Abstract
Purpose
Despite novel left ventricular (LV) lead technologies, phrenic nerve stimulation (PNS) remains an adverse effect observed in many patients with cardiac resynchronization therapy (CRT). Beyond anatomic repositioning, modern CRT devices allow avoidance of PNS also by software-based adaption of the pacing configuration. The Electronic Repositioning With Acuity and Easytrak Leads study evaluated the incidence of PNS in a CRT population and examined how often LV lead relocation can be avoided by “electronic repositioning” (ER).
Methods
Patients who had an indication for implantation of a first CRT defibrillator with the option of ER were enrolled. Primary endpoint was the efficiency of ER determined by the frequency of PNS with the standard pacing configuration (LV tip to RV coil) avoidable by ER. PNS and pacing parameters were evaluated during implant, predischarge, and first routine follow-up (FU) using four different pacing configurations available by ER.
Results
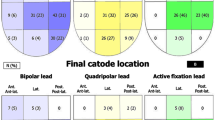
In total, 292 patients were enrolled and provided with a transvenous LV lead (82.2 % male, 65.5 ± 9.2 years old). The majority of the population was in NYHA III (84.2 %) with a LV ejection fraction of 25.3 ± 6.8 % and mean QRS width of 155 ± 27 ms, ischemic cardiomyopathy was present in 43.6 %. Median FU was 116 days. In the standard pacing configuration, PNS was inducible in 19.0/25.6/24.6 % at implant/predischarge/FU, respectively, resulting in 32.2 % of the patients presenting at least once with PNS. The safety margin for the standard pacing configuration between LV and PNS threshold was <1.0 V at 0.5 ms in 5.6/7.0/5.0 % of the patients, corresponding with a total rate of 11.6 % during the FU. In the finally chosen configuration, clinically relevant PNS occurred in 1.0/2.2/1.3 %. The four vector configurations allowed all but 6 of 292 (2 %) patients to be reprogrammed using ER without reoperation.
Conclusions
The incidence of inducible PNS in CRT patients is considerable. In this study, PNS could be avoided in the majority of the patients by means of electronic repositioning. Thus, the use of ER should be considered for CRT patients.


Similar content being viewed by others
References
Dickstein, K., Vardas, P. E., Auricchio, A., Daubert, J. C., Linde, C., McMurray, J., et al. (2010). 2010 Focused Update of ESC Guidelines on device therapy in heart failure. European Heart Journal, 31, 2677–2687.
Jessup, M., Abraham, W. T., Casey, D. E., Feldman, A. M., Francis, G. S., Ganiats, T. G., et al. (2009). 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation / American Heart Association Task Force on Practice Guidelines: Developed in collaboration with the International Society for Heart and Lung Transplantation. Circulation, 119, 1977–2016.
Butter, C., Auricchio, A., Stellbrink, C., Fleck, E., Ding, J., Yu, Y., et al. (2001). Effect of resynchronization therapy stimulation site on the systolic function of heart failure patients. Circulation, 104, 3026–3029.
Dekker, A. L., Phelps, B., Dijkman, B., Van Der Nagel, T., Van Der Veen, F. H., Geskes, G. G., et al. (2004). Epicardial left ventricular lead placement for cardiac resynchronization therapy: Optimal pace site selection with pressure–volume loops. The Journal of Thoracic and Cardiovascular Surgery, 127, 1641–1647.
Sanchez-Quintana, D., Cabrera, J. A., Climent, V., Farré, J., Weiglein, A., & Ho, S. Y. (2005). How close are the phrenic nerves to cardiac structures? Implications for cardiac interventionalists. Journal of Cardiovascular Electrophysiology, 16(3)), 309–313.
Alonso, C., Leclerq, C., D’Allonnes, F. R., Pavin, D., Victor, F., Mabo, P., et al. (2001). Six year experience of transvenous left ventricular lead implantation for permanent biventricular pacing in patients with advanced heart failure: Technical aspects. Heart, 86, 405–410.
Knight, B. P., Desai, A., Coman, J., Faddis, M., & Yong, P. (2004). Long-term retention of cardiac resynchronization therapy. Journal of the American College of Cardiology, 44(1), 72–77.
Gurevitz, O., Nof, E., Carasso, S., Luria, D., Bar-Lev, D., Tanami, N., et al. (2005). Programmable multiple pacing configurations help to overcome high left ventricular pacing thresholds and avoid phrenic nerve stimulation. Pacing and Clinical Electrophysiology, 28(12), 1255–1259.
Leon, A. R., Abraham, W. T., Curtis, A. B., Daubert, J. P., Fisher, W. G., Gurley, J., et al. (2005). Safety of transvenous cardiac resynchronization system implantation in patients with chronic heart failure: Combined results of over 2,000 patients from a multicenter study program. Journal of the American College of Cardiology, 46, 2348–2356.
Biffi, M., Moschini, C., Bertini, M., Saporito, D., Ziacchi, M., Diemberger, I., et al. (2009). Phrenic stimulation: A challenge for cardiac resynchronization therapy. Circ Arrhythmia Electrophysiol, 2, 402–410.
Champagne, J., Healey, J. S., Krahn, A. D., Phillipon, F., Gurevitz, O., Swearingen, A., et al. (2011). The effect of electronic repositioning on left ventricular pacing and phrenic nerve stimulation. Europace, 13(3), 409–415.
Jastrzebski, M., Bacior, B., Wojciechowska, W., & Czarnecka, D. (2011). Left ventricular lead implantation at a phrenic stimulation site is safe and effective. Europace, 13(4), 520–525.
Seifert, M., Schau, T., Moeller, V., Neuss, M., Meyhoefer, J., & Butter, C. (2010). Influence of pacing configurations, body mass index, and position of coronary sinus lead on frequency of phrenic nerve stimulation and pacing thresholds under cardiac resynchronization therapy. Europace, 12(7), 961–967.
Vaseghi, M., Cesario, D. A., Ji, S., Shannon, K. M., Wiener, I., Boyle, N. G., et al. (2005). Beyond coronary sinus angiography: The value of coronary arteriography and identification of the pericardiophrenic vein during left ventricular lead placement. PACE, 28(3), 185–190.
D'Ivernois, C., Lesage, J., & Blanc, P. (2008). Where are the left ventricular leads really implanted? A study of 90 consecutive patients. PACE, 31(5), 554–559.
Biffi, M., & Boriani, G. (2011). Phrenic stimulation management in CRT patients: Are we there yet? Current Opinion in Cardiology, 26(1), 12–16.
Biffi, M., Exner, D. V., Crossley, G. H., Ramza, B., Coutu, B., Tomassoni, G., et al. (2013). Occurrence of phrenic nerve stimulation in cardiac resynchronization therapy patients: The role of left ventricular lead type and placement site. Europace, 15, 77–82.
Biffi, M., Bertini, M., Ziacchi, M., Gardini, B., Mazzotti, A., Massaro, G., et al. (2011). Management of phrenic stimulation in CRT patients over the long term: Still an unmet need? Pacing and Clinical Electrophysiology, 34, 1201–1208.
Klein, N., Klein, M., Weglage, H., Przibille, O., Fischer, S., Trappe, H. J., et al. (2012). Clinical efficacy of left ventricular pacing vector programmability in cardiac resynchronization therapy defibrillator patients for management of phrenic nerve stimulation and/or elevated left ventricular pacing thresholds: Insights from the Efface Phrenic Stim study. Europace, 14, 826–832.
Sperzel, J., Daenschel, W., Gutleben, K. J., Kranig, W., Mortensen, P., Connelly, D., et al. (2012). First prospective, multi-centre clinical experience with a novel left ventricular quadripolar lead. Europace, 14, 365–372.
Tomassoni, G., Baker, J., Corbisiero, R., Love, C., Martin, D., Niazi, I., et al. (2013). Postoperative performance of the Quartet® left ventricular heart lead. Journal of Cardiovascular Electrophysiology, 24, 449–456.
Parahuleva, M. S., Chasan, R., Soydan, N., Abdallah, Y., Neuhof, C., Tillmanns, H., et al. (2011). Quadripolar left ventricular lead in a patient with CRT-D does not overcome phrenic nerve stimulation. Clin Med Insights Cardiol, 5, 45–47.
Biffi, M., Zanon, F., Bertaglia, E., Padeletti, L., Varbaro, A., De Santo, T., et al. (2013). Short-spaced dipole for managing phrenic nerve stimulation in patients with CRT: the "phrenic nerve mapping and stimulation EP" catheter study. Heart Rhythm, 10, 39–45.
Biffi, M., Foerster, L., Eastman, W., Eggen, M., Grenz, N. A., Sommer, J., et al. (2012). Effect of bipolar electrode spacing on phrenic nerve stimulation and left ventricular pacing thresholds: an acute canine study. Circ Arrh Electr, 5, 815–820.
Acknowledgments
We wish to thank the centers for their participation in the ERACE study (enrolled number of patients in brackets). The logistic support for the centers by the responsible study coordinator Mrs. Andrea Ungefehr as well as the data management by Dr. Carsten Morkel (both employees of Boston Scientific) were highly appreciated.
Participating centers: Berlin, Charité—Universitaetsmedizin Berlin, Campus Benjamin Franklin (4), Berlin, Deutsches Herzzentrum Berlin (35), Coburg, Klinikum Coburg gGmbH (7), Dachau, Amper Kliniken AG (2), Duesseldorf, Universitaetsklinikum Duesseldorf (6), Erfurt, Kardiologie am Fischmarkt (3), Erfurt, Kardiologische Gemeinschaftspraxis Dr. Bischoff und Dr. Lang (4), Frankfurt am Main, CCB Cardioangiologisches Centrum Bethanien (8), Hamburg, Asklepios Kliniken Hamburg (5), Hannover, Medizinische Hochschule Hannover (2), Heidelberg, Universitaetsklinikum Heidelberg (24), Karlsruhe, Staedt. Klinikum Karlsruhe gGmbH (16), Landshut, Krankenhaus Landshut-Achdorf (8), Mainz, Johannes-Gutenberg-Universitaet Mainz (4), Muenchen, KGP Dr. Boedigheimer, Dr. Muehling, Prof. Silber (4), Muenchen, Klinik Augustinum Muenchen (1), Muenster, Westf. Wilhelms-Universitaet Muenster Med. Klinik u. Poliklinik C (9), Oldenburg, Klinikum Oldenburg gGmbH (9), Stuttgart, Klinikum Stuttgart Katharinenhospital (8), all Germany
Amiens, CHRU Amiens—Hôpital Sud (4), Angers, CHU (11), Avignon, CH Henri Duffaut (3), Caen, CHU Caen (2), Clamart, Hopital A Béclère (4), Clermont Ferrand, Cl des Dômes (1), Dijon, Hopital du Bocage (4), Fort de France, CHU (2), Grenoble, CHU Albert Michallon (29), La Roche sur Yon, CHD La Roche Yon (6), Lyon, Hopital de la Croix Rousse (1), Marseille, CHP Clairval (2), Marseille, La Timone (1), Nantes, Nouvelles cliniques Nantaises (9), Orleans, CHR Orleans, Hopital La Source (13), Paris, Clinique Bizet (7), Paris, Pitie Salpetrière (4), Pau, Sise au Centre Hospitalier de Pau ( 18), Rennes, Hôpital Pontchaillou (1), Rouen, CHU de Rouen (1), Toulouse, Clinique Pasteur (9), Toulouse, Hopital Rangueil (4), Tours, CHU—Hôpital Trousseau (10), all France.
Conflict of interest
Sven Treusch, MD, and Klaus Contzen, PhD are employees of Boston Scientific Corporation.
Funding
This study was sponsored by Guidant/Boston Scientific Int. Inc.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Goetze, S., Defaye, P., Bauer, A. et al. Phrenic nerve stimulation in CRT patients and benefits of electronic lead repositioning: the ERACE trial. J Interv Card Electrophysiol 38, 1–9 (2013). https://doi.org/10.1007/s10840-013-9811-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-013-9811-9