Abstract
Purpose
Protected channels of surviving myocytes in late postinfarction ventricular scar predispose to ventricular tachycardia (VT). However, only a few patients develop VT spontaneously. We studied differences in electric remodeling and protected channels in late postinfarction patients with and without spontaneous VT.
Methods
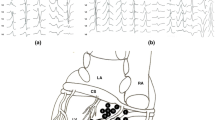
Patients with ischemic cardiomyopathy (ICM) with recurrent sustained monomorphic VT (n = 22) were compared with stable ICM patients without spontaneous VT (control group; n = 5). Left ventricular mapping was performed with a 20-pole catheter. Detailed pace mapping was used to identify channels of protected conduction, and confirmed, when feasible, by entrainment. Anatomical and electrophysiological properties of VT channels and non-VT channels in VT patients and channels in controls were evaluated.
Results
Seventy-three (median 3) VTs were inducible in VT patients compared to two (median 0) in controls. The VT channels in VT patients (n = 57, 3 ± 1 per patient) were lengthier (mean ± SEM 53 ± 5 vs. 33 ± 4 vs. 24 ± 8 mm), had longer S-QRS (73 ± 4 vs. 63 ± 3 vs. 44 ± 8 ms), longer conduction time (103 ± 13 vs. 33 ± 4 vs. 24 ± 8 ms), and slower conduction velocity (CV) (0.85 ± 0.21 vs. 1.39 ± 0.20 vs. 1.31 ± 0.41 m/s) than non-VT channels in VT patients (n = 183, 8 ± 6 per patient) (p ≤ 0.01) and channels in controls (n = 46, 9 ± 8 per patient) (p ≤ 0.01). Additionally, non-VT channels in VT patients had longer S-QRS (p = 0.02); however, they were similar in length, conduction time, and CV compared to channels in controls.
Conclusions
Channels supporting VT are lengthier, with longer conduction times and slower CV compared to channels in patients without spontaneous VT. These observations may explain why some ICM patients have spontaneous VT and others do not.



Similar content being viewed by others
References
Wissner E, Stevenson WG, Kuck KH. Catheter ablation of ventricular tachycardia in ischaemic and non-ischaemic cardiomyopathy: where are we today? A clinical review. Eur Heart J. 2012;33(12):1440–50. https://doi.org/10.1093/eurheartj/ehs007.
de Bakker JMT, van Capelle F, Janse M, Tasseron S, Vermeulen J, de Jonge N, et al. Slow conduction in the infarcted human heart. ‘Zigzag’ course of activation. Circulation. 1993;88(3):915–26. https://doi.org/10.1161/01.CIR.88.3.915.
Cassidy D, Vassallo J, Miller J, Poll D, Buxton A, Marchlinski F, et al. Endocardial catheter mapping during sinus rhythm: relation of underlying heart disease and ventricular arrhythmia. Circulation. 1986;73(4):645–52. https://doi.org/10.1161/01.CIR.73.4.645.
Haqqani HM, Kalman JM, Roberts-Thomson KC, Balasubramaniam RN, Rosso R, Snowdon RL, et al. Fundamental differences in electrophysiologic and electroanatomic substrate between ischemic cardiomyopathy patients with and without clinical ventricular tachycardia. J Am Coll Cardiol. 2009;54(2):166–73. https://doi.org/10.1016/j.jacc.2009.04.024.
Nayyar S, Wilson L, Ganesan AN, Sullivan T, Kuklik P, Chapman D, et al. High-density mapping of ventricular scar: a comparison of ventricular tachycardia (VT) supporting channels with channels that do not support VT. Circ Arrhythm Electrophysiol. 2014;7(1):90–8. https://doi.org/10.1161/CIRCEP.113.000882.
Epstein AE, Dimarco JP, Ellenbogen KA, Estes NA III, Freedman RA, Gettes LS, et al. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary. Heart Rhythm. 2008;5(6):934–55. https://doi.org/10.1016/j.hrthm.2008.04.015.
Josephson M. Clinical cardiac electrophysiology: techniques and interpretations. Philadelphia: Lippincott Williams & Wilkins; 2002. p. 425–610.
Marchlinski FE, Callans DJ, Gottlieb CD, Zado E. Linear ablation lesions for control of unmappable ventricular tachycardia in patients with ischemic and nonischemic cardiomyopathy. Circulation. 2000;101(11):1288–96. https://doi.org/10.1161/01.CIR.101.11.1288.
Bogun F, Good E, Reich S, Elmouchi D, Igic P, Lemola K, et al. Isolated potentials during sinus rhythm and pace-mapping within scars as guides for ablation of post-infarction ventricular tachycardia. J Am Coll Cardiol. 2006;47(10):2013–9. https://doi.org/10.1016/j.jacc.2005.12.062.
Brunckhorst CB, Stevenson WG, Soejima K, Maisel WH, Delacretaz E, Friedman PL, et al. Relationship of slow conduction detected by pace-mapping to ventricular tachycardia re-entry circuit sites after infarction. J Am Coll Cardiol. 2003;41(5):802–9. https://doi.org/10.1016/S0735-1097(02)02932-7.
Stevenson WG, Sager PT, Natterson PD, Saxon LA, Middlekauff HR, Wiener I. Relation of pace mapping QRS configuration and conduction delay to ventricular tachycardia reentry circuits in human infarct scars. J Am Coll Cardiol. 1995;26(2):481–8. https://doi.org/10.1016/0735-1097(95)80026-D.
de Chillou C, Groben L, Magnin-Poull I, Andronache M, MagdiAbbas M, Zhang N, et al. Localizing the critical isthmus of postinfarct ventricular tachycardia: the value of pace-mapping during sinus rhythm. Heart Rhythm. 2014;11(2):175–81. https://doi.org/10.1016/j.hrthm.2013.10.042.
de Bakker J, van Capelle F, Janse M, Wilde A, Coronel R, Becker A, et al. Reentry as a cause of ventricular tachycardia in patients with chronic ischemic heart disease: electrophysiologic and anatomic correlation. Circulation. 1988;77(3):589–606. https://doi.org/10.1161/01.CIR.77.3.589.
de Bakker JM, Coronel R, Tasseron S, Wilde AA, Opthof T, Janse MJ, et al. Ventricular tachycardia in the infarcted, Langendorff-perfused human heart: role of the arrangement of surviving cardiac fibers. J Am Coll Cardiol. 1990;15(7):1594–607. https://doi.org/10.1016/0735-1097(90)92832-M.
Anter E, Tschabrunn CM, Buxton AE, Josephson ME. High-resolution mapping of postinfarction reentrant ventricular tachycardia: electrophysiological characterization of the circuit. Circulation. 2016;134(4):314–27. https://doi.org/10.1161/CIRCULATIONAHA.116.021955.
Dillon SM, Allessie MA, Ursell PC, Wit AL. Influences of anisotropic tissue structure on reentrant circuits in the epicardial border zone of subacute canine infarcts. Circ Res. 1988;63(1):182–206. https://doi.org/10.1161/01.RES.63.1.182.
Ding C, Gepstein L, Nguyen DT, Wilson E, Hulley G, Beaser A, et al. High-resolution optical mapping of ventricular tachycardia in rats with chronic myocardial infarction. Pacing Clin Electrophysiol. 2010;33(6):687–95. https://doi.org/10.1111/j.1540-8159.2010.02704.x.
Hsia H, Lin D, Sauer W, Callans D, Marchlinski F. Anatomic characterization of endocardial substrate for hemodynamically stable reentrant ventricular tachycardia: identification of endocardial conducting channels. Heart Rhythm. 2006;3(5):503–12. https://doi.org/10.1016/j.hrthm.2006.01.015.
de Chillou C, Lacroix D, Klug D, Magnin-Poull I, Marquie C, Messier M, et al. Isthmus characteristics of reentrant ventricular tachycardia after myocardial infarction. Circulation. 2002;105(6):726–31. https://doi.org/10.1161/hc0602.103675.
Nayyar S, Kuklik P, Ganesan AN, Sullivan TR, Wilson L, Young GD, et al. Development of time- and voltage-domain mapping (V-T-mapping) to localize ventricular tachycardia channels during sinus rhythm. Circ Arrhythm Electrophysiol. 2016;9(12):e004050. https://doi.org/10.1161/CIRCEP.116.004050.
Brunckhorst CB, Delacretaz E, Soejima K, Maisel WH, Friedman PL, Stevenson WG. Identification of the ventricular tachycardia isthmus after infarction by pace mapping. Circulation. 2004;110(6):652–9. https://doi.org/10.1161/01.CIR.0000138107.11518.AF.
Wiener I, Mindich B, Pitchon R. Determinants of ventricular tachycardia in patients with ventricular aneurysms: results of intraoperative epicardial and endocardial mapping. Circulation. 1982;65(5):856–61. https://doi.org/10.1161/01.CIR.65.5.856.
Bogun F, Bahu M, Knight BP, Weiss R, Goyal R, Daoud E, et al. Response to pacing at sites of isolated diastolic potentials during ventricular tachycardia in patients with previous myocardial infarction. J Am Coll Cardiol. 1997;30(2):505–13. https://doi.org/10.1016/S0735-1097(97)00177-0.
Tschabrunn CM, Roujol S, Dorman NC, Nezafat R, Josephson ME, Anter E. High-resolution mapping of ventricular scar: comparison between single and multielectrode catheters. Circ Arrhythm Electrophysiol. 2016;9(6):e003841. https://doi.org/10.1161/CIRCEP.115.003841.
Cabo C, Pertsov AM, Baxter WT, Davidenko JM, Gray RA, Jalife J. Wave-front curvature as a cause of slow conduction and block in isolated cardiac muscle. Circ Res. 1994;75(6):1014–28. https://doi.org/10.1161/01.RES.75.6.1014.
Roy D, Marchand E, Theroux P, Waters DD, Pelletier GB, Cartier R, et al. Long-term reproducibility and significance of provokable ventricular arrhythmias after myocardial infarction. J Am Coll Cardiol. 1986;8(1):32–9. https://doi.org/10.1016/S0735-1097(86)80088-2.
Nayyar S, Kuklik P, Suszko A, Chauhan VS. Evoked intra-QRS and post-QRS potentials predict freedom from ventricular arrhythmias: a detailed body surface ECG analysis of cardiomyopathy patients. Heart Rhythm. 2017;14:s539.
Stevenson WG, Soejima K. Catheter ablation for ventricular tachycardia. Circulation. 2007;115(21):2750–60. https://doi.org/10.1161/CIRCULATIONAHA.106.655720.
Leshem E, Tschabrunn CM, Jihye J, Whitaker J, Israel Z, Beeckler C, et al. High-resolution mapping of ventricular scar—evaluation of a novel integrated multielectrode mapping and ablation catheter. J Am Coll Cardiol EP. 2017;3:220–31.
Funding
This work was supported by the Robert J. Craig Electrophysiology Scholarship from the University of Adelaide (S.N), the National Heart Foundation of Australia (A.G., P.K., K.R-T., P.S.), Early Career Health Practitioner Fellowship from the National Health and Medical Research Council of Australia (A.G.), the Practitioner Fellowship from the National Health and Medical Research Council of Australia (P.S.), and the Sylvia & Charles Viertel Foundation Australia (K.R-T.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Roberts-Thomson reports having served on the advisory board of St Jude Medical. Dr. Sanders reports having served on the advisory board of Biosense-Webster, Medtronic, CathRx, and St Jude Medical; received lecture and/or consulting fees from Biosense-Webster, Medtronic, St Jude Medical, and Boston Scientific; and received research funding from Medtronic, St Jude Medical, Boston Scientific, Biotronik, and Sorin.
Rights and permissions
About this article
Cite this article
Nayyar, S., Wilson, L., Ganesan, A. et al. Electrophysiologic features of protected channels in late postinfarction patients with and without spontaneous ventricular tachycardia. J Interv Card Electrophysiol 51, 13–24 (2018). https://doi.org/10.1007/s10840-017-0299-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-017-0299-6