Abstract
Purpose
The purpose of this narrative review was to assess the limited literature on fetal anomalies diagnosed in the second trimester of pregnancy and parental decision-making and identify sources of information deemed as facilitators and barriers to medical decisions.
Methods
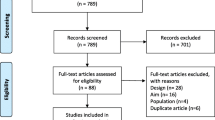
This was a literature review of source material and information about fetal anomalies diagnosed in the second trimester of pregnancy, decision-making, decision tools or aids, and sources of information for anomalies. The search string used explored related peer-reviewed publications and systematic reviews between 2007 and 2024. We also reviewed references from publications meeting inclusion criteria. The search was conducted between June 2022 and February 2024. Exclusion criteria included conference abstracts, non-peer reviewed literature, and articles not available in English language. A total of 77 publications were identified by searching multiple databases using a predefined search string. The search encompassed full text articles from 2007 to 2024 and 11 full-text publications were ultimately included in the review. A list of 45 co-occurring keywords was generated from the included texts, with each keyword having a minimum of two co-occurrences.
Results
Key themes identified included (1) the role of the clinician and need for development of professional knowledge and empathy surrounding discussion of fetal anomalies with patients; (2) information gathering, with individuals reporting use of multiple strategies to obtain information; while the majority found information satisfying, they preferred more details on diagnosis, long-term outcomes of the fetus/child and management of the pregnancy or termination process; and (3) decision-making, the path and process of how individuals made decisions about the pregnancy including quality of life, future fertility, and seeking other people’s experiences.
Conclusion
Many factors contribute to an individual’s decision-making after a diagnosis of a fetal anomalies diagnosed in the second trimester of pregnancy, ranging from personal beliefs and goals to shared experiences of others and access to care. Understanding how sources of information may be deemed both as facilitators and barriers to different individuals during the decision-making process is important for healthcare providers in order to understand how to most effectively support patients. There is a dearth of information on training healthcare professionals to provide support to patients facing these decisions.



Similar content being viewed by others
References
Rose NC, Kaimal AJ, Dugoff L, Norton ME, American College of Obstetricians and Gynecologists. Screening for fetal chromosomal abnormalities: ACOG practice bulletin, number 226. Obstet Gynecol. 2020;136(4):e48–69.
Sommerseth E, Sundby J. Women’s experiences when ultrasound examinations give unexpected findings in the second trimester. Women Birth. 2010;23(3):111–6.
Coleman P. Diagnosis of fetal anomaly and the increased maternal psychological toll associated with pregnancy termination. Issues in Law Med. 2015;30:3–23.
Redlinger-Grosse K, Bernhardt BA, Berg K, Muenke M, Biesecker BB. The decision to continue: the experiences and needs of parents who receive a prenatal diagnosis of Holoprosencephaly. Am J Med Genet. 2002;112:369–78. https://doi.org/10.1002/ajmg.10657.
Gawron LM, Cameron KA, Phisuthikul A, Simon MA. An exploration of women’s reasons for termination timing in the setting of fetal abnormalities. J Contracept. 2013;88:109–15. https://doi.org/10.1016/j.contraception.2012.12.004.
Guon J, Wilfond BS, Farlow B, Brazg T, Janvier A. Our children are not a diagnosis: the experience of parents who continue their pregnancy after prenatal diagnosis of trisomy 13 or 18. Am J Med Genet. 2014;164(2):308–18. https://doi.org/10.1002/ajmg.a.36298.
Reddy UM, Abuhamad AZ, Levine D, Saade GR, Participants FIWI. Fetal imaging: Executive summary of a joint Eunice Kennedy Shriver National Institute of child health and human development, Society for Maternal-Fetal medicine, American Institute of ultrasound in medicine, American College of obstetricians and Gynecologists, American College of radiology, Society for pediatric radiology, and society of radiologists in ultrasound fetal imaging workshop. Am J Obstet Gynecol. 2014;210(5):387–97.
Andersson IM, Gemzell-Danielsson K, Christensson K. Caring for women undergoing second-trimester medical termination of pregnancy. Contraception. 2014;89(5):460–5.
Andersson IM, Christensson K, Gemzell-Danielsson K. Experiences, feelings and thoughts of women undergoing second trimester medical termination of pregnancy. PLoS ONE. 2014;9(12):e115957.
Kerns JL, Mengesha B, McNamara BC, Cassidy A, Pearlson G, Kuppermann M. Effect of counseling quality on anxiety, grief, and coping after second-trimester abortion for pregnancy complications. Contraception. 2018;97(6):520–3.
Ramdaney A, Hashmi SS, Monga M, Carter R, Czerwinski J. Support desired by women following termination of pregnancy for a fetal anomaly. J Genet Couns. 2015;24(6):952–60.
Govender L, Ndjapa-Ndamkou C, Aldous C, Moodley J. A pilot study of women’s experiences after being offered late termination of pregnancy for severe fetal anomaly. Niger J Clin Pract. 2015;18(Suppl 1):S71–6.
Hendrix T, Roncoroni J, Magdamo B, Whitaker S, Zareba K, Grieco N. Stigma, social support, and decision satisfaction in terminations of pregnancy for medical reasons. Women’s Health Reports. 2023;4(1):271–9.
Maguire M, Light A, Kuppermann M, Dalton VK, Steinauer JE, Kerns JL. Grief after second-trimester termination for fetal anomaly: a qualitative study. Contraception. 2015;91(3):234–9.
Maistrellis E, Janiak E, Hammel R, Hurwitz S, Delli-Bovi L, Bartz D. Demographic, clinical, and counseling factors associated with the selection of pregnancy termination method in the second trimester for fetal and pregnancy anomalies. Womens Health Issues. 2019;29(4):349–55.
Kerns J, Vanjani R, Freedman L, Meckstroth K, Drey EA, Steinauer J. Women’s decision making regarding choice of second trimester termination method for pregnancy complications. Int J Gynecol Obstet. 2012;116(3):244–8.
Yee LM, Simon MA. The role of health literacy and numeracy in contraceptive decision-making for urban Chicago women. J Community Health. 2014;39:394–9.
Wills CE, Holmes-Rovner M. Patient comprehension of information for shared treatment decision making: state of the art and future directions. Patient Educ Couns. 2003;50(3):285–90.
Ancker JS, Kaufman D. Rethinking health numeracy: a multidisciplinary literature review. J Am Med Inform Assoc. 2007;14(6):713–21.
Entwistle VA, France EF, Wyke S, Jepson R, Hunt K, Ziebland S, Thompson A. How information about other people’s personal experiences can help with healthcare decision-making: a qualitative study. Patient Educ Couns. 2011;85(3):e291–8.
McKinnon LC, Prosser SJ, Miller YD. What women want: qualitative analysis of consumer evaluations of maternity care in Queensland, Australia. BMC Pregnancy Childbirth. 2014;14:1–14.
Meier S, Carter MM, DeMaria AL. “And Understand I am a Person and Not Just a Number:” Reproductive Healthcare Experiences of Italian Women. Women’s Reprod Health. 2021;8(1):60–78.
Cernat A, De Freitas C, Majid U, Higgins C, Vanstone M. Facilitating informed choice about non-invasive prenatal testing (NIPT): a systematic review and qualitative meta-synthesis of women’s experiences. BMC Pregnancy Childbirth. 2019;19(1):1–15.
Vamos CA, Merrell L, Detman L, Louis J, Daley E. Exploring women’s experiences in accessing, understanding, appraising, and applying health information during pregnancy. J Midwifery Womens Health. 2019;64(4):472–80.
Thapa DK, Visentin DC, Kornhaber R, West S, Cleary M. The influence of online health information on health decisions: A systematic review. Patient Educ Couns. 2021;104(4):770–84.
Wang C, Han L, Stein G, Day S, Bien-Gund C, Mathews A, Ong JJ, Zhao PZ, Wei SF, Walker J, Chou R. Crowdsourcing in health and medical research: a systematic review. Infect Dis Poverty. 2020;9:1–9.
Wazny K. Applications of crowdsourcing in health: an overview. J Glob Health. 2018;8(1):010502.
Chang T, Verma B, Shull T, et al. Crowdsourcing and the accuracy of online information regarding weight gain in pregnancy: a descriptive study. J Med Internet Res. 2016;18(4):e81.
H.B. 537 (Louisiana 2022). https://www.legis.la.gov/legis/BillInfo.aspx?s=22RS&b=HB537&sbi=y. Accessed 03–15–24.
Summit A, Chong E. Abortion training in family medicine residency programs: a national survey of program directors 5 months after the Dobbs Decision. Family Med. 2024.
Sabbath EL, McKetchnie SM, Arora KS, Buchbinder M. US Obstetrician-Gynecologists’ Perceived Impacts of Post-Dobbs v Jackson State Abortion Bans. JAMA Netw Open. 2024;7(1):e2352109. https://doi.org/10.1001/jamanetworkopen.2023.52109.
Author information
Authors and Affiliations
Contributions
J.P. collected, analyzed and interpreted the data and wrote the article. A.G., D.J., and C.M., interpreted the data and reviewed the article. G.Q. and C.P. reviewed the article and supervised the entire research process. All authors read, edited, and approved the final article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pecoriello, J., Lilly, A.G., Jalili, D. et al. Decision-making for congenital anomalies diagnosed during pregnancy: a narrative review. J Assist Reprod Genet (2024). https://doi.org/10.1007/s10815-024-03112-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10815-024-03112-x