Abstract
Purpose
To examine processes, barriers, and facilitators to sperm banking counseling and decision-making for adolescent males newly diagnosed with cancer from the perspective of clinicians who completed Oncofertility communication training. We also identify opportunities for improvement to inform future interventions and implementation.
Methods
A survey (N=104) and subsequent focus groups (N=15) were conducted with non-physician clinicians practicing in pediatric oncology who completed Oncofertility communication training.
Results
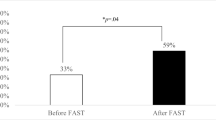
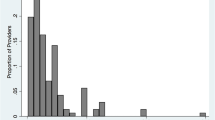
Most survey participants were confident in communicating about the impact of cancer on fertility (n=87, 83.7%) and fertility preservation options (n=80, 76.9%). Most participants reported never/rarely using a sperm banking decision tool (n=70, 67.3%), although 98.1% (n=102) said a decision tool with a family-centered approach would be beneficial. Primary themes in the subsequent focus groups included variable processes/workflows (inconsistent approaches to consult initiation; involvement of adolescents, caregivers, and various clinician types; assessment of puberty/sexual experience), structural and psychosocial barriers (cost and logistics, developmental, cultural, clinical acuity/prognosis), and facilitators (educational materials, alternative options for banking). Opportunities and strategies for improvement (including fertility preservation in existing research protocols; additional staffing/resources; oncologist education and buy-in; and development of decision tools) were informed by challenges identified in the other themes.
Conclusion
Barriers to adolescent sperm banking remain, even among clinicians who have completed Oncofertility training. Although training is one factor necessary to facilitate banking, structural and psychosocial barriers persist. Given the complexities of offering sperm banking to pediatric populations, continued efforts are needed to mitigate structural barriers and develop strategies to facilitate decision-making before childhood cancer treatment.

Similar content being viewed by others
Data Availability
Deidentified survey data are available upon request to the corresponding author.
References
Siegel RL, et al. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33. https://doi.org/10.3322/caac.21654.
Howlader N, et al. SEER cancer statistics review, 1975–2018. National Cancer Institute; 2021.
Hudson MM, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. Jama. 2013;309(22):2371–81. https://doi.org/10.1001/jama.2013.6296.
Green DM, et al. Fertility of male survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. J Clin Oncol. 2010;28(2):332. https://doi.org/10.1200/JCO.2009.24.9037.
Armuand GM, et al. Desire for children, difficulties achieving a pregnancy, and infertility distress 3 to 7 years after cancer diagnosis. Support Care Cancer. 2014;22:2805–12. https://doi.org/10.1007/s00520-014-2279-z.
Mulder RL, et al. Fertility preservation for male patients with childhood, adolescent, and young adult cancer: recommendations from the PanCareLIFE Consortium and the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2021;22(2):e57–67. https://doi.org/10.1016/S1470-2045(20)30582-9.
Practice Committee of the American Society for Reproductive Medicine. Fertility preservation in patients undergoing gonadotoxic therapy or gonadectomy: a committee opinion. Fertil Steril. 2019;112(6):1022–33. https://doi.org/10.1016/j.fertnstert.2019.09.013.
Kapadia A, et al. An institutional assessment of sperm cryospreservation and fertility counselling in pubertal male cancer survivors. J Pediatr Urol. 2020;16(4):474. https://doi.org/10.1016/j.jpurol.2020.05.164.
Saraf AJ, et al. Examining predictors and outcomes of fertility consults among children, adolescents, and young adults with cancer. Pediatric Blood Cancer. 2018;65(12):e27409. https://doi.org/10.1002/pbc.27409.
Patel V, et al. Recollection of fertility discussion in adolescent and young adult oncology patients: a single-institution study. J Adolesc Young Adult Oncol. 2020;9(1):72–7. https://doi.org/10.1089/jayao.2019.0075.
Stein DM, et al. Fertility preservation preferences and perspectives among adult male survivors of pediatric cancer and their parents. J Adolesc Young Adult Oncol. 2014;3(2):75–82. https://doi.org/10.1089/jayao.2014.0007.
Frederick NN, et al. Infrastructure of fertility preservation services for pediatric cancer patients: a report from the Children’s Oncology Group. JCO Oncol Pract. 2022;18(3):e325–33. https://doi.org/10.1200/OP.21.00275.
Frederick NN, et al. Fertility preservation practices at pediatric oncology institutions in the United States: a report from the Children’s Oncology Group. JCO Oncol Pract. 2023;19(4):e550–8. https://doi.org/10.1200/OP.22.00349.
Nahata L, Gerhardt CA, Quinn GP. Fertility preservation discussions with male adolescents with cancer and their parents: “ultimately, it’s his decision”. JAMA Pediatr. 2018;172(9):799–800. https://doi.org/10.1001/jamapediatrics.2018.1534.
Hayden RP, Kashanian JA. Facing a cancer diagnosis: empowering parents to speak with adolescents about sperm banking. Fertil Steril. 2017;108(6):957–8. https://doi.org/10.1016/j.fertnstert.2017.09.035.
Morgan TL, et al. Recruiting families and children newly diagnosed with cancer for behavioral research: important considerations and successful strategies. Psychooncology. 2019;28(4):928–30. https://doi.org/10.1002/pon.5012.
Clinicians. CMS.gov, Accessed July 24, 2023; https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/MMS/QMY-Clinicians
Klosky JL, et al. Prevalence and predictors of sperm banking in adolescents newly diagnosed with cancer: examination of adolescent, parent, and provider factors influencing fertility preservation outcomes. J Clin Oncol. 2017;35(34):3830. https://doi.org/10.1200/JCO.2016.70.4767.
Olsavsky AL, et al. Family communication about fertility preservation in adolescent males newly diagnosed with cancer. Pediatr Blood Cancer. 2021;68(7):e28978. https://doi.org/10.1002/pbc.28978.
Fuchs A, et al. Pediatric oncology providers’ attitudes and practice patterns regarding fertility preservation in adolescent male cancer patients. J Pediatr Hematol/Oncol. 2016;38(2):118. https://doi.org/10.1097/MPH.0000000000000488.
Vadaparampil ST, Hutchins NM, Quinn GP. Reproductive health in the adolescent and young adult cancer patient: an innovative training program for oncology nurses. J Cancer Educ. 2013;28:197–208. https://doi.org/10.1007/s13187-012-0435-z.
Vadaparampil ST, et al. ENRICH: a promising oncology nurse training program to implement ASCO clinical practice guidelines on fertility for AYA cancer patients. Patient Educ Couns. 2016;99(11):1907–10. https://doi.org/10.1016/j.pec.2016.05.013.
Quinn GP, et al. Impact of a web-based reproductive health training program: ENRICH (Educating Nurses about Reproductive Issues in Cancer Healthcare). Psycho-oncology. 2019;28(5):1096–101. https://doi.org/10.1002/pon.5063.
Pecoriello J, et al. Evolution and growth of the ECHO (Enriching Communication skills for Health professionals in Oncofertility) program: a 5-year study in the training of oncofertility professionals. J Cancer Surviv. 2022. https://doi.org/10.1007/s11764-021-01139-y.
Barrett F, et al. Perspectives surrounding fertility preservation and posthumous reproduction for adolescent and young adults with terminal cancer: survey of allied health professionals. Cancer Med. 2023;12(5):6129–38. https://doi.org/10.1002/cam4.5345.
Glaser BG. The constant comparative method of qualitative analysis. Social problems. 1965;12(4):436–45.
Panagiotopoulou N, et al. Barriers and facilitators towards fertility preservation care for cancer patients: a meta-synthesis. Eur J Cancer Care (Engl). 2018;27(1):e12428. https://doi.org/10.1111/ecc.12428.
Flynn JS, et al. Parent recommendation to bank sperm among at-risk adolescent and young adult males with cancer. Pediatr Blood Cancer. 2020;67(10):e28217. https://doi.org/10.1002/pbc.28217.
Klosky JL, et al. Parental influences on sperm banking attempts among adolescent males newly diagnosed with cancer. Fertil Steril. 2017;108(6):1043–9. https://doi.org/10.1016/j.fertnstert.2017.08.039.
Nahata L, et al. Parent–adolescent concordance regarding fertility perspectives and sperm banking attempts in adolescent males with cancer. J Pediatr Psychol. 2021;46(10):1149–58. https://doi.org/10.1093/jpepsy/jsab069.
Nahata L, et al. Impact of a novel family-centered values clarification tool on adolescent sperm banking attempts at the time of a new cancer diagnosis. J Assist Reprod Genet. 2021;38:1561–9. https://doi.org/10.1007/s10815-021-02092-6.
Letourneau JM, et al. Racial, socioeconomic, and demographic disparities in access to fertility preservation in young women diagnosed with cancer. Cancer. 2012;118(18):4579–88. https://doi.org/10.1002/cncr.26649.
Voigt PE, et al. Equal oppurtunity for all? An analysis of race and ethnicity in fertility preservation in New York City. J Assist Reprod Genet. 2020;37:3095–102. https://doi.org/10.1007/s10815-020-01980-7.
Canzona MR, et al. Fertility preservation decisional turning points for adolescents and young adults with cancer: exploring alignment and divergence by race and ethnicity. JCO Oncol Pract. 2023; https://doi.org/10.1200/op.22.00613.
Woodruff TK, et al. A view from the past into our collective future: the oncofertility consortium visit statemnet. J Assist Reprod Genet. 2021;38:3–15. https://doi.org/10.1007/s10815-020-01983-4.
Author contributions
LN, GPQ, CAG, SHO, and STV contributed to the study conception and design. Material preparation, data collection, and analysis were performed by LN, SML, DJ, and GPQ. The first draft of the manuscript was written by LN, SML, DJ, and GPQ. All authors read, revised, and approved the final manuscript.
Funding
This study was funded by NIH/NCI-K08CA237338 (PI Nahata) and 2R25CA142519-11 (MPIs Quinn and Vadaparampil) and NYU Grossman School of Medicine.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was deemed non-human subjects by the New York University Institutional Review Board.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nahata, L., Liles, S.M., Gerhardt, C.A. et al. Clinicians’ perspectives on barriers and facilitators to sperm banking in adolescent males with cancer: a mixed-methods study. J Assist Reprod Genet 40, 2809–2817 (2023). https://doi.org/10.1007/s10815-023-02944-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02944-3