Abstract
Purpose
In arrhythmogenic right ventricular cardiomyopathy (ARVC), abnormal electroanatomic mapping (EAM) areas are proportional to extent of T-wave inversion on 12-lead ECG. We aimed to evaluate local repolarization changes and their relationship to EAM substrate in ARVC.
Methods
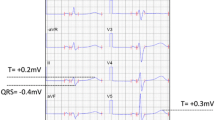
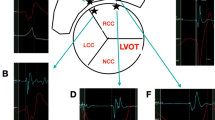
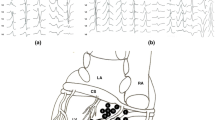
Using unipolar recordings, we analyzed the proportion of negative T waves ≥ 1 mV in depth (NegT), NegT area, Q-Tpeak (QTP), Tpeak-Tend (TPE) intervals and their relationship to bipolar (< 1.5 mV ENDO, < 1.0 mV EPI) and unipolar (< 5.5 mV) endocardial (ENDO) and epicardial (EPI) low-voltage area (LVA) in 21 pts. (15 men, mean age 39 ± 14) with ARVC. Control group included 5 pts. with normal hearts and idiopathic PVCs.
Results
On ENDO, the % of NegT (7 ± 5% vs 30 ± 20%, p = 0.004) and the NegT area (12.9 ± 9.7 c m2 vs 61.4 ± 30.0 cm2, p = 0.001) were smaller in ARVC compared to controls. On EPI, the % of NegT was similar (5 ± 7% vs 3 ± 4%, p = 0.323) and the NegT area, larger (11.0 ± 8.4 cm2 vs 2.7 ± 0.9 cm2, p = 0.027) in ARVC group. In ARVC group, the % of NegT area inside LVA was larger on EPI compared to ENDO for both bipolar (81 ± 27% vs 31 ± 33%, p < 0.001) and unipolar (90 ± 19% vs 73 ± 28%, p = 0.036) recordings. Compared to normal voltage regions, QTP inside ENDO abnormal LVA was on average 58 ± 26 ms shorter and TPE, 25 ± 56 ms longer (97 ± 26 ms and 56 ± 86 ms on EPI, respectively).
Conclusions
In ARVC, NegT areas are more closely associated with abnormal depolarization LVA on the EPI and QTP is shorter and TPE longer inside ENDO and EPI abnormal LVA compared to normal voltage regions. The results add to our understanding of ARVC arrhythmia substrate.






Similar content being viewed by others
References
Basso C, Corrado D, Marcus FI, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373(9671):1289–300.
Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the task force criteria. Circulation. 2010;121(13):1533–41.
Tanawuttiwat T, et al. Electroanatomic correlates of depolarization abnormalities in arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Cardiovasc Electrophysiol. 2016;27(4):443–52.
Zorzi A, et al. Electrocardiographic predictors of electroanatomic scar size in arrhythmogenic right ventricular cardiomyopathy: implications for arrhythmic risk stratification. J Cardiovasc Electrophysiol. 2013;24(12):1321–7.
Santangeli P, Marchlinski FE. Substrate mapping for unstable ventricular tachycardia. Heart Rhythm. 2016;13(2):569–83.
Higuchi T, Nakaya Y. T wave polarity related to the repolarization process of epicardial and endocardial ventricular surfaces. Am Heart J. 1984;108(2):290–5.
Arteyeva NV, Azarov JE. The role of transmural repolarization gradient in the inversion of cardiac electric field: model study of ECG in hypothermia. Ann Noninvasive Electrocardiol. 2017;22(1).
Antzelevitch C, Fish J. Electrical heterogeneity within the ventricular wall. Basic Res Cardiol. 2001;96(6):517–27.
Chauhan VS, Downar E, Nanthakumar K, Parker JD, Ross HJ, Chan W, et al. Increased ventricular repolarization heterogeneity in patients with ventricular arrhythmia vulnerability and cardiomyopathy: a human in vivo study. Am J Physiol Heart Circ Physiol. 2006;290(1):H79–86.
Kubala M, Pathak RK, Xie S, Casado Arroyo R, Tschabrunn CM, Hayashi T, et al. Electrocardiographic repolarization abnormalities and electroanatomic substrate in arrhythmogenic right ventricular cardiomyopathy. Circ Arrhythm Electrophysiol. 2018;11(3):e005553. https://doi.org/10.1161/CIRCEP.117.005553.
Ghanem RN, Burnes JE, Waldo AL, Rudy Y. Imaging dispersion of myocardial repolarization, II: noninvasive reconstruction of epicardial measures. Circulation. 2001;104(11):1306–12.
Opthof T, Coronel R, Wilms-Schopman FJG, Plotnikov AN, Shlapakova IN, Danilo P Jr, et al. Dispersion of repolarization in canine ventricle and the electrocardiographic T wave: Tp-e interval does not reflect transmural dispersion. Heart Rhythm. 2007;4(3):341–8.
Xia Y, Liang Y, Kongstad O, Holm M, Olsson B, Yuan S. Tpeak-tend interval as an index of global dispersion of ventricular repolarization: evaluations using monophasic action potential mapping of the epi- and endocardium in swine. J Interv Card Electrophysiol. 2005;14(2):79–87.
Zabel M, Portnoy S, Franz MR. Electrocardiographic indexes of dispersion of ventricular repolarization: an isolated heart validation study. J Am Coll Cardiol. 1995;25(3):746–52.
Zabel M, et al. Comparison of ECG variables of dispersion of ventricular repolarization with direct myocardial repolarization measurements in the human heart. J Cardiovasc Electrophysiol. 1998;9(12):1279–84.
Taggart P, et al. Transmural repolarisation in the left ventricle in humans during normoxia and ischaemia. Cardiovasc Res. 2001;50(3):454–62.
Brugada J, Pappone C, Berruezo A, Vicedomini G, Manguso F, Ciconte G, et al. Brugada syndrome phenotype elimination by epicardial substrate ablation. Circ Arrhythm Electrophysiol. 2015;8(6):1373–81.
Garcia FC, Bazan V, Zado ES, Ren JF, Marchlinski FE. Epicardial substrate and outcome with epicardial ablation of ventricular tachycardia in arrhythmogenic right ventricular cardiomyopathy/dysplasia. Circulation. 2009;120(5):366–75.
Tschabrunn CM, Marchlinski FE. Ventricular tachycardia mapping and ablation in arrhythmogenic right ventricular cardiomyopathy/dysplasia: lessons learned. World J Cardiol. 2014;6(9):959–67.
Riley MP, Zado E, Bala R, Callans DJ, Cooper J, Dixit S, et al. Lack of uniform progression of endocardial scar in patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy and ventricular tachycardia. Circ Arrhythm Electrophysiol. 2010;3(4):332–8.
Sosa E, et al. A new technique to perform epicardial mapping in the electrophysiology laboratory. J Cardiovasc Electrophysiol. 1996;7(6):531–6.
Cano O, Hutchinson M, Lin D, Garcia F, Zado E, Bala R, et al. Electroanatomic substrate and ablation outcome for suspected epicardial ventricular tachycardia in left ventricular nonischemic cardiomyopathy. J Am Coll Cardiol. 2009;54(9):799–808.
Campos B, Jauregui ME, Park KM, Mountantonakis SE, Gerstenfeld EP, Haqqani H, et al. New unipolar electrogram criteria to identify irreversibility of nonischemic left ventricular cardiomyopathy. J Am Coll Cardiol. 2012;60(21):2194–204.
Van Herendael H, et al. Idiopathic right ventricular arrhythmias not arising from the outflow tract: prevalence, electrocardiographic characteristics, and outcome of catheter ablation. Heart Rhythm. 2011;8(4):511–8.
Janse MJ, Coronel R, Opthof T. Counterpoint: M cells do not have a functional role in the ventricular myocardium of the intact heart. Heart Rhythm. 2011;8(6):934–7.
Taccardi B, Punske BB, Sachse F, Tricoche X, Colli-Franzone P, Pavarino LF, et al. Intramural activation and repolarization sequences in canine ventricles. Experimental and simulation studies. J Electrocardiol. 2005;38(4 Suppl):131–7.
Janse MJ, Coronel R, Opthof T, Sosunov EA, Anyukhovsky EP, Rosen MR. Repolarization gradients in the intact heart: transmural or apico-basal? Prog Biophys Mol Biol. 2012;109(1–2):6–15.
Ramanathan C, Jia P, Ghanem R, Ryu K, Rudy Y. Activation and repolarization of the normal human heart under complete physiological conditions. Proc Natl Acad Sci U S A. 2006;103(16):6309–14.
Cowan JC, Hilton CJ, Griffiths CJ, Tansuphaswadikul S, Bourke JP, Murray A, et al. Sequence of epicardial repolarisation and configuration of the T wave. Br Heart J. 1988;60(5):424–33.
Castro Hevia J, Antzelevitch C, Tornés Bárzaga F, Dorantes Sánchez M, Dorticós Balea F, Zayas Molina R, et al. Tpeak-Tend and Tpeak-Tend dispersion as risk factors for ventricular tachycardia/ventricular fibrillation in patients with the Brugada syndrome. J Am Coll Cardiol. 2006;47(9):1828–34.
Lubinski A, et al. The terminal portion of the T wave: a new electrocardiographic marker of risk of ventricular arrhythmias. Pacing Clin Electrophysiol. 2000;23(11 Pt 2):1957–9.
Smetana P, Schmidt A, Zabel M, Hnatkova K, Franz M, Huber K, et al. Assessment of repolarization heterogeneity for prediction of mortality in cardiovascular disease: peak to the end of the T wave interval and nondipolar repolarization components. J Electrocardiol. 2011;44(3):301–8.
Yan GX, Antzelevitch C. Cellular basis for the Brugada syndrome and other mechanisms of arrhythmogenesis associated with ST-segment elevation. Circulation. 1999;100(15):1660–6.
Funding
This study is funded in part by the F Harlan Batrus EP Research Fund, Katherine M. Miller Research Fund, and the Winkelman Family Fund in Cardiovascular Innovation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kubala, M., Xie, S., Santangeli, P. et al. Analysis of local ventricular repolarization using unipolar recordings in patients with arrhythmogenic right ventricular cardiomyopathy. J Interv Card Electrophysiol 57, 261–270 (2020). https://doi.org/10.1007/s10840-019-00594-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-019-00594-z