Abstract
Endometriosis is a chronic inflammatory estrogen-dependent disease characterized by the growth of endometrial-like tissue outside the physiological region. Despite the fact that this disease is common, laparoscopic surgery is currently the gold standard in the treatment of endometriosis. In this regard, it is necessary to develop new effective methods of minimally invasive therapy for endometriosis. One of the promising areas in the treatment of endometriosis is cell therapy. Cellular therapy is a vast branch of therapeutic methods with various agents. Potential cell therapies for endometriosis may be based on the principle of targeting aspects of the pathogenesis of the disease: suppression of estrogen receptor activity, angiogenesis, fibrosis, and a decrease in the content of stem cells in endometriosis foci. In addition, immune cells such as NK cells and macrophages may be promising agents for cell therapy of endometriosis. Standing apart in the methods of cell therapy is the replacement therapy of endometriosis. Thus, many studies in the field of the pathogenesis of endometriosis can shed light not only on the causes of the disease and may contribute to the development of new methods for personalized cell therapy of endometriosis.
Similar content being viewed by others
References
Han SJ, Jung SY, Wu SP, et al. Estrogen receptor β modulates apoptosis complexes and the inflammasome to drive the pathogenesis of endometriosis. Cell. 2015;163:960–74. https://doi.org/10.1016/j.cell.2015.10.034.
Koninckx PR, Ph D, Ussia A, et al. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. 2019;111:327–40. https://doi.org/10.1016/j.fertnstert.2018.10.013.
Zhang L, Xiong W, Xiong Y, et al. 17 β-Estradiol promotes vascular endothelial growth factor expression via the Wnt/β-catenin pathway during the pathogenesis of endometriosis. Mol Hum Reprod. 2016;22:526–35. https://doi.org/10.1093/molehr/gaw025.
Ding D, Liu X, Duan J, Guo SW. Platelets are an unindicted culprit in the development of endometriosis: clinical and experimental evidence. Hum Reprod. 2015;30:812–32. https://doi.org/10.1093/humrep/dev025.
Nnoaham KE, Hummelshoj L, et al. Europe PMC Funders Group impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2013;96:366–73. https://doi.org/10.1016/j.fertnstert.2011.05.090.Impact.
Matalliotakis M, Zervou MI, Matalliotaki C, et al. The role of gene polymorphisms in endometriosis. Mol Med Rep. 2017;16(5):5881–6. https://doi.org/10.3892/mmr.2017.7398.
Menni K, Facchetti L, Cabassa P. Extragenital endometriosis: assessment with MR imaging. A pictorial review. Br J Radiol. 2016;89:1060. https://doi.org/10.1259/bjr.20150672.
Kennedy S, Bergqvist A, Chapron C, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20:2698–704.
Chapron C, Marcellin L, Borghese B, Santulli P. Rethinking mechanisms, diagnosis and management of endometriosis. Nat Rev Endocrinol. 2019;15:666–82. https://doi.org/10.1038/s41574-019-0245-z.
Berker B, Seval M. Problems with the diagnosis of endometriosis. Women’s Heal. 2015;11:597–601. https://doi.org/10.2217/whe.15.44.
Singh SS, Gude K, Perdeaux E, et al. Surgical outcomes in patients with endometriosis: a systematic review. J Obstet Gynaecol Canada. 2020;42:881-888.e11. https://doi.org/10.1016/j.jogc.2019.08.004.
Avraham S, Seidman DS. Surgery versus pharmacological treatment for endometriosis. Women’s Health. 2014;10(2):161–6. https://doi.org/10.2217/WHE.13.77.
Olive DL, Pritts EA. Treatment of endometriosis. N Engl J Med. 2001;345:266–75.
Blumenfeld Z. Hormonal suppressive therapy for endometriosis may not improve patient health. Fertil Steril. 2004;81:487–92. https://doi.org/10.1016/j.fertnstert.2003.07.038.
Yang Y, Wang Y, Yang J, et al. Original study adolescent endometriosis in China: a retrospective analysis of 63 cases. J Pediatr Adolesc Gynecol. 2012;25:295–9. https://doi.org/10.1016/j.jpag.2012.03.002.
Takagi H, Takata E, Sakamoto J, et al. Malignant transformation of an ovarian endometrioma during endometriosis treatment: a case report. Case Rep Obstet Gynecol. 2018;2018:6210172. https://doi.org/10.1155/2018/6210172.
Mechsner S, Bartley J, Halis G, et al. Endometrial carcinoma using GnRH analogues therapy in endometriosis. Zentralbl Gynakol. 2002;124:478–81. https://doi.org/10.1055/s-2002-38912.
Kiisholts K, Kurrikoff K, Arukuusk P, et al. Cell-penetrating peptide and siRNA-mediated therapeutic effects on endometriosis and cancer in vitro models. Pharmaceutics. 2021;13(10):1618. https://doi.org/10.3390/pharmaceutics13101618.
Burney RO, Giudice LC. Pathogenesis and pathophysiology of endometriosis. Fertil Steril. 2012;98:1–7. https://doi.org/10.1016/j.fertnstert.2012.06.029.Pathogenesis.
Chantalat E, Valera M-C, Vaysse C, et al. Estrogen receptors and endometriosis. Int J Mol Sci. 2020;21:1–17. https://doi.org/10.3390/ijms21082815.
Huhtinen K, Desai R, Ståhle M, et al. Endometrial and endometriotic concentrations of estrone and estradiol are determined by local metabolism rather than circulating levels. J Clin Endocrinol Metab. 2012;97:4228–35. https://doi.org/10.1210/jc.2012-1154.
Pellegrini C, Gori I, Achtari C, et al. The expression of estrogen receptors as well as GREB1, c-MYC, and cyclin D1, estrogen-regulated genes implicated in proliferation, is increased in peritoneal endometriosis. Fertil Steril. 2012;98:1200–8. https://doi.org/10.1016/j.fertnstert.2012.06.056.
Burns KA, Rodriguez KF, Hewitt SC, et al. Role of estrogen receptor signaling required for endometriosis-like lesion establishment in a mouse model. Endocrinology. 2012;153:3960–71. https://doi.org/10.1210/en.2012-1294.
Patel BG, Rudnicki M, Yu J, et al. Progesterone resistance in endometriosis: origins, consequences and interventions. Acta Obstet Gynecol Scand. 2017;96:623–32. https://doi.org/10.1111/aogs.13156.
Machairiotis N, Vasilakaki S, Thomakos N. Inflammatory mediators and pain in endometriosis: a systematic review. Biomedicines. 2021;9(1):54. https://doi.org/10.3390/biomedicines9010054.
Lin Y-H, Chen Y-H, Chang H-Y, et al. Chronic niche inflammation in endometriosis-associated infertility: current understanding and future therapeutic strategies. Int J Mol Sci. 2018;19(8):2385. https://doi.org/10.3390/ijms19082385.
Wang X, Jia Y, Li D, et al. The abundance and function of neutrophils in the endometriosis systemic and pelvic microenvironment. Mediators Inflamm. 2023;2023:1481489. https://doi.org/10.1155/2023/1481489.
Huang Y, Li Q, Hu R, et al. Five immune-related genes as diagnostic markers for endometriosis and their correlation with immune infiltration. Front Endocrinol (Lausanne). 2022;13:1011742. https://doi.org/10.3389/fendo.2022.1011742.
Chen L, Wang X, Shu J, et al. Diagnostic value of serum D-dimer, CA125, and neutrophil-to-lymphocyte ratio in differentiating ovarian cancer and endometriosis. Int J Gynecol Obstet. 2019;147:212–8. https://doi.org/10.1002/ijgo.12949.
Arici A. Local cytokines in endometrial tissue: the role of interleukin-8 in the pathogenesis of endometriosis. Ann N Y Acad Sci. 2009;955:101–9.
Di Carlo C, Bonifacio M, Tommaselli GA, et al. Metalloproteinases, vascular endothelial growth factor, and angiopoietin 1 and 2 in eutopic and ectopic endometrium. Fertil Steril. 2009;91:2315–23. https://doi.org/10.1016/j.fertnstert.2008.03.079.
Selam B, Kayisli UA, Garcia-Velasco JA, et al. Regulation of Fas ligand expression by IL-8 in human endometrium. J Clin Endocrinol Metab. 2002;87:3921–7. https://doi.org/10.1210/jcem.87.8.8713.
Shi JL, Zheng ZM, Chen M, et al. IL-17: an important pathogenic factor in endometriosis. Int J Med Sci. 2022;19:769–78. https://doi.org/10.7150/ijms.71972.
Jaillon S, Ponzetta A, Di Mitri D, et al. Neutrophil diversity and plasticity in tumour progression and therapy. Nat Rev Cancer. 2020;20:485–503. https://doi.org/10.1038/s41568-020-0281-y.
Berbic M, Hey-Cunningham AJ, Ng C, et al. The role of Foxp3+ regulatory T-cells in endometriosis: a potential controlling mechanism for a complex, chronic immunological condition. Hum Reprod. 2010;25:900–7. https://doi.org/10.1093/humrep/deq020.
Abramiuk M, Grywalska E, Małkowska P, et al. The role of the immune system in the development of endometriosis. Cells. 2022;11:1–23. https://doi.org/10.3390/cells11132028.
Tanaka Y, Mori T, Ito F, et al. Exacerbation of endometriosis due to regulatory t-cell dysfunction. J Clin Endocrinol Metab. 2017;102:3206–17. https://doi.org/10.1210/jc.2017-00052.
Xiao F, Liu X, Guo SW. Platelets and regulatory T cells may induce a type 2 immunity that is conducive to the progression and fibrogenesis of endometriosis. Front Immunol. 2020;11:610963. https://doi.org/10.3389/fimmu.2020.610963.
Wu M-H, Hsiao K-Y, Tsai S-J. Endometriosis and possible inflammation markers. Gynecol Minim Invasive Ther. 2015;4:61–7. https://doi.org/10.1016/j.gmit.2015.05.001.
Matsuzaki S, Pouly JL, Canis M. Dose-dependent pro- or anti-fibrotic responses of endometriotic stromal cells to interleukin-1β and tumor necrosis factor α. Sci Rep. 2020;10:1–12. https://doi.org/10.1038/s41598-020-66298-x.
Braga TT, Agudelo JSH, Camara NOS. Macrophages during the fibrotic process: M2 as friend and foe. Front Immunol. 2015;6:1–8. https://doi.org/10.3389/fimmu.2015.00602.
Wynn TA. Cellular and molecular mechanisms of fibrosis. J Pathol. 2008;214:199–210. https://doi.org/10.1002/path.2277.
Zhang Q, Duan J, Liu X, Guo S-W. Platelets drive smooth muscle metaplasia and fibrogenesis in endometriosis through epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation. Mol Cell Endocrinol. 2016;428:1–16. https://doi.org/10.1016/j.mce.2016.03.015.
Vigano P, Candiani M, Monno A, et al. Time to redefine endometriosis including its pro-fibrotic nature. Hum Reprod. 2018;33:347–52. https://doi.org/10.1093/humrep/dex354.
Lebovic DI, Bentzien F, Chao VA, et al. Induction of an angiogenic phenotype in endometriotic stromal cell cultures by interleukin-1beta. Mol Hum Reprod. 2000;6:269–75. https://doi.org/10.1093/molehr/6.3.269.
Chung MS, Han SJ. Endometriosis-associated angiogenesis and anti-angiogenic therapy for endometriosis. Front Glob Women’s Heal. 2022;3:1–11. https://doi.org/10.3389/fgwh.2022.856316.
Rocha ALL, Reis FM, Taylor RN. Angiogenesis and endometriosis. Endometr Sci Pract. 2013;2013:190–9. https://doi.org/10.1002/9781444398519.ch19.
Liu H, Zhang Z, Xiong W, et al. Hypoxia-inducible factor-1α promotes endometrial stromal cells migration and invasion by upregulating autophagy in endometriosis. Reproduction. 2017;153:809–20. https://doi.org/10.1530/REP-16-0643.
Li J, Li SX, Gao XH, et al. HIF1A and VEGF regulate each other by competing endogenous RNA mechanism and involve in the pathogenesis of peritoneal fibrosis. Pathol Res Pract. 2019;215:644–52. https://doi.org/10.1016/j.prp.2018.12.022.
Masuda H, Kalka C, Takahashi T, et al. Estrogen-mediated endothelial progenitor cell biology and kinetics for physiological postnatal vasculogenesis. Circ Res. 2007;101:598–606. https://doi.org/10.1161/CIRCRESAHA.106.144006.
Dhesi AS, Morelli SS. Endometriosis: a role for stem cells. Women’s Health. 2015;11(1):35–49. https://doi.org/10.2217/WHE.14.57.
Taylor HS. Endometrial cells derived from donor stem cells in bone marrow transplant recipients. JAMA. 2004;292(1):81–5. https://doi.org/10.1001/jama.292.1.81.
Faramarzi H, Mehrabani D, Fard M, et al. The potential of menstrual blood-derived stem cells in differentiation to epidermal lineage: a preliminary report. 2016.
Song Y, Xiao L, Fu J, et al. Increased expression of the pluripotency markers sex-determining region Y-box 2 and Nanog homeobox in ovarian endometriosis. Reprod Biol Endocrinol. 2014;12(1):42. https://doi.org/10.1186/1477-7827-12-42.
Pacchiarotti A, Caserta D, Sbracia M, Moscarini M. Expression of oct-4 and c-kit antigens in endometriosis. Fertil Steril. 2011;95:1171–3. https://doi.org/10.1016/j.fertnstert.2010.10.029.
Du H, Taylor HS. Contribution of bone marrow-derived stem cells to endometrium and endometriosis. Stem Cells. 2007;25(8):2082–6. https://doi.org/10.1634/stemcells.2006-0828.
Taniguchi F, Kaponis A, Izawa M, et al. Apoptosis and endometriosis. Front Biosci (Elite Ed). 2011;3:648–62. https://doi.org/10.2741/e277.
Beliard A, Noёl A, Foidart J-M. Reduction of apoptosis and proliferation in endometriosis. Fertil Steril. 2004;82(1):80–5. https://doi.org/10.1016/j.fertnstert.2003.11.048.
Braun DP, Ding J, Shaheen F, et al. Quantitative expression of apoptosis-regulating genes in endometrium from women with and without endometriosis. Fertil Steril. 2007;87(2):263–268. https://doi.org/10.1016/j.fertnstert.2006.06.026.
Bohl J, Goebel HH, Esinger W, et al. Komplikationen nach Zelltherapie *’ * *. Rechtsmedizin. 1989;1988:1–20.
Bordignon C, Carlo-Stella C, Colombo M, et al. Cell therapy: achievements and perspectives. Haematologica. 1999;84(12):1110–49.
El-kadiry AE, Rafei M, Shammaa R. Cell therapy: types, regulation, and clinical benefits. Front Med. 2021;8:1–24. https://doi.org/10.3389/fmed.2021.756029.
Brown C, Mckee C, Bakshi S, et al. Mesenchymal stem cells: cell therapy and regeneration potential. J Tissue Eng Regen Med. 2019;1738–1755. https://doi.org/10.1002/term.2914.
Oiseth SJ, Aziz MS. Cancer immunotherapy: a brief review of the history, possibilities, and challenges ahead. J Cancer Metastasis Treat. 2017;3:250–61. https://doi.org/10.20517/2394-4722.2017.41.
Miliotou AN, Papadopoulou LC. CAR T-cell therapy: a new era in cancer immunotherapy. Curr Pharm Biotechnol. 2018;19:5–18. https://doi.org/10.2174/1389201019666180418095526.
Bonifant CL, Jackson HJ, Brentjens RJ, Curran KJ. Toxicity and management in CAR T-cell therapy. Mol Ther - Oncolytics. 2016;3:16011. https://doi.org/10.1038/mto.2016.11.
Guillerey C, Huntington ND, Smyth MJ. Targeting natural killer cells in cancer immunotherapy. Nat Immunol. 2016;17:1025–36. https://doi.org/10.1038/ni.3518.
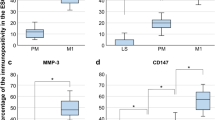
Artemova D, Vishnyakova P, Khashchenko E, et al. Endometriosis and cancer: exploring the role of macrophages. Int J Mol Sci. 2021;22:1–16. https://doi.org/10.3390/ijms22105196.
ClinicalTrials.gov Endometriosis/cell therapy. https://clinicaltrials.gov/ct2/results?cond=Endometriosis&term=cell+therapy. Accessed 27 Dec 2022.
Mechsner S. Endometriosis, an ongoing pain—step‐by‐step treatment. J Clin Med. 2022;11(2):467. https://doi.org/10.3390/jcm11020467.
Cho YJ, Lee JE, Park MJ, et al. Bufalin suppresses endometriosis progression by inducing pyroptosis and apoptosis. J Endocrinol. 2018;237:255–69. https://doi.org/10.1530/JOE-17-0700.
Kulak JJ, Fischer C, Komm B, Taylor HS. Treatment with bazedoxifene, a selective estrogen receptor modulator, causes regression of endometriosis in a mouse model. Endocrinology. 2011;152:3226–32. https://doi.org/10.1210/en.2010-1010.
Wu D, Lu P, Mi X, Miao J. Exosomal miR-214 from endometrial stromal cells inhibits endometriosis fibrosis. Mol Hum Reprod. 2018;24:357–65. https://doi.org/10.1093/molehr/gay019.
Viganò P, Ottolina J, Bartiromo L, et al. Cellular components contributing to fibrosis in endometriosis: a literature review. J Minim Invasive Gynecol. 2020;27:287–95. https://doi.org/10.1016/j.jmig.2019.11.011.
Leask A, Abraham DJ. TGF-β signaling and the fibrotic response. FASEB J. 2004;18:816–27. https://doi.org/10.1096/fj.03-1273rev.
Fan Y, Chen B, Ma X, Su M. Detection of expression of endometriosis-related cytokine and their receptor genes by cDNA microarray technique. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2005;21:489–92.
Young VJ, Ahmad SF, Duncan WC, Horne AW. The role of TGF-β in the pathophysiology of peritoneal endometriosis. Hum Reprod Update. 2017;23:548–59. https://doi.org/10.1093/HUMUPD/DMX016.
Bernacchioni C, Capezzuoli T, Vannuzzi V, et al. Sphingosine 1-phosphate receptors are dysregulated in endometriosis: possible implication in transforming growth factor β-induced fibrosis. Fertil Steril. 2021;115:501–11. https://doi.org/10.1016/j.fertnstert.2020.08.012.
Hanada T, Tsuji S, Nakayama M, et al. Suppressive regulatory T cells and latent transforming growth factor-β-expressing macrophages are altered in the peritoneal fluid of patients with endometriosis. Reprod Biol Endocrinol. 2018;16:1–8. https://doi.org/10.1186/s12958-018-0325-2.
Gurung S, Williams S, Deane JA, et al. The transcriptome of human endometrial mesenchymal stem cells under TGFβR inhibition reveals improved potential for cell-based therapies. Front Cell Dev Biol. 2018;6:1–15. https://doi.org/10.3389/fcell.2018.00164.
Zhou Y, Zhou G, Tian C, et al. Exosome-mediated small RNA delivery for gene therapy. Wiley Interdiscip Rev RNA. 2016;7:758–71. https://doi.org/10.1002/wrna.1363.
Ibrahim MG, Delarue E, Abesadze E, et al. Abdominal wall endometriosis: myofibroblasts as a possible evidence of metaplasia: a case report. Gynecol Obstet Invest. 2017;82:96–101. https://doi.org/10.1159/000452101.
Hu B, Phan SH. Myofibroblasts. Curr Opin Rheumatol. 2013;25:71–7. https://doi.org/10.1097/BOR.0b013e32835b1352.
Li J, Cen B, Chen S, He Y. MicroRNA-29b inhibits TGF-β1-induced fibrosis via regulation of the TGF-β1/Smad pathway in primary human endometrial stromal cells. Mol Med Rep. 2016;13(5):4229–37. https://doi.org/10.3892/mmr.2016.5062.
Kobayashi H. Somatic driver mutations in endometriosis as possible regulators of fibrogenesis (Review). World Acad Sci J. 2019;1(3):105–12. https://doi.org/10.3892/wasj.2019.12.
Yang J, Huang F. Stem cell and endometriosis: new knowledge may be producing novel therapies. Int J Clin Exp Med. 2014;7:3853–8.
Sakr S, Naqvi H, Komm B, Taylor HS. Endometriosis impairs bone marrow-derived stem cell recruitment to the uterus whereas bazedoxifene treatment leads to endometriosis regression and improved uterine stem cell engraftment. Endocrinology. 2014;155:1489–97. https://doi.org/10.1210/en.2013-1977.
Laschke MW, Giebels C, Nickels RM, et al. Endothelial progenitor cells contribute to the vascularization of endometriotic lesions. AJPA. 2011;178:442–50. https://doi.org/10.1016/j.ajpath.2010.11.037.
Wang X, Mamillapalli R, Mutlu L, et al. Chemoattraction of bone marrow-derived stem cells towards human endometrial stromal cells is mediated by estradiol regulated CXCL12 and CXCR4 expression. Stem Cell Res. 2015;15:14–22. https://doi.org/10.1016/j.scr.2015.04.004.Chemoattraction.
Hufnagel D, Li F, Cosar E, et al. The role of stem cells in the etiology and pathophysiology of endometriosis. Semin Reprod Med. 2015;33:333–40. https://doi.org/10.1055/s-0035-1564609.The.
Kim YS, Kim YJ, Kim MJ, et al. Novel medicine for endometriosis and its therapeutic effect in a mouse model. Biomedicines. 2020;8:1–13.
Hull ML, Charnock-Jones DS, Chan CLK, et al. Antiangiogenic agents are effective inhibitors of endometriosis. J Clin Endocrinol Metab. 2003;88:2889–99. https://doi.org/10.1210/jc.2002-021912.
Khoufache K, Bazin S, Girard K, et al. Macrophage migration inhibitory factor antagonist blocks the development of endometriosis in vivo. PLoS One. 2012;7(5):e37264. https://doi.org/10.1371/journal.pone.0037264.
Pavone ME, Malpani S, Dyson M, Bulun SE. Fenretinide: a potential treatment for endometriosis. Fertil Steril. 2014;102:e11. https://doi.org/10.1016/j.fertnstert.2014.07.044.
Hapangama DK, Turner MA, Drury JA, et al. Endometriosis is associated with aberrant endometrial expression of telomerase and increased telomere length. Hum Reprod. 2008;23:1511–9.
Alnafakh R, Choi F, Bradfield A, et al. Endometriosis is associated with a significant increase in hTERC and altered telomere/telomerase associated genes in the eutopic endometrium, an ex-vivo and in silico study. Biomedicines. 2020;8(12):588. https://doi.org/10.3390/biomedicines8120588.
Sofiyeva N, Ekizoglu S, Gezer A, et al. Does telomerase activity have an effect on infertility in patients with endometriosis? Eur J Obstet Gynecol Reprod Biol. 2017;213:116–22. https://doi.org/10.1016/j.ejogrb.2017.04.027.
Mormile R, Vittori G. MAPK signaling pathway and endometriosis: what is the link? Arch Gynecol Obstet. 2013;287:837–8.
Yotova IY, Quan P, Leditznig N, et al. Abnormal activation of Ras/Raf/MAPK and RhoA/ROCKII signalling pathways in eutopic endometrial stromal cells of patients with endometriosis. Hum Reprod. 2011;26:885–97. https://doi.org/10.1093/humrep/der010.
Zhou W-D, Yang H-M, Wang Q, et al. SB203580, a p38 mitogen-activated protein kinase inhibitor, suppresses the development of endometriosis by down-regulating proinflammatory cytokines and proteolytic factors in a mouse model. Hum Reprod. 2010;25:3110–6. https://doi.org/10.1093/humrep/deq287.
Zhang Y, Yan J, Pan X. miR-141-3p affects apoptosis and migration of endometrial stromal cells by targeting KLF-12. Pflugers Arch. 2019;471:1055–63. https://doi.org/10.1007/s00424-019-02283-2.
Wang S, Zhang M, Zhang T, et al. microRNA-141 inhibits TGF-β1-induced epithelial-to-mesenchymal transition through inhibition of the TGF-β1/SMAD2 signalling pathway in endometriosis. Arch Gynecol Obstet. 2020;301:707–14. https://doi.org/10.1007/s00404-019-05429-w.
Lebovic DI, Mueller MD, Taylor RN. Immunobiology of endometriosis. Fertil Steril. 2001;75:1–10. https://doi.org/10.1016/S0015-0282(00)01630-7.
Evert JH, Paap R, Nap A, Molen R Van Der. The promises of natural killer cell therapy in endometriosis. Int J Mol Sci. 2022;23(10):5539. https://doi.org/10.3390/ijms23105539.
Jeung I, Cheon K, Kim M-R. Decreased cytotoxicity of peripheral and peritoneal natural killer cell in endometriosis. Biomed Res Int. 2016;2016:2916070. https://doi.org/10.1155/2016/2916070.
Paul S, Lal G. The molecular mechanism of natural killer cells function and its importance in cancer immunotherapy. Front Immunol. 2017; 8:1124. https://doi.org/10.3389/fimmu.2017.01124.
Li Y, Sun R. Tumor immunotherapy: new aspects of natural killer cells. Chin J Cancer Res. 2018;30:173–96. https://doi.org/10.21147/j.issn.1000-9604.2018.02.02.
Pan P, Kang S, Wang Y, et al. Black raspberries enhance natural killer cell infiltration into the colon and suppress the progression of colorectal cancer. Front Immunol. 2017;8:997. https://doi.org/10.3389/fimmu.2017.00997.
Du Y, Liu X, Guo S-W. Platelets impair natural killer cell reactivity and function in endometriosis through multiple mechanisms. Hum Reprod. 2017;32:794–810. https://doi.org/10.1093/humrep/dex014.
ClinicalTrials.gov. Hui Qi Clinical study of NK cells in the treatment of severe endometriosis. 2019. https://clinicaltrials.gov/ct2/show/NCT03948828?cond=endometriosis+nk+cell+therapy&draw=2&rank=1. Accessed 30 Dec 2022.
Fuchs TA, Brill A, Wagner DD. Neutrophil extracellular trap (NET) impact on deep vein thrombosis. Arterioscler Thromb Vasc Biol. 2012;32:1777–83. https://doi.org/10.1161/ATVBAHA.111.242859.
Lukács L, Kovács AR, Pál L, et al. Evaluating the phagocytic index of peripheral leukocytes in endometriosis by plasma experiments. Medicina. 2022;58(7):925. https://doi.org/10.3390/medicina58070925.
Bao C, Wang H, Fang H. Genomic evidence supports the recognition of endometriosis as an inflammatory systemic disease and reveals disease-specific therapeutic potentials of targeting neutrophil degranulation. Front Immunol. 2022;13:1–17. https://doi.org/10.3389/fimmu.2022.758440.
He J, Xu Y, Yi M, et al. Involvement of natural killer cells in the pathogenesis of endometriosis in patients with pelvic pain. J Int Med Res. 2020;48(7):030006051987140. https://doi.org/10.1177/0300060519871407
Bacci M, Capobianco A, Monno A, et al. Macrophages are alternatively activated in patients with endometriosis and required for growth and vascularization of lesions in a mouse model of disease. Am J Pathol. 2009;175:547–56. https://doi.org/10.2353/ajpath.2009.081011.
Nisolle M, Alvarez M-L, Colombo M, Foidart J-M. Pathogenèse de l’endométriose. Gynécologie Obs Fertil. 2007;35:898–903. https://doi.org/10.1016/j.gyobfe.2007.07.021.
Zhang F, Ayaub EA, Wang B, et al. Reprogramming of profibrotic macrophages for treatment of bleomycin-induced pulmonary fibrosis. EMBO Mol Med. 2020;12(8):e12034. https://doi.org/10.15252/emmm.202012034.
Doss MX, Koehler CI, Gissel C, et al. Embryonic stem cells: a promising tool for cell replacement therapy. J Cellural Mol Med. 2004;8:465–73.
Efrat S. Cell replacement therapy for type 1 diabetes. Trends Mol Med. 2002;8:334–40. https://doi.org/10.1016/S1471-4914(02)02365-1.
Xu C, Police S, Rao N, Carpenter MK. Characterization and enrichment of cardiomyocytes derived from human embryonic stem cells. Circ Res. 2002;91:501–8. https://doi.org/10.1161/01.RES.0000035254.80718.91.
Barberi T, Klivenyi P, Calingasan NY, et al. Neural subtype specification of fertilization and nuclear transfer embryonic stem cells and application in parkinsonian mice. Nat Biotechnol. 2003;21:1200–7. https://doi.org/10.1038/nbt870.
Miyazaki K, Dyson MT, Coon VJS, et al. Generation of progesterone-responsive endometrial stromal fibroblasts from human induced pluripotent stem cells: role of the WNT/CTNNB1 pathway. Stem Cell Reports. 2018;11:1136–55. https://doi.org/10.1016/j.stemcr.2018.10.002.
Tinker AV, Hirte HW, Provencher D, et al. Dose-ranging and cohort-expansion study of monalizumab (IPH2201) in patients with advanced gynecologic malignancies: a trial of the Canadian Cancer Trials Group (CCTG): IND221. Clin Cancer Res. 2019;25(20):6052–60. https://doi.org/10.1158/1078-0432.CCR-19-0298.
Laganà AS, Garzon S, Götte M, Viganò P, Franchi M, Ghezzi FMD. The pathogenesis of endometriosis: molecular and cell biology insights. Int J Mol Sci. 2019;20(22):5615. https://doi.org/10.3390/ijms20225615.
Funding
Part of the work concerning endometriosis was supported by a grant for young Russian scientists MK-1573.2022.3. This paper has been supported by the PFUR University Strategic Academic Leadership Program. Part of the work concerning macrophages was supported by Russian Science Foundation [grant number 22-14-00152].
Author information
Authors and Affiliations
Contributions
Daria Artemova, Polina Vishnyakova, Elena Gantsova, Andrey Elchaninov, Timur Fatkhudinov, Gennady Sukhikh had the idea for the article. Daria Artemova, Polina Vishnyakova performed the literature search and data analysis. Daria Artemova, Polina Vishnyakova, Elena Gantsova, Andrey Elchaninov drafted the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The all authors claim no conflict of interest. The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Artemova, D., Vishnyakova, P., Gantsova, E. et al. The prospects of cell therapy for endometriosis. J Assist Reprod Genet 40, 955–967 (2023). https://doi.org/10.1007/s10815-023-02772-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02772-5