Abstract
Purpose
Alcoholism is a heterogeneous set of disorders caused by ethanol intake. Harmful effects of paternal consumption on the offspring are poorly explored and not fully understood. We analyzed the effect of paternal alcohol consumption on both their own reproductive capacity and that of their male offspring.
Methods
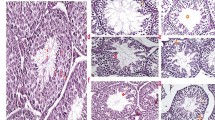
We used a model of ethanol consumption (15% v/v in drinking water) for 12 days in adult CF-1 male mice. DNA integrity and post-translational modifications of histones were assessed in sperm; testicular weight, histology, and DNA fragmentation were analyzed. Treated or untreated male mice were mated with non-treated females to obtain two cell embryos that were cultured for 7 days; morphology and embryonic cell death were evaluated. Males of both groups were mated with non-treated females. Adult male offspring was euthanized, and sperm and testicular parameters determined.
Results
Paternal ethanol consumption caused histological and epigenetic changes, as well as damage in DNA integrity in the testicular germline and sperm. These alterations gave rise to deleterious effects on embryonic development and to testicular and spermatic changes in the offspring.
Conclusion
This study provides critical information on reproductive disturbances brought about by paternal alcohol consumption and the profound impact these could have on the male progeny. The need to explore the effects of paternal alcohol consumption in detail and warn about the importance of controlling alcohol intake for the well-being of future generations should not be underscored.








Similar content being viewed by others
References
Dimijian GG. Evolution of sexuality: biology and behavior. Proc (Bayl Univ Med Cent). 2005;18(3):244–58.
Stearns SC. The evolutionary maintenance of sexual reproduction: the solutions proposed for a longstanding problem. J Genet. 1990;69(1):1–10.
Otto S. Sexual Reproduction and the Evolution of Sex. Nature Education. 2008;1:182.
Marchiani S, Tamburrino L, Benini F, et al. Chromatin protamination and catsper expression in spermatozoa predict clinical outcomes after assisted reproduction programs. Sci Rep. 2017;7(1):15122. https://doi.org/10.1038/s41598-017-15351-3.
Meyer RG, Ketchum CC, Meyer-Ficca ML. Heritable sperm chromatin epigenetics: a break to remember. Biol Reprod. 2017;97(6):784–97. https://doi.org/10.1093/biolre/iox137.
Sakkas D, Alvarez JG. Sperm DNA fragmentation: mechanisms of origin, impact on reproductive outcome, and analysis. Fertil Steril. 2010;93(4):1027–36. https://doi.org/10.1016/j.fertnstert.2009.10.046.
Henkel RR, Franken DR. Sperm DNA fragmentation: origin and impact on human reproduction. J Reprod Stem Cell Biotechnol. 2011;2(2):88–108. https://doi.org/10.1177/205891581100200204.
Asmarinah, Syauqy A, Umar LA, et al. Sperm chromatin maturity and integrity correlated to zygote development in ICSI program. Syst Biol Reprod Med. 2016;62(5):309–316. https://doi.org/10.1080/19396368.2016.1210695
Donkin I, Barrès R. Sperm epigenetics and influence of environmental factors. Mol Metab. 2018;14:1–11. https://doi.org/10.1016/j.molmet.2018.02.006.
Giacone F, Cannarella R, Mongioì LM, et al. Epigenetics of male fertility: effects on assisted reproductive techniques. World J Mens Health. 2019;37(2):148–56. https://doi.org/10.5534/wjmh.180071.
Nanassy L, Carrell DT. Paternal effects on early embryogenesis. J Exp Clin Assist Reprod. 2008;5:2. https://doi.org/10.1186/1743-1050-5-2.
Teperek M, Simeone A, Gaggioli V, et al. Sperm is epigenetically programmed to regulate gene transcription in embryos. Genome Res. 2016;26(8):1034–46. https://doi.org/10.1101/gr.201541.115.
Hammoud SS, Purwar J, Pflueger C, et al. Alterations in sperm DNA methylation patterns at imprinted loci in two classes of infertility. Fertil Steril. 2010;94(5):1728–33. https://doi.org/10.1016/j.fertnstert.2009.09.010.
Knezovich JG, Ramsay M. The effect of preconception paternal alcohol exposure on epigenetic remodeling of the h19 and rasgrf1 imprinting control regions in mouse offspring. Front Genet. 2012;3:10. https://doi.org/10.3389/fgene.2012.00010.
Liang F, Diao L, Liu J, et al. Paternal ethanol exposure and behavioral abnormities in offspring: associated alterations in imprinted gene methylation. Neuropharmacology. 2014;81:126–33. https://doi.org/10.1016/j.neuropharm.2014.01.025.
Sánchez MC, Alvarez Sedó C, Chaufan GR, et al. In vitro effects of endosulfan-based insecticides on mammalian sperm. Toxicol Res (Camb). 2017;7(1):117–26. https://doi.org/10.1039/c7tx00251c.
Sánchez MC, Fontana VA, Galotto C, et al. Murine sperm capacitation, oocyte penetration and decondensation following moderate alcohol intake. Reproduction. 2018;155(6):529–41. https://doi.org/10.1530/REP-17-0507.
Zindy F, den Besten W, Chen B, et al. Control of spermatogenesis in mice by the cyclin D-dependent kinase inhibitors p18(Ink4c) and p19(Ink4d). Mol Cell Biol. 2001;21(9):3244–55. https://doi.org/10.1128/MCB.21.9.3244-3255.2001.
Fraser LR, Drury LM. The relationship between sperm concentration and fertilization in vitro of mouse eggs. Biol Reprod. 1975;13(5):513–8. https://doi.org/10.1095/biolreprod13.5.513.
Kyjovska ZO, Boisen AMZ, Jackson P, et al. Daily sperm production: application in studies of prenatal exposure to nanoparticles in mice. Reprod Toxicol. 2013;36:88–97. https://doi.org/10.1016/j.reprotox.2012.12.005.
Nanjappa MK, Hess RA, Medrano TI, et al. Membrane-localized estrogen receptor 1 is required for normal male reproductive development and function in mice. Endocrinology. 2016;157(7):2909–19. https://doi.org/10.1210/en.2016-1085.
Sanchez MC, Sedo CA, Julianelli VL, et al. Dermatan sulfate synergizes with heparin in murine sperm chromatin decondensation. Syst Biol Reprod Med. 2013;59(2):82–90. https://doi.org/10.3109/19396368.2012.756952.
Fontana V, Choren V, Vauthay L, et al. Exogenous interferon-gamma alters murine inner cell mass and trophoblast development. Effect on the expression of ErbB1, ErbB4 and heparan sulfate proteoglycan (perlecan). Reproduction. 2004;128(6):717–25. https://doi.org/10.1530/rep.1.00335F.
Enders AC, Chávez DJ Schlafke S. Comparison of implantation in utero and in vitro. In: Glasser S.R., Bullock D.W, editors. Cellular and molecular aspects of implantation. Springer, Boston, MA; 1981. https://doi.org/10.1007/978-1-4613-3180-3_29
Salamone G, Giordano M, Trevani AS, et al. Promotion of neutrophil apoptosis by TNF-alpha. J Immunol. 2001;166(5):3476–83. https://doi.org/10.4049/jimmunol.166.5.3476.
Condorelli RA, Calogero AE, Vicari E, et al. Chronic consumption of alcohol and sperm parameters: our experience and the main evidences. Andrologia. 2015;47(4):368–79. https://doi.org/10.1111/and.12284.
Aitken RJ, Gordon E, Harkiss D, et al. Relative impact of oxidative stress on the functional competence and genomic integrity of human spermatozoa. Biol Reprod. 1998;59(5):1037–46. https://doi.org/10.1095/biolreprod59.5.1037.
Aitken RJ, Curry BJ. Redox regulation of human sperm function: from the physiological control of sperm capacitation to the etiology of infertility and DNA damage in the germ line. Antioxid Redox Signal. 2011;14(3):367–81. https://doi.org/10.1089/ars.2010.3186.
Aitken RJ. Not every sperm is sacred; a perspective on male infertility. Mol Hum Reprod. 2018;24(6):287–98. https://doi.org/10.1093/molehr/gay010.
Harikrishnan R, Abhilash PA, Syam Das S, et al. Protective effect ascorbic acid against ethanol-induced reproductive toxicity in male guinea pigs. Br J Nutr. 2013;110(4):689–98. https://doi.org/10.1017/S0007114512005739.
Maneesh M, Dutta S, Chakrabarti A, et al. Alcohol abuse-duration dependent decrease in plasma testosterone and antioxidants in males. Indian J Physiol Pharmacol. 2006;50(3):291–6.
Kuladip J, Prabhat KS, Dipak KD. Nicotine diminishes testicular gametogenesis, steroidogenesis, and steroidogenic acute regulatory protein expression in adult albino rats: possible influence on pituitary gonadotropins and alteration of testicular antioxidant status. Toxicol Sci. 2010;116(2):647–59. https://doi.org/10.1093/toxsci/kfq149.
Jalili C, Salahshoor MR, Naseri A. Protective effect of Urtica dioica L against nicotine-induced damage on sperm parameters, testosterone and testis tissue in mice. Iran J Reprod Med. 2014;12(6):401–8.
Russell LD, Sinhá- Hikim AP, Ettlin RA, et al. Evaluation of the testis: histological and histopathological. 1ed. Cache River Press, 1990.
Rocha NR, Braz JKFDS, de Souza SRG, et al. Testicular morphometry of rats with Walker 256 tumor supplemented with L-glutamine. Anim Reprod. 2021;18(2):e20200051 https://doi.org/10.1590/1984-3143-AR2020-0051
Veron GL, Tissera AD, Bello R, et al. Impact of age, clinical conditions, and lifestyle on routine semen parameters and sperm kinematics. Fertility & Sterility 2018;110 68–75.e4 https://doi.org/10.1016/j.fertnstert.2018.03.016.
Shi L, Wu J. Epigenetic regulation in mammalian preimplantation embryo development. Reprod Biol Endocrinol. 2009;7:59. Published 2009 Jun 5. https://doi.org/10.1186/1477-7827-7-59
Brykczynska U, Hisano M, Erkek S, et al. Repressive and active histone methylation mark distinct promoters in human and mouse spermatozoa. Nat Struct Mol Biol. 2010;17(6):679–87. https://doi.org/10.1038/nsmb.1821.
Carrell DT, Hammoud SS. The human sperm epigenome and its potential role in embryonic development. Mol Hum Reprod. 2010;16(1):37–47. https://doi.org/10.1093/molehr/gap090.
Boissonnas CC, Jouannet P, Jammes H. Epigenetic disorders and male subfertility. Fertil Steril. 2013;99(3):624–31. https://doi.org/10.1016/j.fertnstert.2013.01.124.
Jung YH, Sauria MEG, Lyu X, et al. Chromatin states in mouse sperm correlate with embryonic and adult regulatory landscapes. Cell Rep. 2017;18(6):1366–82. https://doi.org/10.1016/j.celrep.2017.01.034.
Krejčí J, Stixová L, Pagáčová E, et al. Post-translational modifications of histones in human sperm. J Cell Biochem. 2015;116(10):2195–209. https://doi.org/10.1002/jcb.25170.
Bernstein BE, Humphrey EL, Erlich RL, et al. Methylation of histone H3 Lys 4 in coding regions of active genes. Proc Natl Acad Sci U S A. 2002;99(13):8695–700. https://doi.org/10.1073/pnas.082249499.
Samson M, Jow MM, Wong CC, et al. The specification and global reprogramming of histone epigenetic marks during gamete formation and early embryo development in C. elegans. PLoS Genet. 2014;10(10):e1004588. https://doi.org/10.1371/journal.pgen.1004588.
Latham KE, Schultz RM. Embryonic genome activation. Front Biosci. 2001;6:D748–59. https://doi.org/10.2741/latham.
Jansen R, Mortimer D. Gardner’s system for grading human blastocysts. Adapted from: Gardner and Schoolcraft, 1999a. In vitro culture of human blastocysts. Toward Reproductive Certainty: Fertility and Genetics Beyond. London: Parthenon. 1999;378–388
Machtinger R, Racowsky C. Morphological systems of human embryo assessment and clinical evidence. Reprod Biomed Online. 2013;26(3):210–21. https://doi.org/10.1016/j.rbmo.2012.10.021.
Kalisch-Smith JI, Steane SE, Simmons DG, et al. Periconceptional alcohol exposure causes female-specific perturbations to trophoblast differentiation and placental formation in the rat. Development. 2019;146(11):dev172205. https://doi.org/10.1242/dev.172205.
Pérez-Tito L, Bevilacqua E, Cebral E. Peri-implantational in vivo and in vitro embryo-trophoblast development after perigestational alcohol exposure in the CD-1 mouse. Drug Chem Toxicol. 2014;37(2):184–97. https://doi.org/10.3109/01480545.2013.834358.
McReight EK, Liew SH, Steane SE, et al. Moderate episodic prenatal alcohol does not impact female offspring fertility in rats. Reproduction. 2020;159(5):615–26. https://doi.org/10.1530/REP-20-0039.
Chang RC, Skiles WM, Chronister SS, et al. DNA methylation-independent growth restriction and altered development programming in a mouse model of preconception male alcohol exposure. Epigenetics. 2017;12(10):841–53. https://doi.org/10.1080/15592294.2017.1363952.
Bedi Y, Chang RC, Gibbs R, et al. Alterations in sperm-inherited noncoding RNAs associate with late-term fetal growth restriction induced by preconception paternal alcohol use. Reprod Toxicol. 2019;87:11–20. https://doi.org/10.1016/j.reprotox.2019.04.006.
Chang RC, Wang H, Bedi Y, et al. Preconception paternal alcohol exposure exerts sex-specific effects on offspring growth and long-term metabolic programming. Epigenetics Chromatin. 2019;12(1):9. https://doi.org/10.1186/s13072-019-0254-0.
Govorko D, Bekdash RA, Zhang C, et al. Male germline transmits fetal alcohol adverse effect o hypothalamic proopiomelanocortin gene across generations. Biol Psychiatry. 2012;72(5):378–88. https://doi.org/10.1016/j.biopsych.2012.04.006.
Rompala GR, Simons A, Kihle B, et al. Paternal preconception chronic variable stress confers attenuated ethanol drinking behavior selectively to male offspring in a pre-stress environment dependent manner. Front Behav Neurosci. 2018;12:257. https://doi.org/10.3389/fnbeh.2018.00257.
van der Heijden GW, Derijck AA, Ramos L, et al. Transmission of modified nucleosomes from the mouse male germline to the zygote and subsequent remodeling of paternal chromatin. Dev Biol. 2006;298(2):458–69. https://doi.org/10.1016/j.ydbio.2006.06.05.
Okada Y, Scott G, Ray M, et al. Histone demethylase JHDM2A is critical for Tnp1 and Prm1 transcription and spermatogenesis. Nature. 2007;450:119–23. https://doi.org/10.1038/nature06236.
Capra E, Lazzari B, Turri F, et al. Epigenetic analysis of high and low motile sperm populations reveals methylation variation in satellite regions within the pericentromeric position and in genes functionally related to sperm DNA organization and maintenance in Bos taurus. BMC Genomics. 2019;20(1):940. https://doi.org/10.1186/s12864-019-6317-6.
Ge S, Zhao P, Liu X, et al. Necessity to evaluate epigenetic quality of the sperm for assisted reproductive technology. Reprod Sci. 2019;26(3):315–22. https://doi.org/10.1177/1933719118808907.
Gaydos LJ, Wang W, Strome S. Gene repression. H3K27me and PRC2 transmit a memory of repression across generations and during development. Science. 2014;345(6203):1515–1518. https://doi.org/10.1126/science.1255023
Paradowska AS, Miller D, Spiess AN, et al. Genome wide identification of promoter binding sites for H4K12ac in human sperm and its relevance for early embryonic development. Epigenetics. 2012;7(9):1057–70. https://doi.org/10.4161/epi.21556.
Vieweg M, Dvorakova-Hortova K, Dudkova B, et al. Methylation analysis of histone H4K12ac-associated promoters in sperm of healthy donors and subfertile patients. Clin Epigenetics. 2015;7(1):31. https://doi.org/10.1186/s13148-015-0058-4.
Acknowledgements
The authors wish to acknowledge Dr. Lucrecia Piñeiro for helping us with statistical interpretation of the data and technician Zaira Naguila for her collaboration and support in handling animals, as well as all the staff of the Central Bioterio of the University of Buenos Aires.
Funding
This work was supported by a grant from Fundación Honorio Bigand, Buenos Aires, Argentina. MYC and LG are doctoral fellows, CONICET, Argentina.
Author information
Authors and Affiliations
Contributions
MYC performed experiments, analyzed data, and wrote the paper. LG performed experiments and analyzed data. MGS was involved in animal care and treatment and language correction. SB involved in animal care and treatment. GS performed cell death experiments. MR analyzed data and corrected the paper. JCC supervised the study and corrected the paper. VAF conceived the study and wrote the paper.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the CICUAL (Comisión Institucional de Cuidado y Uso de Animales de Laboratorio) of FCEN-UBA (Protocol Number 56/2016).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cambiasso, M.Y., Gotfryd, L., Stinson, M.G. et al. Paternal alcohol consumption has intergenerational consequences in male offspring. J Assist Reprod Genet 39, 441–459 (2022). https://doi.org/10.1007/s10815-021-02373-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02373-0