Abstract
Purpose
To assess oncofertility content on fertility clinic websites as indicated by eight relevant keywords. Additionally, we sought to describe the relationship between oncofertility content and five predetermined clinic characteristics.
Methods
We examined 381 fertility clinic websites that are members of the Society for Associated Reproductive Technology (SART). Extracted data included clinic location, practice type (private vs academic), size (cycles/year), type of NCI designated center (cancer center vs comprehensive cancer center), and distance from the nearest NCI center. Additionally, we documented whether the clinic was located in a state mandating reproductive and infertility services and/or included fertility preservation for “iatrogenic infertility” as reported by the American Society for Reproductive Medicine (ASRM). Data were summarized using descriptive statistics and compared using chi-squared or t-test as appropriate.
Results
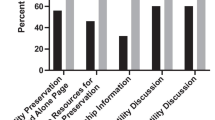
Of the 381 fertility clinic websites analyzed, 322 (85%) contained at least one oncofertility-related keyword. Most frequently used terms included cancer (79%) and fertility preservation (78%), while less frequently used terms included suppression (9.4%) and shielding (5.0%). Practices that initiated ≥ 501 cycles per year were more likely to mention one of the oncofertility keywords (OR 1.2; 95% CI 1.1–1.3). The associations of oncofertility website content with practice type, state-mandated fertility insurance coverage, and distance from an NCI-designated cancer center were not statistically significant. Large clinic size was the only predictive factor for inclusion of oncofertility website content. Further studies are required to evaluate whether inclusion of oncofertility content on clinic websites impacts the use of these services by patients with cancer.
Conclusion
This is the first study correlating availability of oncofertility content on SART fertility clinic websites with consideration of geographic proximity to NCI designated cancer centers. Large clinic size was the only predictive factor for inclusion of oncofertility website content.
Similar content being viewed by others
Data availability
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Code availability
Not applicable.
References
“Cancer Among Children, Adolescents, and Young Adults.” Centers for Disease Control and Prevention, Division of Cancer Prevention and Control. 2020. www.cdc.gov/cancer/annual-report/children-aya.htm. Accessed 12 February 2021.
Lambertini M, et al. Cancer and fertility preservation: international recommendations from an expert meeting. BMC Med. 2016;14(1):4. https://doi.org/10.1186/s12916-015-0545-7.
Loren AW, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500–10. https://doi.org/10.1200/JCO.2013.49.2678.
Runco DV, et al. Ethical barriers in adolescent oncofertility counseling. J Pediatr Hematol Oncol. 2017;39(1):56–61. https://doi.org/10.1097/MPH.0000000000000713.
Woodruff TK. Oncofertility: a grand collaboration between reproductive medicine and oncology. Reproduction (Cambridge, England). 2015;150(3):S1-10. https://doi.org/10.1530/REP-15-0163.
Abusief M, et al. Assessment of United States fertility clinic websites according to the American Society for Reproductive Medicine (ASRM)/Society for Assisted Reproductive Technology (SART) guidelines. Fertil Steril. 2007;87(1):88–92. https://doi.org/10.1016/j.fertnstert.2006.05.073.
“Gynecologic issues in children and adolescent cancer patients and survivors.” ACOG Committee Opinion, ACOG, Aug. 2018. Accessed 12 February 2021.
Oktay K, et al. Fertility preservation in patients with cancer: ASCO clinical practice guideline update summary. J Oncol Pract. 2018;14(6):381–5. https://doi.org/10.1200/jop.18.00160.
Jones G, et al. What factors hinder the decision-making process for women with cancer and contemplating fertility preservation treatment? Hum Reprod Update. 2017;23(4):433–57. https://doi.org/10.1093/humupd/dmx009.
Ruddy KJ, et al. Prospective study of fertility concerns and preservation strategies in young women with breast cancer. J Clin Oncol. 2014;32(11):1151–6. https://doi.org/10.1200/JCO.2013.52.8877.
Anazodo A, et al. How can we improve oncofertility care for patients? A systematic scoping review of current international practice and models of care. Hum Reprod Update. 2019;25(2):159–79. https://doi.org/10.1093/humupd/dmy038.
Jin H, Dasgupta S. Disparities between online assisted reproduction patient education for same-sex and heterosexual couples. Hum Reprod (Oxford, England). 2016;31(10):2280–4. https://doi.org/10.1093/humrep/dew182.
Hesse BW, et al. Surveys of physicians and electronic health information. N Engl J Med. 2010;362(9):859–60. https://doi.org/10.1056/NEJMc0909595.
Kim J, et al. Fertility preservation consultation for women with cancer: are we helping patients make high-quality decisions? Reprod Biomed Online. 2013;27(1):96–103. https://doi.org/10.1016/j.rbmo.2013.03.004.
“NCI-Designated Cancer Centers.” National Cancer Institute, National Cancer Institute at the National Institutes of Health, www.cancer.gov/research/infrastructure/cancer-centers, June 2019. Accessed 20 October 2020.
Onega T, et al. Influence of NCI cancer center attendance on mortality in lung, breast, colorectal, and prostate cancer patients. Med Care Res Rev: MCRR. 2009;66(5):542–60. https://doi.org/10.1177/1077558709335536.
Hoyos-Martinez, A, et al. “Availability of Fertility Preservation Information on the Websites of U.S. News and World Report Top-Ranked Pediatric Cancer Programs. J Adolesc Young Adult Oncol. 10 1 (2021): https://doi.org/10.1089/jayao.2020.003.
Vest AN et al. “Is fertility preservation a part of comprehensive cancer care in the USA? A study of NCI-designated cancer center websites.” J Cancer Surviv. (2021). https://doi.org/10.1007/s11764-020-00983-8. Epub ahead of print. PMID: 33454796.
Rasouli, M.A., et al. “Have oncofertility information for patients improved? Objective assessment of Internet based fertility preservation resources at NCI cancer centers from 2015–2020.” Fertil Steril, 114 3, (2020). https://doi.org/10.1016/j.fertnstert.2020.10.011.
Lopategui DM, Ibrahim E, Aballa TC, et al. Effect of a formal oncofertility program on fertility preservation rates-first year experience. Transl Androl Urol. 2018;7(3):S271–5. https://doi.org/10.21037/tau.2018.04.24.
Zalia KE, et al. Male reproductive oncofertility specialisits at NCI designated cancer centers: association of web site constent with institutional ranking and location sociodemographics. Fertil Steril. 2020;114(3):e468.
Skinner, E. State laws related to insurance coverage for infertility treatment. https://www.ncsl.org/research/health/insurance-coverage-for-infertility-laws.aspx, 2021. Accessed 1 March 2021.
“Discover infertility treatment coverage by U.S. state.” RESOLVE https://resolve.org/what-are-my-options/insurance-coverage/infertility-coverage-state/, 2021. Accessed 1 March 2021.
“State Legislation - California.” Alliance for Fertility Preservation, https://www.allianceforfertilitypreservation.org/state-legislation/california, 2019. Accessed 1 March 2021.
“Fertility Preservation for Cancer Patients Covered In CA - NCFMC.” Northern California Fertility Medical Center - Sacramento IVF, https://ncfmc.com/cancer-fertility-preservation/?cn-reloaded=1, 2019. Accessed 1 March 2021.
“Senate Bill No. 600.” Bill Text - SB-600 Health care coverage: fertility preservation. https://leginfo.legislature.ca.gov/faces/billTextClient.xhtml?bill_id=201920200SB600, 2019. Accessed 1 March 2021.
Fujimoto VY, et al. Racial and ethnic disparities in assisted reproductive technology outcomes in the United States. Fertil Steril. 2010;93(2):382–90. https://doi.org/10.1016/j.fertnstert.2008.10.061.
Londra, LC, et al. “Spanish language content on reproductive endocrinology and infertility practice websites.” Fertil Steril. 102 5, (2014). https://doi.org/10.1016/j.fertnstert.2014.07.1243.
Gates, G. LGBT demographics: comparisons among population-based surveys. Los Angeles: Williams Institute, University of California Los Angeles School of Law, https://williamsinstitute.law.ucla.edu/wp-content/uploads/LGBT-Demographics-Comparison-Oct-2014.pdf, 2014. Accessed 20 October 2020.
Wu HY, et al. Lesbian, gay, bisexual, transgender content on reproductive endocrinology and infertility clinic websites. Fertil Steril. 2017;108(1):183–91. https://doi.org/10.1016/j.fertnstert.2017.05.011.
Dorfman CS, Stalls JM, Mills C, et al. Addressing barriers to fertility preservation for cancer patients: the role of oncofertility patient navigation. J Oncol Navig Surviv. 2021;12(10):332–48.
Acknowledgements
We thank Rebecca J. Mercier, MD, MPH (Thomas Jefferson University Hospitals) for assistance in conceptualizing methodology and Brandie Plasencia RN, BSN (Stanford Hospitals and Clinics) for review and revision of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conception or design of the work; acquisition, analysis, or interpretation of data; or revised the manuscript critically for important intellectual content.
Corresponding author
Ethics declarations
Ethics approval
This study was granted exemption from requiring ethics approval due to its utilization of public access online data.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mujumdar, V., Shivashankar, K., Madding, R. et al. An assessment of oncofertility content on reproductive endocrinology and infertility clinic websites. J Assist Reprod Genet 39, 957–962 (2022). https://doi.org/10.1007/s10815-022-02442-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02442-y