Abstract
Purpose
To evaluate pre-implantation genetic testing for aneuploidy (PGT-A) outcomes in patients without infertility compared to infertile patients.
Methods
We performed a retrospective cohort study of all patients without an infertility diagnosis (“fertile” patients) who utilized PGT-A at a large university-affiliated fertility center between 2016 and 2021. Fertile patients were 1-to-3 matched to infertile controls by age and number of oocytes retrieved. The primary outcome was blastocyst aneuploidy rate. Secondary outcomes included ovarian reserve markers, laboratory outcomes, and other PGT-A outcomes [rates of euploidy, mosaicism, and potentially transferrable (euploid + mosaic) embryos].
Results
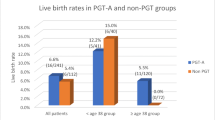
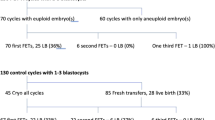
283 fertile and 849 infertile patients were included. Median age, anti-Mullerian hormone, and day 2 estradiol levels were equivalent among groups; day 2 follicle-stimulating hormone levels were higher in fertile patients (6.9 vs. 6.5 IU/mL, p < 0.01). The aneuploidy rate was similar among fertile and infertile patients (33.7% vs. 31.8%, p = 0.11); the euploidy rate was higher (50.8% vs. 47.0%, p < 0.01), and the mosaicism rate was lower in fertile patients (13.3% vs. 19.2%, p < 0.01). The rate of transferrable embryos was similar among groups (64.0% vs. 66.3%, p = 0.07), as was the percentage of patients yielding ≥ 1 euploid embryo (90.1% vs. 87.3%, p = 0.25). When controlling for significant covariates, multiple linear regression showed that aneuploidy rate was equivalent in both cohorts.
Conclusion
Aneuploidy rate was similar in fertile and infertile patients. Fertile patients had slightly higher euploidy and lower mosaicism than infertile patients. Still, compared to fertile patients, infertile patients had equivalent rates of transferrable embryos and were just as likely to yield ≥ 1 euploid embryo.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, EAC, upon reasonable request.
References
Hodes-Wertz B, Grifo J, Ghadir S, Kaplan B, Laskin CA, Glassner M, et al. Idiopathic recurrent miscarriage is caused mostly by aneuploid embryos. Fertil Steril. 2012;98:675–80.
Marquard K, Westphal LM, Milki AA, Lathi RB. Etiology of recurrent pregnancy loss in women over the age of 35 years. Fertil Steril. 2010;94:1473–7.
Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2:280–91.
Pylyp LY, Spynenko LO, Verhoglyad NV, Mishenko AO, Mykytenko DO, Zukin VD. Chromosomal abnormalities in products of conception of first-trimester miscarriages detected by conventional cytogenetic analysis: a review of 1000 cases. J Assist Reprod Genet. 2018;35:265–71.
Lee H, McCulloh DH, Hodes-Wertz B, Adler A, McCaffrey C, Grifo JA. In vitro fertilization with preimplantation genetic screening improves implanation and live birth in women age 40 through 43. J Assist Reprod Genet. 2015;32:435–44.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril. 2014;101:656–63.
Pantou A, Mitrakos A, Kokkali G, Petroutsou K, Tounta G, Lazaros L, Dimopoulos A, Sfakianoudis K, Pantos K, Koutsilieris M, Mavrou A, Kanavakis E, Tzetis M. The impact of preimplantation genetic testing for aneuploidies (PGT-A) on clinical outcomes in high risk patients. J Assist Reprod Genet. 2022;39:1341–9.
Simopoulou M, Sfakianoudis K, Maziotis E, et al. PGT-A: who and when? Alpha systematic review and network meta-analysis of RCTs. J Assist Reprod Genet. 2021;38:1939–57.
Roche K, Racowsky C, Harper J. Utilization of preimplantation genetic testing in the USA. J Assist Reprod Genet. 2021;38:1045–53.
Practice Committees of the American Society for Reproductive Medicine and the Society for Assisted Reproductive Technology. The use of preimplantation genetic testing for aneuploidy (PGT-A): a committee opinion. Fertil Steril. 2018;109(3):429–436.
Taylor TH, Patrick JL, Gitlin SA, Crain JL, Wilson JM, Griffin DK. Blastocyst euploidy and implantation rates in young (<35 years) and old (≥35 years) presumed fertile and infertile patient population. Fertil Steril. 2014;102:1318–23.
Kort JD, McCoy RC, Demko Z, Lathi RB. Are blastocyst aneuploidy rates different between fertile and infertile populations? J Assist Reprod Genet. 2018;35:403–8.
Hoyos LR, Cheng CY, Brennan K, et al. Euploid rates among oocyte donors: is there an optimal age for donation? J Assist Reprod Genet. 2020;37:589–94.
Munne S, Alikani M, Ribustello L, et al. Euploidy rates in donor egg cycles significantly differ between fertility centers. Hum Reprod. 2017;32:743–9.
Leigh D, Cram DS, Rechitsky S, Handyside A, Wells D, Munne S, et al. PGDIS position statement on the transfer of mosaic embryos 2021. Reprod Biomed Online. 2022;45:19–25.
Practice Committee and Genetic Counseling Professional Group (GCPG) of the American Society for Reproductive Medicine. Clinical management of mosaic results from preimplantation genetic testing for aneuploidy (PGT-A) of blastocysts: a committee opinion. Fertil Steril. 2020;114:246–54.
Victor AR, Tyndall JC, Brake AJ, Lepkowsky LT, Murphy AE, Griffin DK, et al. One hundred mosaic embryos transferred prospectively in a single clinic: exploring when and why they result in healthy pregnancies. Fertil Steril. 2019;111:280–93.
Lee CI, Cheng EH, Lee MS, Lin PY, Chen YC, Chen CH, et al. Healthy live births from transfers of low-mosaicism embryos after preimplantation genetic testing for aneuploidy. J Assist Reprod Genet. 2020;37:2305–13.
Fragouli E, Alfarawati S, Spath K, Babariya D, Tarozzi N, Borini A, et al. Analysis of implantation and ongoing pregnancy rates following the transfer of mosaic diploid-aneuploid blastocysts. Hum Genet. 2017;136:805–19.
Zore T, Kroener LL, Wang C, Liu L, Buyalos R, Hubert G, Shamonki M. Transfer of embryos with segmental mosaicism is associated with a significant reduction in live-birth rate. Fertil Steril. 2019;111:69–76.
Capalbo A, Poli M, Rienzi L, Girardi L, Patassini C, Fabiani M, et al. Mosaic human preimplantation embryos and their developmental potential in a prospective, non-selection clinical trial. Am J Hum Genet. 2021;108(12):2238–47.
Stovezky YR, Romanski PA, Bortoletto P, Spandorfer SD. Body mass index is not associated with embryo ploidy in patients undergoing in vitro fertilization with preimplantation genetic testing. Fertil Steril. 2021;116:388–95.
Goldman KN, Hodes-Wertz B, McCulloh DH, Flom JD, Grifo JA. Association of body mass index with embryonic aneuploidy. Fertil Steril. 2015;103:744–8.
Massie JAM, Shahine LK, Milki A, Westphal L, Lathi R. Ovarian stimulation and the risk of aneuploid conceptions. Fertil Steril. 2011;95:970–2.
Barash OO, Hinckley MD, Rosenbluth EM, Ivani KA, Weckstein LN. Hum Reprod. 2017;32:2209–17.
Cascales A, Lledó B, Ortiz JA, Morales R, Ten J, Llácer J, et al. Effect of ovarian stimulation on embryo aneuploidy and mosaicism rate. Syst Biol Reprod Med. 2021;67:42–9.
Baart EB, Martini E, Eijkemans MJ, van Opstal D, Beckers NGM, Verhoeff A, et al. Milder ovarian stimulation for in-vitro fertilization reduces aneuploidy in the human preimplantation embryo: a randomized controlled trial. Hum Reprod. 2007;22:980–8.
Katz-Jaffe MG, Trounson AO, Cram DS. Chromosome 21 mosaic human preimplantation embryos predominantly arise from diploid conceptions. Fertil Steril. 2005;84:634–43.
Acknowledgements
The authors thankfully acknowledge the patients included in this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by Emily A. Clarke and Asha K. Dahiya. The first draft of the manuscript was written by Emily A. Clarke, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and informed consent
This research study was conducted retrospectively from data obtained for clinical purposes. The study was performed with New York University Institutional Review Board approval (s13-00389).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clarke, E.A., Dahiya, A.K., Cascante, S.D. et al. Evaluation of pre-implantation genetic testing for aneuploidy outcomes in patients without infertility undergoing in vitro fertilization compared to infertile controls. J Assist Reprod Genet 40, 2697–2704 (2023). https://doi.org/10.1007/s10815-023-02941-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02941-6