Abstract
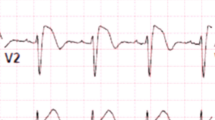
Right bundle branch block is relatively frequent in the general population and is generally considered benign in healthy individuals. However, it has been associated with increased cardiovascular risk and all-cause mortality in various cohort studies. Indeed, the presence of right bundle branch block in subjects affected by cardiomyopathies or channelopathies is not rare and may conceal underlying electrocardiographic changes, thus making the diagnosis of such conditions more challenging. The purpose of this review is to analyze the prevalence and clinical significance of right bundle branch block in subjects affected by Brugada syndrome and arrhythmogenic right ventricular cardiomyopathy.

Similar content being viewed by others
Abbreviations
- AC:
-
Arrhythmogenic cardiomyopathy
- BrS:
-
Brugada syndrome
- CMR:
-
Cardiac magnetic resonance
- CRBBB:
-
Complete right bundle branch block
- ECG:
-
Electrocardiogram
- IRBBB:
-
Incomplete RBBB
- IVF:
-
Idiopathic ventricular fibrillation
- LV:
-
Left ventricle
- RV:
-
Right ventricular
- RVOT:
-
Right ventricular outflow tract
- SAECG:
-
Signal averaged ECG
- SCB:
-
Sodium channel blocker
- TAD:
-
Terminal activation delay
- TWI:
-
T wave inversion
- SCD:
-
Sudden cardiac death
References
Surawicz B, Childers R, Deal BJ, Gettes LS, Bailey JJ, Gorgels A, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram part III: intraventricular conduction disturbances. J Am Coll Cardiol. 2009;53:976–8.
Eriksson P, Wilhelmsen L, Rosengren A. Bundle-branch block in middle-aged men: risk of complications and death over 28 years: the primary prevention study in Goteborg, Sweden. Eur Heart J. 2005;26:2300–6.
Jeong JH, Kim JH, Park YH, Han DC, Hwang KW, Lee DW, et al. Incidence of and risk factors for bundle branch block in adults older than 40 years. Korean J Intern Med. 2004;19:171–8.
Fahy GJ, Pinski SL, Miller DP, McCabe N, Pye C, Walsh MJ, et al. Natural history of isolated bundle branch block. Am J Cardiol. 1996;77:1185–90.
Bussink BE, Holst AG, Jespersen L, Deckers JW, Jensen GB, Prescott E. Right bundle branch block: prevalence, risk factors, and outcome in the general population: results from the Copenhagen City Heart Study. Eur Heart J. 2013;34:138–46.
Aizawa Y, Takatsuki S, Kimura T, Nishiyama N, Fukumoto K, Tanimoto Y, et al. Ventricular fibrillation associated with complete right bundle branch block. Heart Rhythm. 2013;10:1028–35.
Horowitz LN, Alexander JA, Edmunds LH Jr. Postoperative right bundle branch block: identification of three levels of block. Circulation. 1980;62:319–28.
Windham CRC. Epicardial activation in bundle branch block. Pacing Clin Electrophysiol. 1983;6:1201–9.
Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391–6.
Brugada J, Brugada R, Brugada P. Right bundle-branch block and ST-segment elevation in leads V1 through V3: a marker for sudden death in patients without demonstrable structural heart disease. Circulation. 1998;97:457–60.
Ohkubo K, Watanabe I, Okumura Y, Ashino S, Kofune M, Nagashima K, et al. A new criteria differentiating type 2 and 3 Brugada patterns from ordinary incomplete right bundle branch block. Int Heart J. 2011;52:159–63.
Aizawa Y, Kimura T, Takatsuki S. A case of Brugada syndrome showing augmentation of electrocardiogram phenotype by complete right bundle branch block. Europace. 2013;15:1525.
Chiale PA, Garro HA, Fernandez PA, et al. High-degree right bundle branch block obscuring the diagnosis of Brugada electrocardiographic pattern. Heart Rhythm. 2012;9:974–6.
Tomita M, Kitazawa H, Sato M, Okabe M, Antzelevitch C, Aizawa Y. A complete right bundle-branch block masking Brugada syndrome. J Electrocardiol. 2012;45:780–2.
Wada T, Nagase S, Morita H, Nakagawa K, Nishii N, Nakamura K, et al. Incidence and clinical significance of Brugada syndrome masked by complete right bundle-branch block. Circ J. 2015;79:2568–75.
Maury P, Rollin A, Sacher F, Gourraud JB, Raczka F, Pasquié JL, et al. Prevalence and prognostic role of various conduction disturbances in patients with the Brugada syndrome. Am J Cardiol. 2013;112:1384–9.
Yamawake N, Nishizaki M, Shimizu M, Fujii H, Sakurada H, Hiraoka M. Unmasking Brugada-type electrocardiogram on deep inspiration. Circ J. 2014;78:360–5.
Oreto G, Corrado D, Delise P, et al. Doubts of the cardiologist regarding an electrocardiogram presenting QRS V1-V2 complexes with positive terminal wave and ST segment elevation. Consensus Conference promoted by the Italian Cardiology Society. G Ital Cardiol. 2010;11(Suppl 2):3S–22S.
Peréz-Riera AR, Filho CF, de Abreu LC, et al. Do patients with electrocardiographic Brugada type 1 pattern have associated right bundle branch block? A comparative vectorcardiographic study. Europace. 2015;14:889–97.
Bayés de Luna A. Clinical electrocardiography: a textbook. 2nd ed. New York: Futura; 1999.
Corrado D, Basso C, Buja G, Nava A, Rossi L, Thiene G. Right bundle branch block, right precordial ST-segment elevation, and sudden death in young people. Circulation. 2001;103:710–7.
Coronel R, Casini S, Koopmann TT, Wilms-Schopman FJ, Verkerk AO, de Groot JR, et al. Right ventricular fibrosis and conduction delay in a patient with clinical signs of Brugada syndrome: a combined electrophysiological, genetic, histopathologic, and computational study. Circulation. 2005;112:2769–77.
Nagase S, Kusano KF, Morita H, Fujimoto Y, Kakishita M, Nakamura K, et al. Epicardial electrogram of the right ventricular outflow tract in patients with the Brugada syndrome: using the epicardial lead. J Am Coll Cardiol. 2002;39:1992–5.
Postema PG, van Dessel PF, de Bakker JM, et al. Slow and discontinuous conduction conspire in Brugada syndrome: a right ventricular mapping and stimulation study. Circ Arrhythm Electrophysiol. 2008;1:379–86.
Postema PG, van Dessel PF, Kors JA, Linnenbank AC, van Herpen G, Ritsema van Eck H, et al. Local depolarization abnormalities are the dominant pathophysiologic mechanism for type 1 electrocardiogram in Brugada syndrome a study of electrocardiograms, vectorcardiograms, and body surface potential maps during ajmaline provocation. J Am Coll Cardiol. 2010;55:789–97.
Lambiase PD, Ahmed AK, Ciaccio EJ, Brugada R, Lizotte E, Chaubey S, et al. High-density substrate mapping in Brugada syndrome: combined role of conduction and repolarization heterogeneities in arrhythmogenesis. Circulation. 2009;120:106–17.
Doi A, Takagi M, Maeda K, Tatsumi H, Shimeno K, Yoshiyama M. Conduction delay in right ventricle as a marker for identifying high-risk patients with Brugada syndrome. J Cardiovasc Electrophysiol. 2010;21:688–96.
Kanda M, Shimizu W, Matsuo K, Nagaya N, Taguchi A, Suyama K, et al. Electrophysiologic characteristics and implications of induced ventricular fibrillation in symptomatic patients with Brugada syndrome. J Am Coll Cardiol. 2002;39:1799–805.
Nademanee K, Veerakul G, Chandanamattha P, Chaothawee L, Ariyachaipanich A, Jirasirirojanakorn K, et al. Prevention of ventricular fibrillation episodes in Brugada syndrome by catheter ablation over the anterior right ventricular outflow tract epicardium. Circulation. 2011;123:1270–9.
Martini B, Nava A, Thiene G, Buja GF, Canciani B, Scognamiglio R, et al. Ventricular fibrillation without apparent heart disease: description of six cases. Am Heart J. 1989;118:1203–9.
van Veen TA, Stein M, Royer A, le Quang K, Charpentier F, Colledge WH, et al. Impaired impulse propagation in scn5a-knockout mice: combined contribution of excitability, connexin expression, and tissue architecture in relation to aging. Circulation. 2005;112:1927–35.
Nademanee K, Raju H, de Noronha SV, Papadakis M, Robinson L, Rothery S, et al. Fibrosis, connexin-43, and conduction abnormalities in the Brugada syndrome. J Am Coll Cardiol. 2015;66:1976–86.
Zhang J, Sacher F, Hoffmayer K, O'Hara T, Strom M, Cuculich P, et al. Cardiac electrophysiological substrate underlying the ECG phenotype and electrogram abnormalities in Brugada syndrome patients. Circulation. 2015;131:1950–9.
Calo’ L, Giustetto C, Martino A, et al. A new electrocardiographic marker of sudden death in Brugada syndrome: the S-wave in lead I. J Am Coll Cardiol. 2016;67:1427–40.
Basso C, Corrado D, Marcus FI, Nava A, Thiene G. Arrhythmogenic right ventricular cardiomyopathy. Lancet. 2009;373:1289–300.
Sen-Chowdhry S, Syrris P, Prasad SK, Hughes SE, Merrifield R, Ward D, et al. Left-dominant arrhythmogenic cardiomyopathy: an underrecognized clinical entity. J Am Coll Cardiol. 2008;52:2175–87.
Te Riele AS, James CA, Bhonsale A, et al. Malignant arrhythmogenic right ventricular dysplasia/cardiomyopathy with a normal 12-lead electrocardiogram: a rare but underrecognized clinical entity. Heart Rhythm. 2013;10:1484–91.
Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia. Proposed modification of the task force criteria. Circulation. 2010;121:1533–41.
Nunes de Alencar Neto J, Baranchuk A, Bayès-Genìs A, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy: an electrocardiogram-based review. Europace. 2017;0:1–10. https://doi.org/10.1093/europace/eux202.
Durrer D, Van Dam THR, Freud GE, et al. Total excitation of the isolated human heart. Circulation. 1970;16:899–912.
Cox MG, Nelen MR, Wilde AA, et al. Activation delay and VT parameters in arrhythmogenic right ventricular dysplasia/cardiomyopathy: toward improvement of diagnostic ECG criteria. J Cardiovasc Electrophysiol. 2008;19:775–81.
Peters S, Trummel M. Diagnosis of arrhythmogenic right ventricular dysplasia-cardiomyopathy: value of standard ECG revisited. Ann Noninvasive Electrocardiol. 2003;8:238–45.
Peters S, Trummel M, Koehler B. QRS fragmentation in standard ECG as a diagnostic marker of arrhythmogenic right ventricular dysplasia-cardiomyopathy. Heart Rhythm. 2008;5:1417–21.
Peters S, Trummel M, Koehler B. Special features of right bundle branch block in patients with arrhythmogenic right ventricular cardiomyopathy/dysplasia. Int J Cardiol. 2012;157:102–3.
Fontaine G, Fontaliran F, Hebert JL, et al. Arrhythmogenic right ventricular dysplasia. Annu Rev Med. 1999;50:17–35.
Jain R, Dalal D, Daly A, Tichnell C, James C, Evenson A, et al. Electrocardiographic features of arrhythmogenic right ventricular dysplasia. Circulation. 2009;120:477–87.
Peters S. QRS fragmentation in patients with arrhythmogenic right ventricular cardiomyopathy and complete right bundle branch block: a risk stratification. Eur Heart J Acute Cardiovasc Care. 2012;1:236–9.
Tanawuttiwat T, Te Riele AS, Philips B, et al. Electroanatomic correlates of depolarization abnormalities in arrhythmogenic right ventricular dysplasia/cardiomyopathy. J Cardiovasc Electrophysiol. 2016;27:443–52.
Kawasuji M, Iwa T. Spread of the epicardial excitation in right bundle branch block pattern. Jpn Circ J. 1978;42:1041–56.
Acknowledgements
We thank Margaret Knowles for the review of the English language.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Calò, L., Martino, A., Goanta, E. et al. Right bundle branch block and conduction disturbances in Brugada syndrome and arrhythmogenic right ventricular cardiomyopathy. J Interv Card Electrophysiol 52, 307–313 (2018). https://doi.org/10.1007/s10840-018-0386-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-018-0386-3