Abstract
Purpose
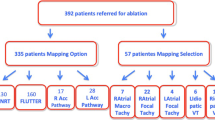
Audit has played a key role in monitoring and improving clinical practice. However, audit often fails to drive change as summative institutional data alone may be insufficient to do so. We hypothesised that the practice of attributed audit, wherein each individual’s procedural performance is presented will have a greater impact on clinical practice. This hypothesis was tested in an observational study evaluating improvement in fluoroscopy times for AF ablation.
Methods
Retrospective analyses of fluoroscopy times in AF ablations at the Barts Heart Centre (BHC) from 2012–2017. Fluoroscopy times were compared pre- and post- the introduction of attributed audit in 2012 at St Bartholomew’s Hospital (SBH). In order to test the hypothesis, this concept was introduced to a second group of experienced operators from the Heart Hospital (HH) as part of a merger of the two institutions in 2015 and change in fluoroscopy times recorded.
Results
A significant drop in fluoroscopy times (33.3 ± 9.14 to 8.95 ± 2.50, p < 0.0001) from 2012-2014 was noted after the introduction of attributed audit. At the time of merger, a significant difference in fluoroscopy times between operators from the two centres was seen in 2015. Each operator’s procedural performance was shared openly at the audit meeting. Subsequent audits showed a steady decrease in fluoroscopy times for each operator with the fluoroscopy time (min, mean±SD) decreasing from 13.29 ± 7.3 in 2015 to 8.84 ± 4.8 (p < 0.0001) in 2017 across the entire group.
Conclusions
Systematic improvement in fluoroscopy times for AF ablation procedures was noted byevaluating individual operators’ performance. Attributing data to physicians in attributed audit can promptsignificant improvement and hence should be adopted in clinical practice.


Similar content being viewed by others
References
Calkins H, et al. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012;14(4):528–06.
Ivers N, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259.
Paton JY, Ranmal R, Dudley J, RCPCH clinical standards committee. Clinical audit: still an important tool for improving healthcare. Arch Dis Child Educ Pract Ed. 2015;100(2):83–8.
Erasmus RT, Zemlin AE. Clinical audit in the laboratory. J Clin Pathol. 2009 Jul;62(7):593–7.
Shaw CD. Measuring against clinical standards. Clin Chim Acta. 2003;333:115–24.
Surgical Outcomes – Royal College of Surgeons. https://www.rcseng.ac.uk/patient-care/surgical-staff-and.../surgical-outcomes/. Accessed Online 10th September 2017.
Spurgeon P, Barwell F, Mazelan P. Developing a medical engagement scale (MES). Int J Clin Leadership. 2008;16:213–23.
Atkinson S, et al. Engaging doctors: what can we learn from trusts with high levels of medical engagement? UK: NHS Institute for Innovation and Improvement and Academy of Medical Royal Colleges; 2011.
Cameron M, Penney G, MacLennan G, McLeer S, Walker A. Impact on maternity professionals of novel approaches to clinical audit feedback. Eval Health Prof. 2007;30(1):75–95.
Acknowledgements
We wish to acknowledge the enormous contribution of David Bays, who helped develop our electronic AF ablation registry and helped with organising data collection. The registry played a central role in testing the hypothesis of the present study.
Contributorship
VS: data collection, data analyses, manuscript draft and preparation; EV: data collection, MS: data collection; FK: manuscript review; OS: manuscript review; SA: manuscript review; AC: manuscript review; VE: manuscript review; MF: manuscript review; PL: manuscript review; ML: manuscript review; MD: manuscript review; SS: manuscript review; MJE: manuscript review; RH: supervised data collection, manuscript review; RJS: study concept and design, initiated open audit in trust, supervised data collection and manuscript draft, manuscript review
Funding
Cost-neutral study
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Sawhney, V., Volkova, E., Shaukat, M. et al. Impact of attributed audit on procedural performance in cardiac electrophysiology catheter laboratory. J Interv Card Electrophysiol 56, 199–203 (2019). https://doi.org/10.1007/s10840-018-0383-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-018-0383-6