Abstract
Purpose
Few studies explored whether prolonged cryo-storage after vitrification affects embryo competence and perinatal outcomes. This systematic review and meta-analysis aims at highlighting any putative impact of cryo-storage duration on cryo-survival, miscarriage, live birth and major malformations.
Methods
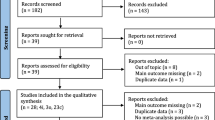
A systematic review was performed using MEDLINE (PubMed), ISI Web of Knowledge, Scopus and Embase databases up to June 2021. Data were combined to obtain a pooled OR, and meta-analysis was conducted using a random effects model. Out of 1,389 screened abstracts, 22 papers were assessed for eligibility, and 5 studies were included (N = 18,047 embryos). Prolonged cryo-storage was defined as > 12 months (N = 3389 embryos). Subgroup analysis was performed for untested vitrified cleavage stage embryos (N = 1739 embryos) and for untested and euploid vitrified blastocysts (N = 13,596 and 2712 embryos, respectively).
Results
Survival rate, miscarriage, live birth and major malformation rates were all similar in the two groups.
Conclusion
These data further support the safety of long-term cryo-storage of human embryos beyond 12 months. This is reassuring for good prognosis patients with surplus embryos, couples seeking a second child from supernumerary embryos and women postponing the transfer for clinical or personal reasons.





Similar content being viewed by others
References
Bosch E, De Vos M, Humaidan P. The future of cryopreservation in assisted reproductive technologies. Front Endocrinol (Lausanne). 2020;11:67. https://doi.org/10.3389/fendo.2020.00067.
Practice Committees of the American Society for Reproductive M, Society of Reproductive B, Technologists. Electronic address jao. A review of best practices of rapid-cooling vitrification for oocytes and embryos: a committee opinion. Fertil Steril. 2021;115(2):305–10. https://doi.org/10.1016/j.fertnstert.2020.11.017.
Practice Committees of the American Society for Reproductive Medicine SfRB, Technologists, Society for Assisted Reproductive Technology. Electronic address aao. Cryostorage of reproductive tissues in the in vitro fertilization laboratory: a committee opinion. Fertil Steril. 2020;114(3):486–91. https://doi.org/10.1016/j.fertnstert.2020.06.019.
Cobo A, Garcia-Velasco JA, Remohi J, Pellicer A. Oocyte vitrification for fertility preservation for both medical and nonmedical reasons. Fertil Steril. 2021;115(5):1091–101. https://doi.org/10.1016/j.fertnstert.2021.02.006.
Ethics Committee of the American Society for Reproductive Medicine. Electronic address aao, Ethics Committee of the American Society for Reproductive M. Planned oocyte cryopreservation for women seeking to preserve future reproductive potential: an Ethics Committee opinion. Fertil Steril. 2018;110(6):1022–8. https://doi.org/10.1016/j.fertnstert.2018.08.027.
Devroey P, Polyzos NP, Blockeel C. An OHSS-free clinic by segmentation of IVF treatment. Hum Reprod. 2011;26(10):2593–7. https://doi.org/10.1093/humrep/der251.
Zhu Q, Chen Q, Wang L, Lu X, Lyu Q, Wang Y, et al. Live birth rates in the first complete IVF cycle among 20 687 women using a freeze-all strategy. Hum Reprod. 2018;33(5):924–9. https://doi.org/10.1093/humrep/dey044.
European IVFMCftESoHR, Embryology, Wyns C, De Geyter C, Calhaz-Jorge C, Kupka MS, et al. (2021) ART in Europe, 2017: results generated from European registries by ESHRE. Hum Reprod Open. 2021;3:hoab026. https://doi.org/10.1093/hropen/hoab026.
Conforti A, Picarelli S, Carbone L, La Marca A, Venturella R, Vaiarelli A, et al. Perinatal and obstetric outcomes in singleton pregnancies following fresh versus cryopreserved blastocyst transfer: a meta-analysis. Reprod Biomed Online. 2021;42(2):401–12. https://doi.org/10.1016/j.rbmo.2020.09.029.
Vajta G, Nagy ZP. Are programmable freezers still needed in the embryo laboratory? Review on vitrification. Reprod Biomed Online. 2006;12(6):779–96.
Rienzi L, Gracia C, Maggiulli R, LaBarbera AR, Kaser DJ, Ubaldi FM, et al. Oocyte, embryo and blastocyst cryopreservation in ART: systematic review and meta-analysis comparing slow-freezing versus vitrification to produce evidence for the development of global guidance. Hum Reprod Update. 2017;23(2):139–55. https://doi.org/10.1093/humupd/dmw038.
Cobo A, de los Santos MJ, Castello D, Gamiz P, Campos P, Remohi J. Outcomes of vitrified early cleavage-stage and blastocyst-stage embryos in a cryopreservation program: evaluation of 3,150 warming cycles. Fertil Steril. 2012;98(5):1138-1146 e1. https://doi.org/10.1016/j.fertnstert.2012.07.1107.
Zaat T, Zagers M, Mol F, Goddijn M, van Wely M, Mastenbroek S. Fresh versus frozen embryo transfers in assisted reproduction. Cochrane Database Syst Rev. 2021;2:CD011184. https://doi.org/10.1002/14651858.CD011184.pub3.
Roy TK, Bradley CK, Bowman MC, McArthur SJ. Single-embryo transfer of vitrified-warmed blastocysts yields equivalent live-birth rates and improved neonatal outcomes compared with fresh transfers. Fertil Steril. 2014;101(5):1294–301. https://doi.org/10.1016/j.fertnstert.2014.01.046.
Feng G, Zhang B, Zhou H, Shu J, Gan X, Wu F, et al. Comparable clinical outcomes and live births after single vitrified-warmed and fresh blastocyst transfer. Reprod Biomed Online. 2012;25(5):466–73. https://doi.org/10.1016/j.rbmo.2012.07.008.
Edgar DH, Gook DA. A critical appraisal of cryopreservation (slow cooling versus vitrification) of human oocytes and embryos. Hum Reprod Update. 2012;18(5):536–54. https://doi.org/10.1093/humupd/dms016.
Nagy ZP, Shapiro D, Chang CC. Vitrification of the human embryo: a more efficient and safer in vitro fertilization treatment. Fertil Steril. 2020;113(2):241–7. https://doi.org/10.1016/j.fertnstert.2019.12.009.
Maheshwari A, Pandey S, Amalraj Raja E, Shetty A, Hamilton M, Bhattacharya S. Is frozen embryo transfer better for mothers and babies? Can cumulative meta-analysis provide a definitive answer? Hum Reprod Update. 2018;24(1):35–58. https://doi.org/10.1093/humupd/dmx031.
Ma Y, Liu X, Shi G, Liu Y, Zhou S, Hou W, et al. Storage time of cryopreserved embryos and pregnancy outcomes: a dose-response meta-analysis. Geburtshilfe Frauenheilkd. 2021;81(3):311–20. https://doi.org/10.1055/a-1326-1830.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. https://doi.org/10.1186/2046-4053-4-1.
Lo CK, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014;14:45. https://doi.org/10.1186/1471-2288-14-45.
Holmes LB. Current concepts in genetics Congenital malformations. N Engl J Med. 1976;295(4):204–7. https://doi.org/10.1056/NEJM197607222950406.
Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63. https://doi.org/10.1111/j.0006-341x.2000.00455.x.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. https://doi.org/10.1136/bmj.315.7109.629.
Ueno S, Uchiyama K, Kuroda T, Yabuuchi A, Ezoe K, Okimura T, et al. Cryostorage duration does not affect pregnancy and neonatal outcomes: a retrospective single-centre cohort study of vitrified-warmed blastocysts. Reprod Biomed Online. 2018;36(6):614–9. https://doi.org/10.1016/j.rbmo.2018.03.008.
Lee HN, Park JK, Paek SK, Byun JH, Song H, Lee HJ, et al. Does duration of cryostorage affect survival rate, pregnancy, and neonatal outcomes? Large-scale single-center study of slush nitrogen (SN2) vitrified-warmed blastocysts. Int J Gynaecol Obstet. 2021;152(3):351–7. https://doi.org/10.1002/ijgo.13381.
Wirleitner B, Vanderzwalmen P, Bach M, Baramsai B, Neyer A, Schwerda D, et al. The time aspect in storing vitrified blastocysts: its impact on survival rate, implantation potential and babies born. Hum Reprod. 2013;28(11):2950–7. https://doi.org/10.1093/humrep/det361.
Li W, Zhao W, Xue X, Zhang S, Zhang X, Shi J. Influence of storage time on vitrified human cleavage-stage embryos froze in open system. Gynecol Endocrinol. 2017;33(2):96–9. https://doi.org/10.1080/09513590.2016.1207166.
Cimadomo D, Fabozzi G, Dovere L, Maggiulli R, Albricci L, Innocenti F, et al. Clinical, obstetric and perinatal outcomes after vitrified-warmed euploid blastocyst transfer are independent from cryo-storage duration: analysis of 2688 procedures. Reprod Biomed Online. 2021. https://doi.org/10.1016/j.rbmo.2021.09.027.
Parmegiani L, Vajta G. The effect of cryostorage duration on vitrified embryos: has vitrification suddenly become unsafe? Hum Reprod. 2020;35(11):2632–3. https://doi.org/10.1093/humrep/deaa238.
De Santis L, Parmegiani L, Scarica C, SierrISoER, Research. Changing perspectives on liquid nitrogen use and storage. J Assist Reprod Genet. 2021;38(4):783–4. https://doi.org/10.1007/s10815-021-02102-7.
Gosden R. Cryopreservation: a cold look at technology for fertility preservation. Fertil Steril. 2011;96(2):264–8. https://doi.org/10.1016/j.fertnstert.2011.06.029.
Maxwell SM, Goldman KN, Labella PA, McCaffrey C, Noyes NL, Grifo J. Live birth in a 46 year old using autologous oocytes cryopreserved for a duration of 3 years: a case report documenting fertility preservation at an advanced reproductive age. J Assist Reprod Genet. 2014;31(6):651–5. https://doi.org/10.1007/s10815-014-0202-7.
Parmegiani L, Fabbri R, Cognigni GE, Bernardi S, Pocognoli P, Filicori M. Blastocyst formation, pregnancy, and birth derived from human oocytes cryopreserved for 5 years. Fertil Steril. 2008;90(5):2014 e7-2014 e10. https://doi.org/10.1016/j.fertnstert.2008.01.106.
Quintans CJ, Donaldson MJ, Urquiza MF, Carretero I, Pasqualini RA, Horton M, et al. Live birth of twins after IVF of oocytes that were cryopreserved almost 12 years before. Reprod Biomed Online. 2012;25(6):600–2. https://doi.org/10.1016/j.rbmo.2012.09.002.
Urquiza MF, Carretero I, Cano Carabajal PR, Pasqualini RA, Felici MM, Pasqualini RS, et al. Successful live birth from oocytes after more than 14 years of cryopreservation. J Assist Reprod Genet. 2014;31(11):1553–5. https://doi.org/10.1007/s10815-014-0318-9.
Reed ML, Hamic A, Caperton CL, Thompson DJ. Live birth after anonymous donation of twice-cryopreserved embryos that had been stored in liquid nitrogen for a cumulative storage time of approximately 13.5 years. Fertil Steril. 2010;94(7):2771 e1-2771 e3. https://doi.org/10.1016/j.fertnstert.2010.04.071.
Pruksananonda K, Rungsiwiwut R, Numchaisrika P, Ahnonkitpanit V, Isarasena N, Virutamasen P. Eighteen-year cryopreservation does not negatively affect the pluripotency of human embryos: evidence from embryonic stem cell derivation. Biores Open Access. 2012;1(4):166–73. https://doi.org/10.1089/biores.2012.0242.
Stigliani S, Moretti S, Anserini P, Casciano I, Venturini PL, Scaruffi P. Storage time does not modify the gene expression profile of cryopreserved human metaphase II oocytes. Hum Reprod. 2015;30(11):2519–26. https://doi.org/10.1093/humrep/dev232.
Huo Y, Yuan P, Qin Q, Yan Z, Yan L, Liu P, et al. Effects of vitrification and cryostorage duration on single-cell RNA-Seq profiling of vitrified-thawed human metaphase II oocytes. Front Med. 2021;15(1):144–54. https://doi.org/10.1007/s11684-020-0792-7.
Cai L. Cryo-storage time had no influence on post-thaw survival and pregnancy outcomes in vitrified human oocytes. J Assist Reprod Genet. 2013;30(2):184.
Cohen J, Inge KL, Wiker SR, Wright G, Fehilly CB Jr, Turner TG. Duration of storage of cryopreserved human embryos. J in vitro Fertil Embryo Trans. 1988;5(5):301–3.
Check JH, Summers-Chase D, Yuan W, Swenson K, Horwath D. Length of time of embryo storage does not negatively influence pregnancy rates after thawing and transfer. Clin Exp Obstet Gynecol. 2010;37(3):185–6.
Galliano D, Garrido N, Serra-Serra V, Pellicer A. Difference in birth weight of consecutive sibling singletons is not found in oocyte donation when comparing fresh versus frozen embryo replacements. Fertil Steril. 2015;104(6):1411-8 e1-3. https://doi.org/10.1016/j.fertnstert.2015.08.013.
Xu JJ, Chen L, Li C, Duan CC, Huang HF, Wu YT. Effect of embryo cryopreservation duration on pregnancy-related complications and birthweight after frozen-thawed embryo transfer: a retrospective cohort study. J Dev Orig Health Dis. 2021;2021:1–10. https://doi.org/10.1017/S2040174421000192.
Machtinger R, Dor J, Levron J, Mashiach S, Levran D, Seidman DS. The effect of prolonged cryopreservation on embryo survival. Gynecol Endocrinol. 2002;16(4):293–8.
Riggs R, Mayer J, Dowling-Lacey D, Chi TF, Jones E, Oehninger S. Does storage time influence postthaw survival and pregnancy outcome? An analysis of 11,768 cryopreserved human embryos. Fertil Steril. 2010;93(1):109–15. https://doi.org/10.1016/j.fertnstert.2008.09.084.
Aflatoonian N, Pourmasumi S, Aflatoonian A, Eftekhar M. Duration of storage does not influence pregnancy outcome in cryopreserved human embryos. Iran J Reprod Med. 2013;11(10):843–6.
Schalkoff ME, Oskowitz SP, Powers RD. A multifactorial analysis of the pregnancy outcome in a successful embryo cryopreservation program. Fertil Steril. 1993;59(5):1070–4.
Alpha Scientists In Reproductive Medicine. The Alpha consensus meeting on cryopreservation key performance indicators and benchmarks: proceedings of an expert meeting. Reprod Biomed Online. 2012;25(2):146–67. https://doi.org/10.1016/j.rbmo.2012.05.006.
Hammond ER, Foong AKM, Rosli N, Morbeck DE. Should we freeze it? Agreement on fate of borderline blastocysts is poor and does not improve with a modified blastocyst grading system. Hum Reprod. 2020. https://doi.org/10.1093/humrep/deaa060.
Simopoulou M, Sfakianoudis K, Giannelou P, Rapani A, Maziotis E, Tsioulou P, et al. Discarding IVF embryos: reporting on global practices. J Assist Reprod Genet. 2019;36(12):2447–57. https://doi.org/10.1007/s10815-019-01592-w.
Acknowledgements
We sincerely thank all authors who provided data for this analysis and especially Dr Satoshi Ueno for its contribution.
Author information
Authors and Affiliations
Consortia
Contributions
S.C., D.C., R.M. and G.F. conceived the study, drafted and edited the manuscript; A.C. performed the statistical analysis and contributed to the drafting and editing the manuscript; S.C., D.C., R.M., A.T., F.G. and A.G. conducted the study selection; G.G., A.V, A.R., C.A., F.M.U and L.R. contributed to the final interpretation of data and editing of the manuscript. All authors gave their final approval.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
S. Canosa and D. Cimadomo should be regarded as joint first authors
Supplementary Information
Rights and permissions
About this article
Cite this article
Canosa, S., Cimadomo, D., Conforti, A. et al. The effect of extended cryo-storage following vitrification on embryo competence: a systematic review and meta-analysis. J Assist Reprod Genet 39, 873–882 (2022). https://doi.org/10.1007/s10815-022-02405-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-022-02405-3



