: Lundbeck, Boehringer Ingelheim, Amarin, Respicardia, Sanofi Aventis
Mark Richards: Boston Scientific, Boehringer Ingelheim, Medtronic, Biotronik, Janssen, Pfizer
Arjun Sharma: Cardialen, VivaQuant, 3M
Paul W. Jones: Boston Scientific
Nick Wold: Boston Scientific
David Pershbacher: Boston Scientific
Bruce L. Wilkoff: Consultant: Medtronic, St. Jude, Spectranetics, Speaker: Medtronic, Spectranetics, St. Jude, Convatec
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Olshansky, B., Richards, M., Sharma, A.D. et al. Heart rate score predicts mortality independent of shocks in ICD and CRT-D patients. J Interv Card Electrophysiol 58, 103–111 (2020). https://doi.org/10.1007/s10840-019-00688-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00688-8