Abstract
Purpose
To investigate the effectiveness and safety of 36 different therapies for recurrent implantation failure (RIF) patients.
Methods
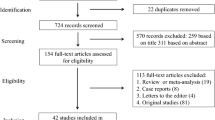
We searched PubMed, Embase, the Cochrane Library (CENTRAL), Web of Science, and China National Knowledge Internet (CNKI) from inception to August 24, 2022, with language in both English and Chinese. Randomized controlled trials (RCTs) and observational studies that provided data with one of pregnancy outcomes on RIF patients were included in the network meta-analysis (NMA). The odds ratios (OR) and 95% credible interval (CrI) on pregnancy outcomes were summarized by NMA with a random-effects model. We also analyzed data from only RCTs and compared whether the optimal treatment is the same for different failed embryo transfer attempts.
Results
The total of 29,906 RIF patients from 154 clinical studies (74 RCTs and 80 non-RCTs) were included in the NMA. In terms of implantation rate (IR), growth hormone (GH) (OR: 3.32, 95% CrI: 1.95–5.67) is the best treatment in all included studies; IVIG+PBMC (5.84, 2.44–14.1) is the best for clinical pregnancy rate (CPR); hyaluronic acid (HA) (12.9, 2.37–112.0) for live birth rate (LBR); and aspirin combined with glucocorticoids (0.208, 0.0494–0.777) for miscarriage rate (MR). The two-dimensional graphs showed that GH could maximize IR and CPR simultaneously; HA and GH could simultaneously increase IR and LBR to a large extent; HA could maximize IR and minimize MR.
Conclusion
IVIG+PBMC, GH, and embryo medium enriched with HA could significantly improve pregnancy outcomes in patients with RIF. It appears that combination therapy is a potential administration strategy.
Trial registration
This study has been registered on PROSPERO (CRD42022353423).




Similar content being viewed by others
Data availability
The data are derived from published studies, and all raw data used in the study are available in the supplementary files.
Abbreviations
- AECC:
-
autologous embryo-cumulus cells co-culture
- AH:
-
assisted hatching
- BET:
-
blastocyst-stage embryo transfer
- cGMP:
-
cyclic guanosine monophosphate
- CPR:
-
clinical pregnancy rate
- CrI:
-
credible interval
- EI:
-
endometrial injury
- EPR:
-
ectopic pregnancy rate
- ERA:
-
endometrial receptivity array
- ET:
-
embryos transfers
- GC:
-
glucocorticoids
- G-CSF:
-
granulocyte-colony stimulating factor
- GH:
-
growth hormone
- HA:
-
hyaluronic acid
- hCG:
-
human chorionic gonadotropin
- HCQ:
-
hydroxychloroquine
- HP:
-
hysteroscopy
- ICSI:
-
intracytoplasmic sperm injection
- IGF-1:
-
insulin-like growth factor 1
- IL:
-
interleukin
- IMSI:
-
intracytoplasmic morphologically selected sperm injection
- IR:
-
implantation rate
- ITGB3:
-
integrin beta 3
- IUD:
-
intra uterine device
- IVF:
-
in vitro fertilization
- IVIG:
-
intravenous immunoglobulins
- LBR:
-
live birth rate
- LIF:
-
leukemia inhibitory factor
- LIT:
-
lymphocyte immunotherapy
- LMWH:
-
low molecular weight heparin
- MR:
-
miscarriage rate
- mTOR:
-
mechanistic target of rapamycin
- NMA:
-
network meta-analysis
- OR:
-
odds ratios
- PBMC:
-
peripheral blood mononuclear cell
- PGT-A:
-
preimplantation genetic testing aneuploidy
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PRP:
-
platelet-rich plasma
- RCT:
-
randomized controlled trials
- r-hLIF:
-
recombinant human leukemia inhibitory factor
- RIF:
-
recurrent implantation failure
- ROBINS-I:
-
Risk of Bias in Non-Randomized Studies of Interventions
- RSA:
-
recurrent spontaneous abortion
- SET:
-
sequential embryo transfer
- SUCRA:
-
surface under the cumulative ranking curve
- TNF-α:
-
tumor necrosis factor-alpha
- Tregs:
-
regulatory T cells
- VEGF:
-
vascular endothelial growth factor
- ZIFT:
-
zygote intrafallopian tube transfer
References
Bashiri A, Halper KI, Orvieto R. Recurrent implantation failure-update overview on etiology, diagnosis, treatment and future directions. Reprod Biol Endocrinol. 2018;16:121.
Coughlan C, Ledger W, Wang Q, Liu F, Demirol A, Gurgan T, et al. Recurrent implantation failure: definition and management. Reprod Biomed Online. 2014;28:14–38.
Cimadomo D, Craciunas L, Vermeulen N, Vomstein K, Toth B. Definition, diagnostic and therapeutic options in recurrent implantation failure: an international survey of clinicians and embryologists. Hum Reprod. 2021;36:305–17.
Polanski LT, Baumgarten MN, Quenby S, Brosens J, Campbell BK, Raine-Fenning NJ. What exactly do we mean by ‘recurrent implantation failure’? A systematic review and opinion. Reprod Biomed Online. 2014;28:409–23.
Cimadomo D, de Los SM, Griesinger G, Lainas G, Le Clef N, McLernon DJ, et al. ESHRE good practice recommendations on recurrent implantation failure. Hum Reprod Open. 2023;2023:hoad23.
Penzias AS. Recurrent IVF failure: other factors. Fertil Steril. 2012;97:1033–8.
Saxtorph MH, Hallager T, Persson G, Petersen KB, Eriksen JO, Larsen LG, et al. Assessing endometrial receptivity after recurrent implantation failure: a prospective controlled cohort study. Reprod Biomed Online. 2020;41:998–1006.
Simon A, Laufer N. Assessment and treatment of repeated implantation failure (RIF). J Assist Reprod Genet. 2012;29:1227–39.
Wang C, Guan D, Li R, Bing Z, Yang Y, Yang K. Comparative efficacies of different immunotherapy regimens in recurrent implantation failure: a systematic review and network meta-analysis. J Reprod Immunol. 2021;148:103429.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence--imprecision. J Clin Epidemiol. 2011;64:1283–93.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
van Valkenhoef G, Dias S, Ades AE, Welton NJ. Automated generation of node-splitting models for assessment of inconsistency in network meta-analysis. Res Synth Methods. 2016;7:80–93.
Cui N, Li AM, Luo ZY, Zhao ZM, Xu YM, Zhang J, et al. Effects of growth hormone on pregnancy rates of patients with thin endometrium. J Endocrinol Invest. 2019;42:27–35.
Huang QY, Rong MH, Lan AH, Lin XM, Lin XG, He RQ, et al. The impact of atosiban on pregnancy outcomes in women undergoing in vitro fertilization-embryo transfer: a meta-analysis. PLoS One. 2017;12:e175501.
Sher G, Fisch JD. Effect of vaginal sildenafil on the outcome of in vitro fertilization (IVF) after multiple IVF failures attributed to poor endometrial development. Fertil Steril. 2002;78:1073–6.
Abdolmohammadi-Vahid S, Pashazadeh F, Pourmoghaddam Z, Aghebati-Maleki L, Abdollahi-Fard S, Yousefi M. The effectiveness of IVIG therapy in pregnancy and live birth rate of women with recurrent implantation failure (RIF): a systematic review and meta-analysis. J Reprod Immunol. 2019;134-135:28–33.
Heilmann L, Schorsch M, Hahn T. CD3-CD56+CD16+ natural killer cells and improvement of pregnancy outcome in IVF/ICSI failure after additional IVIG-treatment. Am J Reprod Immunol. 2010;63:263–5.
Moraru M, Carbone J, Alecsandru D, Castillo-Rama M, Garcia-Segovia A, Gil J, et al. Intravenous immunoglobulin treatment increased live birth rate in a Spanish cohort of women with recurrent reproductive failure and expanded CD56(+) cells. Am J Reprod Immunol. 2012;68:75–84.
Qin Q, Chang H, Zhou S, Zhang S, Yuan D, Yu LL, et al. Intrauterine administration of peripheral blood mononuclear cells activated by human chorionic gonadotropin in patients with repeated implantation failure: a meta-analysis. J Reprod Immunol. 2021;145:103323.
Yu N, Yan W, Yin T, Wang Y, Guo Y, Zhou D, et al. HCG-activated human peripheral blood mononuclear cells (PBMC) promote trophoblast cell invasion. PLoS One. 2015;10:e125589.
Alves R, Grimalt R. A review of platelet-rich plasma: history, biology, mechanism of action, and classification. Skin Appendage Disord. 2018;4:18–24.
Amable PR, Carias RB, Teixeira MV, Da CPI, Correa DAR, Granjeiro JM, et al. Platelet-rich plasma preparation for regenerative medicine: optimization and quantification of cytokines and growth factors. Stem Cell Res Ther. 2013;4:67.
Law BK. Rapamycin: an anti-cancer immunosuppressant? Crit Rev Oncol Hematol. 2005;56:47–60.
Wang WJ, Hao CF, Yi-Lin YGJ, Bao SH, Qiu LH, et al. Increased prevalence of T helper 17 (Th17) cells in peripheral blood and decidua in unexplained recurrent spontaneous abortion patients. J Reprod Immunol. 2010;84:164–70.
Kopf H, de la Rosa GM, Howard OM, Chen X. Rapamycin inhibits differentiation of Th17 cells and promotes generation of FoxP3+ T regulatory cells. Int Immunopharmacol. 2007;7:1819–24.
Karres I, Kremer JP, Dietl I, Steckholzer U, Jochum M, Ertel W. Chloroquine inhibits proinflammatory cytokine release into human whole blood. Am J Physiol. 1998;274:R1058–64.
Bygbjerg IC, Svenson M, Theander TG, Bendtzen K. Effect of antimalarial drugs on stimulation and interleukin 2 production of human lymphocytes. Int J Immunopharmacol. 1987;9:513–9.
van den Borne BE, Dijkmans BA, De Rooij HH, Le Cessie S, Verweij CL. Chloroquine and hydroxychloroquine equally affect tumor necrosis factor-alpha, interleukin 6, and interferon-gamma production by peripheral blood mononuclear cells. J Rheumatol. 1997;24:55–60.
Weber SM, Levitz SM. Chloroquine interferes with lipopolysaccharide-induced TNF-alpha gene expression by a nonlysosomotropic mechanism. J Immunol. 2000;165:1534–40.
Sadeghpour S, Ghasemnejad BM, Nazarian H, Ghasemnejad T, Nematollahi MH, Abroon S, et al. Effects of treatment with hydroxychloroquine on the modulation of Th17/Treg ratio and pregnancy outcomes in women with recurrent implantation failure: clinical trial. Immunopharmacol Immunotoxicol. 2020;42:632–42.
Chen JR, Cheng JG, Shatzer T, Sewell L, Hernandez L, Stewart CL. Leukemia inhibitory factor can substitute for nidatory estrogen and is essential to inducing a receptive uterus for implantation but is not essential for subsequent embryogenesis. Endocrinology. 2000;141:4365–72.
Stewart CL, Kaspar P, Brunet LJ, Bhatt H, Gadi I, Kontgen F, et al. Blastocyst implantation depends on maternal expression of leukaemia inhibitory factor. Nature. 1992;359:76–9.
Binette JP, Ohishi H, Burgi W, Kimura A, Suyemitsu T, Seno N, et al. The content and distribution of glycosaminoglycans in the ejaculates of normal and vasectomized men. Andrologia. 1996;28:145–9.
Eppig JJ. FSH stimulates hyaluronic acid synthesis by oocyte-cumulus cell complexes from mouse preovulatory follicles. Nature. 1979;281:483–4.
Grimek HJ, Bellin ME, Ax RL. Characteristics of proteoglycans isolated from small and large bovine ovarian follicles. Biol Reprod. 1984;30:397–409.
Campbell S, Swann HR, Aplin JD, Seif MW, Kimber SJ, Elstein M. CD44 is expressed throughout pre-implantation human embryo development. Hum Reprod. 1995;10:425–30.
Carson DD, Dutt A, Tang JP. Glycoconjugate synthesis during early pregnancy: hyaluronate synthesis and function. Dev Biol. 1987;120:228–35.
San MS, Soto-Suazo M, Zorn TM. Distribution of versican and hyaluronan in the mouse uterus during decidualization. Braz J Med Biol Res. 2003;36:1067–71.
Friedler S, Schachter M, Strassburger D, Esther K, Ron ER, Raziel A. A randomized clinical trial comparing recombinant hyaluronan/recombinant albumin versus human tubal fluid for cleavage stage embryo transfer in patients with multiple IVF-embryo transfer failure. Hum Reprod. 2007;22:2444–8.
DeMeestere I, Barlow P, Leroy F. Hardening of zona pellucida of mouse oocytes and embryos in vivo and in vitro. Int J Fertil Womens Med. 1997;42:219–22.
Carroll J, Depypere H, Matthews CD. Freeze-thaw-induced changes of the zona pellucida explains decreased rates of fertilization in frozen-thawed mouse oocytes. J Reprod Fertil. 1990;90:547–53.
Mastenbroek S, Twisk M, van der Veen F, Repping S. Preimplantation genetic screening: a systematic review and meta-analysis of RCTs. Hum Reprod Update. 2011;17:454–66.
Mirkin S, Arslan M, Churikov D, Corica A, Diaz JI, Williams S, et al. In search of candidate genes critically expressed in the human endometrium during the window of implantation. Hum Reprod. 2005;20:2104–17.
Almog B, Shalom-Paz E, Dufort D, Tulandi T. Promoting implantation by local injury to the endometrium. Fertil Steril. 2010;94:2026–9.
Zhou L, Li R, Wang R, Huang HX, Zhong K. Local injury to the endometrium in controlled ovarian hyperstimulation cycles improves implantation rates. Fertil Steril. 2008;89:1166–76.
Mao X, Zhang J, Chen Q, Kuang Y, Zhang S. Short-term copper intrauterine device placement improves the implantation and pregnancy rates in women with repeated implantation failure. Fertil Steril. 2017;108:55–61.
Loutradis D, Drakakis P, Dallianidis K, Bletsa SR, Milingos S, Doumplis N, et al. A double embryo transfer on days 2 and 4 or 5 improves pregnancy outcome in patients with good embryos but repeated failures in IVF or ICSI. Clin Exp Obstet Gynecol. 2004;31:63–6.
Acknowledgements
We would like to thank the RIF patients participated in the included studies and all researchers.
Funding
This study was supported by Major Clinical Research Projects of the Second Affiliated Hospital, Air Force Medical University (2021LCYJ004), and was also supported by National Natural Science Foundation of China (82204152). The funders had no influence on the data collection, analyses or conclusions of the study, and the views expressed in the study were from all the authors themselves and not related to the funders. All authors declared that there were no conflicts of interests in the study.
Author information
Authors and Affiliations
Contributions
XHW and YNH conceived and designed the study. YNH, RNT, and HKY selected articles and extracted the data. RNT, YNH, HM, and WWW analyzed the data. YNH, RNT, HBJ, HM, and HKY wrote the manuscript. JD, LW, SQC, and XHW contributed to the writing of final version of the manuscript. All authors agreed and reviewed the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 49080 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
He, Y., Tang, R., Yu, H. et al. Comparative effectiveness and safety of 36 therapies or interventions for pregnancy outcomes with recurrent implantation failure: a systematic review and network meta-analysis. J Assist Reprod Genet 40, 2343–2356 (2023). https://doi.org/10.1007/s10815-023-02923-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02923-8