Abstract
Background
Atrial fibrillation ablation results in microbubbles and particulate emboli formation. We aimed to develop and test the early feasibility of a novel ablation hood to contain microbubbles and particulate emboli with the ultimate goal of preventing systemic embolization.
Methods
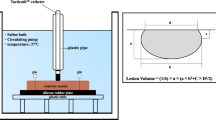
In seven canines, we developed, iterated, and tested a novel retractable hood that can cover the catheter-tissue ablation site. The number and volume (nL) of microbubbles formed during ablation with and without the hood was measured using an extracorporeal circulation loop. Wilcoxon’s signed-rank test was used to compare the number of bubbles detected with and without the hood.
Results
The hood reduced systemic embolization of microbubbles in 21/28 (75%) of ablations. Both atrial and ventricular ablations showed a statistically significant reduction in bubble number (476 ± 811 without hood vs 173 ± 226 with hood, p = 0.02; 2669 ± 1623 without hood vs 1417 ± 970 with hood, p = 0.04, respectively) and bubble volume (3.3 ± 7.6 nL without hood vs 0.2 ± 0.56 nL with hood, p = 0.006; 6.1 ± 5.2 nL without hood vs 1.9 ± 1.4 nL with hood, p = 0.05, respectively).
Conclusions
Use of a novel hood to cover the ablation catheter at the site of catheter-tissue contact has the potential to provide a means to reduce systematic embolization of microbubbles. Further work is required to examine particulate emboli, but these data show the early feasibility of this design concept.






Similar content being viewed by others
References
Calkins H, Kuck KH, Cappato R, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design: a report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation. Developed in partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC) and the European Cardiac Arrhythmia Society (ECAS); and in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), the Asia Pacific Heart Rhythm Society (APHRS), and the Society of Thoracic Surgeons (STS). Endorsed by the governing bodies of the American College of Cardiology Foundation, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, the Asia Pacific Heart Rhythm Society, and the Heart Rhythm Society. Heart Rhythm. 2012;9(4):632–96 e621.
Li P-J, Xiao J, Yang Q, Feng Y, Wang T, Liu GJ, et al. Network meta-analysis of efficacy and safety of competitive oral anticoagulants in patients undergoing radiofrequency catheter ablation of atrial fibrillation. J Interv Card Electrophysiol. 2016;46(3):213–24.
Lickfett L, Hackenbroch M, Lewalter T, Selbach S, Schwab JO, Yang A, et al. Cerebral diffusion-weighted magnetic resonance imaging: a tool to monitor the thrombogenicity of left atrial catheter ablation. J Cardiovasc Electrophysiol. 2006;17(1):1–7.
Herrera Siklody C, Deneke T, Hocini M, et al. Incidence of asymptomatic intracranial embolic events after pulmonary vein isolation: comparison of different atrial fibrillation ablation technologies in a multicenter study. J Am Coll Cardiol. 2011;58(7):681–8.
Nakamura T, Okishige K, Kanazawa T, Yamashita M, Kawaguchi N, Kato N, et al. Incidence of silent cerebral infarctions after catheter ablation of atrial fibrillation utilizing the second-generation cryoballoon. Europace. 2017;19(10):1681–8.
Deneke T, Shin DI, Balta O, Bünz K, Fassbender F, Mügge A, et al. Postablation asymptomatic cerebral lesions: long-term follow-up using magnetic resonance imaging. Heart Rhythm. 2011;8(11):1705–11.
Miyazaki S, Kajiyama T, Yamao K, et al. Silent cerebral events/lesions after second-generation cryoballoon ablation: how can we reduce the risk of silent strokes? Heart Rhythm. 2019;16(1):41–8
Haines DE, Stewart MT, Barka ND, Kirchhof N, Lentz LR, Reinking NM, et al. Microembolism and catheter ablation II: effects of cerebral microemboli injection in a canine model. Circ Arrhythm Electrophysiol. 2013;6(1):23–30.
Haeusler KG, Koch L, Herm J, et al. 3 Tesla MRI-detected brain lesions after pulmonary vein isolation for atrial fibrillation: results of the MACPAF study. J Cardiovasc Electrophysiol. 2013;24(1):14–21.
Medi C, Evered L, Silbert B, Teh A, Halloran K, Morton J, et al. Subtle post-procedural cognitive dysfunction after atrial fibrillation ablation. J Am Coll Cardiol. 2013;62(6):531–9.
Madhavan M, Govil Shalini R, Asirvatham SJ. Signals. Circ Arrhythm Electrophysiol. 2012;5(1):2–4.
Ringelstein EB, Droste DW, Babikian VL, et al. Consensus on microembolus detection by TCD. Stroke. 1998;29(3):725–9.
von Bary C, Deneke T, Arentz T, Schade A, Lehrmann H, Schwab-Malek S, et al. Clinical impact of the microembolic signal burden during catheter ablation for atrial fibrillation: just a lot of noise? J Ultrasound Med. 2018;37(5):1091–101.
Marrouche NF, Martin DO, Wazni O, Gillinov AM, Klein A, Bhargava M, et al. Phased-array intracardiac echocardiography monitoring during pulmonary vein isolation in patients with atrial fibrillation: impact on outcome and complications. Circulation. 2003;107(21):2710–6.
Oh S, Kilicaslan F, Zhang Y, et al. Avoiding microbubbles formation during radiofrequency left atrial ablation versus continuous microbubbles formation and standard radiofrequency ablation protocols: comparison of energy profiles and chronic lesion characteristics. J Cardiovasc Electrophysiol. 2006;17(1):72–7.
Wood MA, Shaffer KM, Ellenbogen AL, Ownby ED. Microbubbles during radiofrequency catheter ablation: composition and formation. Heart Rhythm. 2005;2(4):397–403.
Alaeddini J, Wood MA, Lee BP, Ellenbogen KA. Incidence, time course, and characteristics of microbubble formation during radiofrequency ablation of pulmonary veins with an 8-mm ablation catheter. Pacing Clin Electrophysiol. 2006;29(9):979–84.
Kalman JM, Fitzpatrick AP, Olgin JE, Chin MC, Lee RJ, Scheinman MM, et al. Biophysical characteristics of radiofrequency lesion formation in vivo: dynamics of catheter tip-tissue contact evaluated by intracardiac echocardiography. Am Heart J. 1997;133(1):8–18.
Gaita F, Caponi D, Pianelli M, Scaglione M, Toso E, Cesarani F, et al. Radiofrequency catheter ablation of atrial fibrillation: a cause of silent thromboembolism? Magnetic resonance imaging assessment of cerebral thromboembolism in patients undergoing ablation of atrial fibrillation. Circulation. 2010;122(17):1667–73.
Haines DE, Stewart MT, Dahlberg S, et al. Microembolism and catheter ablation I: a comparison of irrigated radiofrequency and multielectrode-phased radiofrequency catheter ablation of pulmonary vein ostia. Circ Arrhythm Electrophysiol. 2013;6(1):16–22.
Takami M, Lehmann HI, Parker KD, Welker KM, Johnson SB, Packer DL. Effect of left atrial ablation process and strategy on microemboli formation during irrigated radiofrequency catheter ablation in an in vivo model. Circ Arrhythm Electrophysiol. 2016;9(1):e003226.
Schwarz N, Kuniss M, Nedelmann M, Kaps M, Bachmann G, Neumann T, et al. Neuropsychological decline after catheter ablation of atrial fibrillation. Heart Rhythm. 2010;7(12):1761–7.
Wieczorek M, Lukat M, Hoeltgen R, et al. Investigation into causes of abnormal cerebral MRI findings following PVAC duty-cycled, phased RF ablation of atrial fibrillation. J Cardiovasc Electrophysiol. 2013;24(2):121–8.
Khairy P, Chauvet P, Lehmann J, Lambert J, Macle L, Tanguay JF̧, et al. Lower incidence of thrombus formation with cryoenergy versus radiofrequency catheter ablation. Circulation. 2003;107(15):2045–50.
Miyazaki S, Watanabe T, Kajiyama T, Iwasawa J, Ichijo S, Nakamura H, et al. Thromboembolic risks of the procedural process in second-generation cryoballoon ablation procedures: analysis from real-time transcranial Doppler monitoring. Circ Arrhythm Electrophysiol. 2017;10(12):e005612.
Takami M, Fujiwara R, Kijima Y, et al. Techniques for reducing air bubble intrusion into the left atrium during radiofrequency catheter and cryoballoon ablation procedures: an ex vivo study with a high-resolution camera. Heart Rhythm. 2018;16(1):128–139.
Tokuda M, Matsuo S, Kato M, Sato H, Oseto H, Okajima E, et al. Effect of air removal with extracorporeal balloon inflation on incidence of asymptomatic cerebral embolism during cryoballoon ablation of atrial fibrillation. Heart Rhythm. 2017;14(9):1291–6.
Livia C, Sugrue A, Witt T, Polkinghorne MD, Maor E, Kapa S, et al. Elimination of Purkinje fibers by electroporation reduces ventricular fibrillation vulnerability. J Am Heart Assoc. 2018;7(15):e009070.
Witt CM, Sugrue A, Padmanabhan D, Vaidya V, Gruba S, Rohl J, et al. Intrapulmonary vein ablation without stenosis: a novel balloon-based direct current electroporation approach. J Am Heart Assoc. 2018;7(14):e009575.
Sugrue A, Maor E, Ivorra A, Vaidya V, Witt C, Kapa S, et al. Irreversible electroporation for the treatment of cardiac arrhythmias. Expert Rev Cardiovasc Ther. 2018;16(5):349–60.
Reddy VY, Koruth J, Jais P, Petru J, Timko F, Skalsky I, et al. Ablation of atrial fibrillation with pulsed electric fields: an ultra-rapid, tissue-selective modality for cardiac ablation. JACC Clin Electrophysiol. 2018;4(8):987–95.
Wittkampf FHM, van Es R, Neven K. Electroporation and its relevance for cardiac catheter ablation. JACC Clin Electrophysiol. 2018;4(8):977–86.
DeSimone CV, Holmes DR Jr, Ebrille E, et al. Direct pulmonary vein ablation with stenosis prevention therapy. J Cardiovasc Electrophysiol. 2015;26(9):1000–6.
Lim B, Venkatachalam KL, Jahangir A, Johnson SB, Asirvatham SJ. Concurrent application of charge using a novel circuit prevents heat-related coagulum formation during radiofrequency ablation. J Cardiovasc Electrophysiol. 2008;19(8):843–50.
Lim B, Venkatachalam K, Henz BD, Johnson SB, Jahangir A, Asirvatham SJ. Prevention of coagulum formation with simultaneous charge delivery in radiofrequency ablation: a canine model. JACC Clin Electrophysiol. 2016;2(2):233–41.
Igel DA, Urban JF, Kent JP, Lim B, Venkatachalam KL, Asirvatham SJ, et al. Effect of charge delivery on thromboembolism during radiofrequency ablation in canines. JACC Clin Electrophysiol. 2018;4:958–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
SJA has intellectual property rights to the device described in this manuscript. The other authors declare that they have no conflict of interest.
Ethical approval
The Mayo Clinic Animal Care and Use Committee approved this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplemental Figure 1
Increase in bubble count (arrow) after intentional loss of hood contact with the myocardium. (PNG 1255 kb)
ESM 2
(MP4 332 kb)
ESM 3
(MP4 354 kb)
ESM 4
(MP4 212 kb)
Rights and permissions
About this article
Cite this article
Sugrue, A., Vaidya, V., Yasin, O. et al. Development of a novel ablation hood to prevent systemic embolization of microbubbles and particulate emboli. J Interv Card Electrophysiol 58, 281–288 (2020). https://doi.org/10.1007/s10840-019-00595-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00595-y