Abstract
Objective
To compare the prevalence of chromosomal abnormalities detected in products of conception (POCs) between recurrent pregnancy loss and sporadic pregnancy loss.
Methods
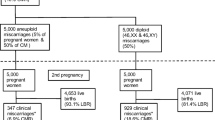
A systematic search was performed in the PubMed and Embase databases from inception to December 31, 2020. Relevant studies analysing the association between the number of pregnancy losses and the incidence of chromosomal abnormalities were included. Independent data extraction was conducted and study quality was assessed. Meta-analyses were carried out to calculate odds ratios by using fixed- or random-effects models according to statistical homogeneity.
Results
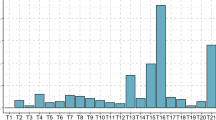
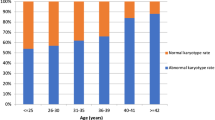
A total of 8320 POCs in 19 studies were identified for the meta-analyses. The incidence of chromosomal abnormalities in sporadic pregnancy loss was significantly higher than that in recurrent pregnancy loss. In subgroup analyses, the following studies reported a high incidence of abnormal outcomes of sporadic pregnancy loss: studies with ≥ 300 samples, studies published before 2014, studies conducted in European and American countries, and studies with analyses using conventional karyotype techniques. Moreover, the incidence of chromosomal abnormalities in women with two pregnancy losses was significantly higher than that in women with three or more pregnancy losses. However, there was no difference in the distribution of abnormal types between sporadic and recurrent pregnancy loss or between two and three or more pregnancy losses.
Conclusions
The prevalence of chromosomal abnormalities detected in POCs was lower in recurrent pregnancy loss than in sporadic pregnancy loss, and decreased with an increasing number of pregnancy losses.





Similar content being viewed by others
References
Bender Atik R, Christiansen OB, Elson J, Kolte AM, Lewis S, Middeldorp S, et al. ESHRE guideline: recurrent pregnancy loss. Hum Reprod Open. 2018;2018:hoy004.
Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98:1103-11.
Dimitriadis E, Menkhorst E, Saito S, Kutteh WH, Brosens JJ. Recurrent pregnancy loss. Nat Rev Dis Primers. 2020;6:98.
van Dijk MM, Kolte AM, Limpens J, Kirk E, Quenby S, van Wely M, et al. Recurrent pregnancy loss: diagnostic workup after two or three pregnancy losses? A systematic review of the literature and meta-analysis. Hum Reprod Update. 2020;26:356–67.
van den Berg MM, van Maarle MC, van Wely M, Goddijn M. Genetics of early miscarriage. Biochim Biophys Acta. 2012;1822:1951–9.
Hardy K, Hardy PJ, Jacobs PA, Lewallen K, Hassold TJ. Temporal changes in chromosome abnormalities in human spontaneous abortions: results of 40 years of analysis. Am J Med Genet A. 2016;170:2671–80.
Soler AMC, Mademont-Soler I, Margarit E, Borrell A, Borobio V, Muñoz M, Sánchez A. Overview of chromosome abnormalities in first trimester miscarriages: a series of 1,011 consecutive chorionic villi sample karyotypes. Cytogenet Genome Res. 2017;152:81–9.
Smits MAJ, van Maarle M, Hamer G, Mastenbroek S, Goddijn M, van Wely M. Cytogenetic testing of pregnancy loss tissue: a meta-analysis. Reprod Biomed Online. 2020;40:867–79.
Zhang T, Sun Y, Chen Z, Li T. Traditional and molecular chromosomal abnormality analysis of products of conception in spontaneous and recurrent miscarriage. BJOG. 2018;125:414–20.
van den Berg MM, van Maarle MC, van Wely M, Goddijn M. Genetics of early miscarriage. Biochim Biophys Acta. 2012;1822:1951–9.
An N, Li LL, Zhang XY, Sun WT, Liu MH, Liu RZ. Result and pedigree analysis of spontaneously abortion villus chromosome detecting by FISH. Genet Mol Res. 2015;14:16662–6.
Dai R, Xi Q, Wang R, Zhang H, Jiang Y, Li L, et al. Chromosomal copy number variations in products of conception from spontaneous abortion by next-generation sequencing technology. Medicine (Baltimore). 2019;98:e18041.
Fan L, Wu J, Wu Y, Shi X, Xin X, Li S, et al. Analysis of Chromosomal Copy Number in First-Trimester Pregnancy Loss Using Next-Generation Sequencing. Front Genet. 2020;11:545856.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Coulam CB, Stephenson M, Stern JJ, Clark DA. Immunotherapy for recurrent pregnancy loss: analysis of results from clinical trials. Am J Reprod Immunol. 1996;35:352–9.
Stern JJ, Dorfmann AD, Gutiérrez-Najar AJ, Cerrillo M, Coulam CB. Frequency of abnormal karyotypes among abortuses from women with and without a history of recurrent spontaneous abortion. Fertil Steril. 1996;65:250–3.
Ogasawara M, Aoki K, Okada S, Suzumori K. Embryonic karyotype of abortuses in relation to the number of previous miscarriages. Fertil Steril. 2000;73:300–4.
Hogge WA, Byrnes AL, Lanasa MC, Surti U. The clinical use of karyotyping spontaneous abortions. Am J Obstet Gynecol. 2003;189:397–400.
Sullivan AE, Silver RM, LaCoursiere DY, Porter TF, Branch DW. Recurrent fetal aneuploidy and recurrent miscarriage. Obstet Gynecol. 2004;104:784–8.
Sugiura-Ogasawara M, Ozaki Y, Kitaori T, Suzumori N, Obayashi S, Suzuki S. Live birth rate according to maternal age and previous number of recurrent miscarriages. Am J Reprod Immunol. 2009;62:314–9.
Grande M, Borrell A, Garcia-Posada R, Borobio V, Muñoz M, Creus M, et al. The effect of maternal age on chromosomal anomaly rate and spectrum in recurrent miscarriage. Hum Reprod. 2012;27:3109–17.
Robberecht C, Pexsters A, Deprest J, Fryns JP, D’Hooghe T, Vermeesch JR. Cytogenetic and morphological analysis of early products of conception following hystero-embryoscopy from couples with recurrent pregnancy loss. Prenat Diagn. 2012;32:933–42.
Choi TY, Lee HM, Park WK, Jeong SY, Moon HS. Spontaneous abortion and recurrent miscarriage: A comparison of cytogenetic diagnosis in 250 cases. Obstet Gynecol Sci. 2014;57:518–25.
Nikitina TV, Sazhenova EA, Tolmacheva EN, Sukhanova NN, Kashevarova AA, Skryabin NA, et al. Comparative cytogenetic analysis of spontaneous abortions in recurrent and sporadic pregnancy losses. Biomed Hub. 2016;1:1–11.
Goldstein M, Svirsky R, Reches A, Yaron Y. Does the number of previous miscarriages influence the incidence of chromosomal aberrations in spontaneous pregnancy loss? J Matern Fetal Neonatal Med. 2017;30:2956–60.
Segawa T, Kuroda T, Kato K, Kuroda M, Omi K, Miyauchi O, et al. Cytogenetic analysis of the retained products of conception after missed abortion following blastocyst transfer: a retrospective, large-scale, single-centre study. Reprod Biomed Online. 2017;34:203–10.
Wang Y, Cheng Q, Meng L, Luo C, Hu H, Zhang J, et al. Clinical application of SNP array analysis in first-trimester pregnancy loss: a prospective study. Clin Genet. 2017;91:849–58.
Lovrečić L, Pereza N, Jaklič H, Ostojić S, Peterlin B. Combination of QF-PCR and aCGH is an efficient diagnostic strategy for the detection of chromosome aberrations in recurrent miscarriage. Mol Genet Genomic Med. 2019;7:e980.
Ozawa N, Ogawa K, Sasaki A, Mitsui M, Wada S, Sago H. Maternal age, history of miscarriage, and embryonic/fetal size are associated with cytogenetic results of spontaneous early miscarriages. J Assist Reprod Genet. 2019;36:749–57.
Gomez R, Hafezi N, Amrani M, Schweiger S, Dewenter MK, Thomas P, et al. Genetic findings in miscarriages and their relation to the number of previous miscarriages. Arch Gynecol Obstet. 2021;303:1425–32.
Acknowledgements
This meta-analysis was performed in accordance with PRISMA guidelines. However, this work was not registered. All authors contributed substantially to the design of this meta-analysis. D.L. performed the literature search. D.L. and XY.Z. selected the studies and extracted the relevant information. PS.Z. acted as a reviewer in case consensus could not be reached directly. D.L. drafted the article. All authors critically revised the manuscript and approved the final version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lei, D., Zhang, XY. & Zheng, PS. Recurrent pregnancy loss: fewer chromosomal abnormalities in products of conception? a meta-analysis. J Assist Reprod Genet 39, 559–572 (2022). https://doi.org/10.1007/s10815-022-02414-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02414-2