Abstract
Purpose
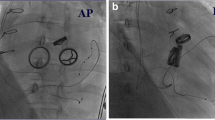
Transvenous right ventricular pacing has traditionally been avoided after surgical tricuspid valve repair or replacement because of possible valvular dysfunction. Epicardial pacing has been used but it requires surgical thoracotomy and has higher lead failure rates when compared to transvenous pacing. We evaluated the lead stability and clinical outcomes in patients with isolated coronary sinus (CS) lead due to relative contraindication to transvenous pacing from prior tricuspid valve (TV) surgery.
Methods
We retrospectively examined a single-center cohort of 34 patients with TV disease and/or surgery who underwent permanent pacemaker implantation with a left ventricular CS lead as the only ventricular pacing lead (to avoid crossing the TV). The clinical outcome, echocardiographic data, and pacing thresholds were evaluated at follow-up.
Results
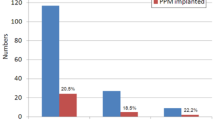
We implanted 19 patients with a single-CS lead and 15 patients with dual-CS leads. The average left ventricular ejection fraction was 56 ± 13% prior to lead implantation and remained stable at 2-year follow-up. The tricuspid regurgitation remained mild at follow-up. The average lead pacing threshold was 1.2 ± 0.6 V × ms at implant and 1.1 ± 0.4 V × ms at 2-year follow-up (P = 0.39). For patients with dual-CS leads, the pacing threshold was 1.2 ± 0.7 V × ms at implant and 1.1 ± 0.5 V × ms at 2-year follow-up (P = 0.52).
Conclusions
The use of ventricular pacing entirely through the CS is an effective and minimally invasive method that provides stable pacing for patients with prior TV surgery in whom transvenous lead placement either is not possible or is relatively contraindicated.





Similar content being viewed by others
References
Delling FN, Hassan ZK, Piatkowski G, et al. Tricuspid regurgitation and mortality in patients with transvenous permanent pacemaker leads. Am J Cardiol. 2016;117:988.92.
Lin G, Nishimura RA, Connolly HM, Dearani JA, Sundt TM, Hayes DL. Severe symptomatic tricuspid valve regurgitation due to permanent pacemaker or implantable cardioverter-defibrillator leads. J Am Coll Cardiol. 2005;45:1672–5.
Leibowitz DW, Rosenheck S, Pollak A, Geist M, Gilon D. Transvenous pacemaker leads do not worsen tricuspid regurgitation: a prospective echocardiographic study. Cardiology. 2000;93:74–7.
Schleifer JW, Pislaru SV, Lin G, Powell BD, Espinosa R, Koestler C, et al. Effect of ventricular pacing lead position on tricuspid regurgitation: a randomized prospective trial. Heart Rhythm. 2018;15:1009–16.
McCarthy PM, Bhudia SK, Rajeswaran J, et al. Tricuspid valve repair: durability and risk factors for failure. J Thorac Cardiovasc Surg. 2004;127:674–85.
Mazine A, Bouchard D, Moss E, Marquis-Gravel G, Perrault LP, Demers P, et al. Transvalvular pacemaker leads increase the recurrence of regurgitation after tricuspid valve repair. Ann Thorac Surg. 2013;96:816–22.
Gordon RS, Ivanov J, Cohen G, Ralph-Edwards AL. Permanent cardiac pacing after a cardiac operation: predicting the use of permanent pacemakers. Ann Thorac Surg. 1998;66:1698–704.
Jokinen JJ, Turpeinen AK, Pitkanen O, Hippelainen MJ, Hartikainen JE. Pacemaker therapy after tricuspid valve operations: implications on mortality, morbidity, and quality of life. Ann Thorac Surg. 2009;87:1806–14.
Ector B, Willems R, Heidbüchel H, et al. Epicardial pacing: a single-centre study on 321 leads in 138 patients. Acta Cardiol. 2006;61:343–51. https://doi.org/10.2143/AC.61.3.2014839.
McLeod CJ, Jost CHA, Warnes CA, et al. Epicardial versus endocardial permanent pacing in adults with congenital heart disease. J Interv Card Electrophysiol. 2010;28:235–43.
Noheria A, van Zyl M, Scott LR, Srivathsan K, Madhavan M, Asirvatham SJ, et al. Single-site ventricular pacing via the coronary sinus in patients with tricuspid valve disease. Europace. 2018;20:636–42.
Sideris S, Drakopoulou M, Oikonomopoulos G, et al. Left ventricular pacing through coronary sinus is feasible and safe for patients with prior tricuspid valve intervention. Pacing Clin Electrophysiol. 2016;39:378–81.
Kim JB, Spevack DM, Tunick PA, Bullinga JR, Kronzon I, Chinitz LA, et al. The effect of transvenous pacemaker and implantable cardioverter defibrillator lead placement on tricuspid valve function: an observational study. J Am Soc Echocardiogr. 2008;21:284–7.
Paniagua D, Aldrich HR, Lieberman EH, Lamas GA, Agatston AS. Increased prevalence of significant tricuspid regurgitation in patients with transvenous pacemakers leads. Am J Cardiol. 1998;82:1130–2 A9.
Saito M, Iannaccone A, Kaye G, Negishi K, Kosmala W, Marwick TH. Effect of right ventricular pacing on right ventricular mechanics and tricuspid regurgitation in patients with high-grade atrioventricular block and sinus rhythm (from the protection of left ventricular function during right ventricular pacing study). Am J Cariol. 2015;116:1875–82.
Saxon LA, Olshansky B, Volosin K, et al. Influence of left ventricular lead location on outcomes in the COMPANION study. J Cardiovasc Electrophysiol. 2009;20:764–8.
Biffi M, Exner DV, Crossley GH, Ramza B, Coutu B, Tomassoni G, et al. Occurrence of phrenic nerve stimulation in cardiac resynchronization therapy patients: the role of left ventricular lead type and placement site. Europace. 2013;15:77–82.
Salcedo J, Doshi RN. Successful cardiac resynchronization defibrillator placement in a patient with tetralogy of Fallot, widened QRS duration, and mechanical tricuspid valve replacement using dual-site left ventricular venous lead placement. J Innov Card Rhythm Manag. 2012;3:829–31.
Kiehl EL, Makki T, Kumar R, Gumber D, Kwon DH, Rickard JW, et al. Incidence and predictors of right ventricular pacing-induced cardiomyopathy in patients with complete atrioventricular block and preserved left ventricular systolic function. Heart Rhythm. 2016;13:2272–8.
Moss AJ, Hall WJ, Cannom DS, Klein H, Brown MW, Daubert JP, et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N Engl J Med. 2009;361:1329–38.
Gasparini M, Bocchiardo M, Lunati M, et al. Comparison of 1-year effects of left ventricular and biventricular pacing in patients with heart failure who have ventricular arrhythmias and left bundle-branch block: the Bi vs Left Ventricular Pacing: an International Pilot Evaluation on Heart Failure Patients with Ventricular Arrhythmias (BELIEVE) multicenter prospective randomized pilot study. Am Heart J. 2006;152:155.e1–7.
Rao RK, Kumar UN, Schafer J, Viloria E, De Lurgio D, Foster E. Reduced ventricular volumes and improved systolic function with cardiac resynchronization therapy: a randomized trial comparing simultaneous biventricular pacing, sequential biventricular pacing, and left ventricular pacing. Circulation. 2007;115:2136–44.
Thibault B, Ducharme A, Harel F, White M, O'Meara E, Guertin MC, et al. Left ventricular versus simultaneous biventricular pacing in patients with heart failure and a QRS complex ≥120 milliseconds. Circulation. 2011;124:2874–81.
Leyva F, Zegard A, Qiu T, et al. Cardiac resynchronization therapy using quadripolar versus non-quadripolar left ventricular leads programmed to biventricular pacing with single-site left ventricular pacing: impact on survival and heart failure hospitalization. J Am Heart Assoc. 2017;6(10):e007026. https://doi.org/10.1161/JAHA.117.007026.
Bordachar P, Gras D, Clementy N, Defaye P, Mondoly P, Boveda S, et al. Clinical impact of an additional left ventricular lead in cardiac resynchronization therapy nonresponders: the V(3) trial. Heart Rhythm. 2018;15:870–6.
Ypenburg C, van Bommel RJ, Borleffs CJ, Bleeker GB, Boersma E, Schalij MJ, et al. Long-term prognosis after cardiac resynchronization therapy is related to the extent of left ventricular reverse remodeling at midterm follow-up. J Am Coll Cardiol. 2009;53:483–90.
Harcombe AA, Newell SA, Ludman PF, Wistow TE, Sharples LD, Schofield PM, et al. Late complications following permanent pacemaker implantation or elective unit replacement. Heart. 1998;80(3):240–4. https://doi.org/10.1136/hrt.80.3.240.
Kleemann T, Becker T, Strauss M, Dyck N, Weisse U, Saggau W, et al. Prevalence of bacterial colonization of generator pockets in implantable cardioverter defibrillator patients without signs of infection undergoing generator replacement or lead revision. Europace. 2010;12:58–63.
Sharma PS, Subzposh FA, Ellenbogen KA, Vijayaraman P. Permanent His-bundle pacing in patients with prosthetic cardiac valves. Heart Rhythm. 2017;14:59–64.
Boveda S, Durand P, Combes S, Mariottini CJ. Leadless pacemaker surrounded by three valvular prostheses. Heart Rhythm. 2017;14:1421.
Reddy VY, Exner DV, Cantillon DJ, Doshi R, Bunch TJ, Tomassoni GF, et al. Percutaneous implantation of an entirely intracardiac leadless pacemaker. N Engl J Med. 2015;373:1125–35.
Tang GH, Kaple R, Cohen M, Dutta T, Undemir C, Ahmad H, et al. First percutaneous Micra leadless pacemaker implantation and tricuspid valve repair with MitraClip NT for lead-associated severe tricuspid regurgitation. Eurointervention. 2017;12:e1845–8.
Salaun E, Tovmassian L, Simonnet B, Giorgi R, Franceschi F, Koutbi-Franceschi L, et al. Right ventricular and tricuspid valve function in patients chronically implanted with leadless pacemakers. Europace. 2018;20:823–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by our local Institutional Review Board at the Keck University of Southern California School of Medicine. The study protocol adheres to the ethical guidelines of the 2008 Declaration of Helsinki.
Conflict of interest
R. Doshi is a consultant and received fellowship support from Abbott Medical and Boston Scientific.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was provided according to institutional protocols.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, C.C., Do, K., Patel, S. et al. Single- and dual-site ventricular pacing entirely through the coronary sinus for patients with prior tricuspid valve surgery. J Interv Card Electrophysiol 56, 79–89 (2019). https://doi.org/10.1007/s10840-019-00599-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00599-8