Abstract
Purpose
To assess the feasibility and outcomes of oocyte cryopreservation with in vitro maturation (IVM) in post-pubertal girls undergoing fertility preservation (FP) for primary ovarian insufficiency (POI) risk.
Methods
Ovarian stimulation was performed with an antagonist protocol or progesterone priming. Ultrasound monitoring was performed transabdominally. Oocytes were retrieved transvaginally under IV sedation. Immature oocytes were subjected to IVM for up to 36 h. All MII oocytes were vitrified. The main outcome measure was the total number of mature oocytes cryopreserved. The secondary outcome was the increase in the mature oocyte yield after IVM.
Results
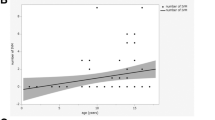
Indications for FP included mosaic Turner syndrome (mTS; n = 10), malignancy (n = 3), and POI risk (n = 2). The mean ± SD age, antral follicle count (AFC), and AMH levels were 14.2 ± 1.4 years, 8 ± 5.2 and 1.3 ± 1.3 ng/mL. In girls with mTS, the ovarian reserve was low for age (AFC 7.4 ± 4.7 and AMH 1.4 ± 1.6 ng/mL). Oocyte cryopreservation was possible in all girls with a range of 1–27 mature oocytes obtained, even in those who were previously exposed to chemotherapy or with low ovarian reserve, and no surgical complications were encountered. After IVM, the median mature oocyte yield increased significantly from 7.5 to 10.5 (p = 0.001).
Conclusions
Oocyte cryopreservation appears to be feasible and safe in girls as young as 12 years of age at risk for POI The utility of IVM increases the yield of cryopreserved mature oocytes. Prior exposure to chemotherapy or low ovarian reserve should not be an automatic reason to exclude these girls from FP consideration.
Similar content being viewed by others
References
United Nations General Assembly. Convention on the Rights of the Child. Annu Rev Popul Law. 1989;16:95, 485–501.
Rodriguez-Wallberg KA, Oktay K. Fertility preservation medicine: options for young adults and children with cancer. J Pediatr Hematol Oncol. 2010;32(5):390–6.
Hovatta O. Ovarian function and in vitro fertilization (IVF) in Turner syndrome. Pediatr Endocrinol Rev. 2012;9(Suppl 2):713–7.
Talaulikar VS, Conway GS, Pimblett A, Davies MC. Outcome of ovarian stimulation for oocyte cryopreservation in women with Turner syndrome. Fertil Steril. 2019;111(3):505–9.
Bernard V, Donadille B, Zenaty D, Courtillot C, Salenave S, Brac de la Perrière A, Albarel F, Fèvre A, Kerlan V, Brue T, Delemer B, Borson-Chazot F, Carel J-C, Chanson P, Léger J, Touraine P, Christin-Maitre S. Spontaneous fertility and pregnancy outcomes amongst 480 women with Turner syndrome. Hum Reprod. 2016;31(4):782–788.
McCracken K, Nahata L. Fertility preservation in children and adolescents: current options and considerations. Curr Opin Obstet Gynecol. 2017;29(5):283–8.
Oktay K, Harvey BE, Partridge AH, Quinn GP, Reinecke J, Taylor HS, Wallace WH, Wang ET, Loren AW. Fertility preservation in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol. 2018;36(19):1994–2001.
Oktay K, Karlikaya G. Ovarian function after transplantation of frozen, banked autologous ovarian tissue. N Engl J Med. 2000;342(25):1919.
Oktay K, Oktem O. Fertility preservation medicine: a new field in the care of young cancer survivors. Pediatr Blood Cancer. 2009;53(2):267–73.
Poirot C, Brugieres L, Yakouben K, Prades‐Borio M, Marzouk F, Lambert G, Pacquement H, Bernaudin F, Neven B, Paye‐Jaouen A, Pondarre C, Dhedin N, Drouineaud V, Chalas C, Martelli H, Michon J, Minard V, Lezeau H, Doz F, Sarnacki S, Philippe‐Chomette P, Dufour C, Laurence V, Baruchel A, Wolf J, Boissel N, Valteau‐Couanet D, Dalle J. Ovarian tissue cryopreservation for fertility preservation in 418 girls and adolescents up to 15 years of age facing highly gonadotoxic treatment. Twenty years of experience at a single center. Acta Obstet Gyneco. Scand. 2019;98(5):630–637.
Oktay K, Newton H, Aubard Y, Salha O, G.Gosden R. Cryopreservation of immature human oocytes and ovarian tissue: an emerging technology? Fertil Steril.1998;69(1):1–7.
Sugishita Y, Suzuki N. Methods of ovarian tissue cryopreservation: vitrification. In: Principles and Practice of Ovarian Tissue Cryopreservation and Transplantation. Elsevier; 2022:99–107.
Oktay K, Bedoschi G, Berkowitz K, Bronson R, Kashani B, McGovern P, Pal L, Quinn G, Rubin K. Fertility preservation in women with Turner syndrome: a comprehensive review and practical guidelines. J Pediatr Adolesc Gynecol. 2016;29(5):409–16.
Oktay K, Bedoschi G. Fertility preservation in girls with Turner syndrome: limitations, current success and future prospects. Fertil Steril. 2019;111(6):1124–6.
Poirot C. Ovarian cryopreservation for transplantation with prepubertal and adolescent girls. In: Principles and Practice of Ovarian Tissue Cryopreservation and Transplantation. Elsevier; 2022:127–141.
Soleimani R, Heytens E, Oktay K. Enhancement of neoangiogenesis and follicle survival by sphingosine-1-phosphate in human ovarian tissue xenotransplants. Bernhard EJ, ed. PLoS One 2011;6(4):e19475.
Oktay K, Bedoschi G, Pacheco F, Turan V, Emirdar V. First pregnancies, live birth, and in vitro fertilization outcomes after transplantation of frozen-banked ovarian tissue with a human extracellular matrix scaffold using robot-assisted minimally invasive surgery. Am J Obstet Gynecol. 2016;214(1):94.e1-94.e9.
Taylan E, Oktay K. Application of decellularized tissue scaffolds in ovarian tissue transplantation. In. 2017:177–181.
Taylan E, Oktay K. Autologous transplantation of human ovarian tissue. In: The Ovary. Elsevier; 2019:493–500.
Marin L, Bedoschi G, Kawahara T, Oktay KH. History, evolution and current state of ovarian tissue auto-transplantation with cryopreserved tissue: a successful translational research journey from 1999 to 2020. Reprod Sci. 2020;27(4):955–62.
Balen A, Harris S, Chambers E, Picton H. Conservation of fertility and oocyte genetics in a young woman with mosaic Turner syndrome. BJOG An Int J Obstet Gynaecol. 2010;117(2):238–42.
Strypstein L, Van Moer E, Nekkebroeck J, Segers I, Tournaye H, Demeestere I, Dolmans M-M, Verpoest W, De Vos M. First live birth after fertility preservation using vitrification of oocytes in a woman with mosaic Turner syndrome. J Assist Reprod Genet. 2022;39(2):543–9.
Mature oocyte cryopreservation. a guideline. Fertil Steril. 2013;99(1):37–43.
Grèze V, Mechdoud S, Vorilhon S, Isfan F, Rouel N, Chaput L, Brugnon F, Kanold J. Accès à la préservation de la fertilité des adolescents et jeunes adultes de 15 à 24 ans atteints de cancers en Auvergne. France Bull Cancer. 2020;107(7–8):773–8.
Oktay K, Rodriguez-Wallberg KA, Sahin G. Fertility preservation by ovarian stimulation and oocyte cryopreservation in a 14-year-old adolescent with Turner syndrome mosaicism and impending premature ovarian failure. Fertil Steril. 2010;94(2):753.e15-753.e19.
Oktay K, Bedoschi G. Oocyte cryopreservation for fertility preservation in postpubertal female children at risk for premature ovarian failure due to accelerated follicle loss in turner syndrome or cancer treatments. J Pediatr Adolesc Gynecol. 2014;27(6):342–6.
Martel RA, Blakemore JK, Fino ME. The use of oocyte cryopreservation for fertility preservation in patients with sex chromosome disorders: a case series describing outcomes. J Assist Reprod Genet. 2022;39(5):1143–53.
Mamsen LS, Charkiewicz K, Anderson RA, Telfer EE, McLaughlin M, Kelsey TW, Kristensen SG, Gook DA, Ernst E, Andersen CY. Characterization of follicles in girls and young women with turner syndrome who underwent ovarian tissue cryopreservation. Fertil Steril. 2019;111(6):1217-1225.e3.
Child TJ, Abdul-Jalil AK, Gulekli B, Tan SL. In vitro maturation and fertilization of oocytes from unstimulated normal ovaries, polycystic ovaries, and women with polycystic ovary syndrome. Fertil Steril. 2001;76(5):936–42.
Oktay K, Buyuk E, Rodriguez-Wallberg KA, Sahin G. In vitro maturation improves oocyte or embryo cryopreservation outcome in breast cancer patients undergoing ovarian stimulation for fertility preservation. Reprod Biomed Online. 2010;20(5):634–8.
Borini A, Coticchio G. Oocyte quantity and quality are crucial for a perspective of fertility preservation in women with Turner syndrome. Fertil Steril. 2019;111(3):461–2.
Comparison of pregnancy rates for poor responders using IVF with mild ovarian stimulation versus conventional IVF: a guideline. Fertil Steril. 2018;109(6):993–999.
Cohen Y, St-Onge-St-Hilaire A, Tannus S, Younes G, Dahan MH, Buckett W, Son W-Y. Decreased pregnancy and live birth rates after vitrification of in vitro matured oocytes. J Assist Reprod Genet. 2018;35(9):1683–9.
Cobo A, Coello A, de los Santos MJ, Giles J, Pellicer A, Remohí J, García-Velasco JA. Number needed to freeze: cumulative live birth rate after fertility preservation in women with endometriosis. Reprod Biomed Online. 2021;42(4):725–732.
Ferraretti AP, La Marca A, Fauser BCJM, Tarlatzis B, Nargund G, Gianaroli L. ESHRE consensus on the definition of “poor response” to ovarian stimulation for in vitro fertilization: the Bologna criteria. Hum Reprod. 2011;26(7):1616–24.
The Vienna consensus: report of an expert meeting on the development of art laboratory performance indicators†‡. Hum Reprod Open. 2017;2017(2). https://doi.org/10.1093/hropen/hox011.
Purushothaman R, Lazareva O, Oktay K, Ten S. Markers of ovarian reserve in young girls with Turner’s syndrome. Fertil Steril. 2010;94(4):1557–9.
Gravholt CH, Viuff M, Just J, Sandahl K, Brun S, van der Velden J, Andersen NH, Skakkebaek A. The changing face of turner syndrome. Endocr Rev. 2023;44(1):33–69.
Visser JA, Hokken-Koelega ACS, Zandwijken GRJ, Limacher A, Ranke MB, Fluck CE. Anti-Mullerian hormone levels in girls and adolescents with Turner syndrome are related to karyotype, pubertal development and growth hormone treatment. Hum Reprod. 2013;28(7):1899–907.
Vergier J, Bottin P, Saias J, Reynaud R, Guillemain C, Courbiere B. Fertility preservation in Turner syndrome: Karyotype does not predict ovarian response to stimulation. Clin Endocrinol (Oxf). 2019;91(5):646–51.
Pilsgaard F, Grynnerup AG-A, Løssl K, Bungum L, Pinborg A. The use of anti-Müllerian hormone for controlled ovarian stimulation in assisted reproductive technology, fertility assessment and -counseling. Acta Obstet Gynecol Scand. 2018;97(9):1105–1113.
Oktem O, Oktay K. Quantitative assessment of the impact of chemotherapy on ovarian follicle reserve and stromal function. Cancer. 2007;110(10):2222–9.
Oktem O, Oktay K. A novel ovarian xenografting model to characterize the impact of chemotherapy agents on human primordial follicle reserve. Cancer Res. 2007;67(21):10159–62.
Soleimani R, Heytens E, Darzynkiewicz Z, Oktay K. Mechanisms of chemotherapy-induced human ovarian aging: double strand DNA breaks and microvascular compromise. Aging (Albany NY). 2011;3(8):782–793.
Titus S, Szymanska KJ, Musul B, Turan V, Taylan E, Garcia- Milian R, Mehta S, Oktay K. Individual-oocyte transcriptomic analysis shows that genotoxic chemotherapy depletes human primordial follicle reserve in vivo by triggering proapoptotic pathways without growth activation. Sci Rep. 2021;11(1):407.
Goldfarb SB, Turan V, Bedoschi G, Taylan E, Abdo N, Cigler T, Bang H, Patil S, Dickler MN, Oktay KH. Impact of adjuvant chemotherapy or tamoxifen-alone on the ovarian reserve of young women with breast cancer. Breast Cancer Res Treat. 2021;185(1):165–73.
Titus S, Li F, Stobezki R, Akula K, Unsal E, Jeong K, Dickler M, Robson M, Moy F, Goswami S, Oktay K. Impairment of BRCA1-related DNA double-strand break repair leads to ovarian aging in mice and humans. Sci Transl Med. 2013;5(172). https://doi.org/10.1126/scitranslmed.3004925.
Turan V, Oktay K. BRCA-related ATM-mediated DNA double-strand break repair and ovarian aging. Hum Reprod Update. 2020;26(1):43–57.
Oktay KH, Bedoschi G, Goldfarb SB, Taylan E, Titus S, Palomaki GE, Cigler T, Robson M, Dickler MN. Increased chemotherapy-induced ovarian reserve loss in women with germline BRCA mutations due to oocyte deoxyribonucleic acid double strand break repair deficiency. Fertil Steril. 2020;113(6):1251-1260.e1.
Byrne J, Rasmussen SA, Steinhorn SC, Connelly RR, Myers MH, Lynch CF, Flannery J, Austin DF, Holmes FF, Holmes GE, Strong LC, Mulvihill JJ. Genetic disease in offspring of long-term survivors of childhood and adolescent cancer. Am J Hum Genet. 1998;62(1):45–52.
Winther JF, Boice JD, Mulvihill JJ, Stovall M, Frederiksen K, Tawn EJ, Olsen JH. Chromosomal abnormalities among offspring of childhood-cancer survivors in Denmark: a population-based study. Am J Hum Genet. 2004;74(6):1282–5.
Oktay K, Newton H, Mullan J, Gosden RG. Development of human primordial follicles to antral stages in SCID/hpg mice stimulated with follicle stimulating hormone. Hum Reprod. 1998;13(5):1133–8.
Bedoschi GM, Navarro PA, Oktay KH. Novel insights into the pathophysiology of chemotherapy-induced damage to the ovary. Panminerva Med. 2019;61(1). https://doi.org/10.23736/S0031-0808.18.03494-8.
Sönmezer M, Türkçüoğlu I, Coşkun U, Oktay K. Random-start controlled ovarian hyperstimulation for emergency fertility preservation in letrozole cycles. Fertil Steril. 2011;95(6):2125.e9-2125.e11.
Kummer NE, Feinn RS, Griffin DW, Nulsen JC, Benadiva CA, Engmann LL. Predicting successful induction of oocyte maturation after gonadotropin-releasing hormone agonist (GnRHa) trigger. Hum Reprod. 2013;28(1):152–159s.
Acknowledgements
We thank Giuliano Bedoschi, M.D., Ph.D. for data clarification, and Anastasia Yedynak, clinical coordinator, for technical assistance. No compensation was received for their contributions.
Funding
K.O. is funded by NIH HD R01HD053112. Foundation Alfonso Martín Escudero (Madrid, Spain) provided grant support for S.G. research fellowship position.
Author information
Authors and Affiliations
Contributions
K.O. conceived the idea, directed the study, and wrote the manuscript; S.G. collected data and wrote the manuscript. V.T. collected data and wrote portions of the manuscript. S.G. and K.O. had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sonia Gayete-Lafuente and Volkan Turan had equal contributions.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gayete-Lafuente, S., Turan, V. & Oktay, K.H. Oocyte cryopreservation with in vitro maturation for fertility preservation in girls at risk for ovarian insufficiency. J Assist Reprod Genet 40, 2777–2785 (2023). https://doi.org/10.1007/s10815-023-02932-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02932-7